Playlist
Show Playlist
Hide Playlist
Hypovolemic Shock
-
Slides Pulmonary Critical Care Respiratory Pathology.pdf
-
Download Lecture Overview
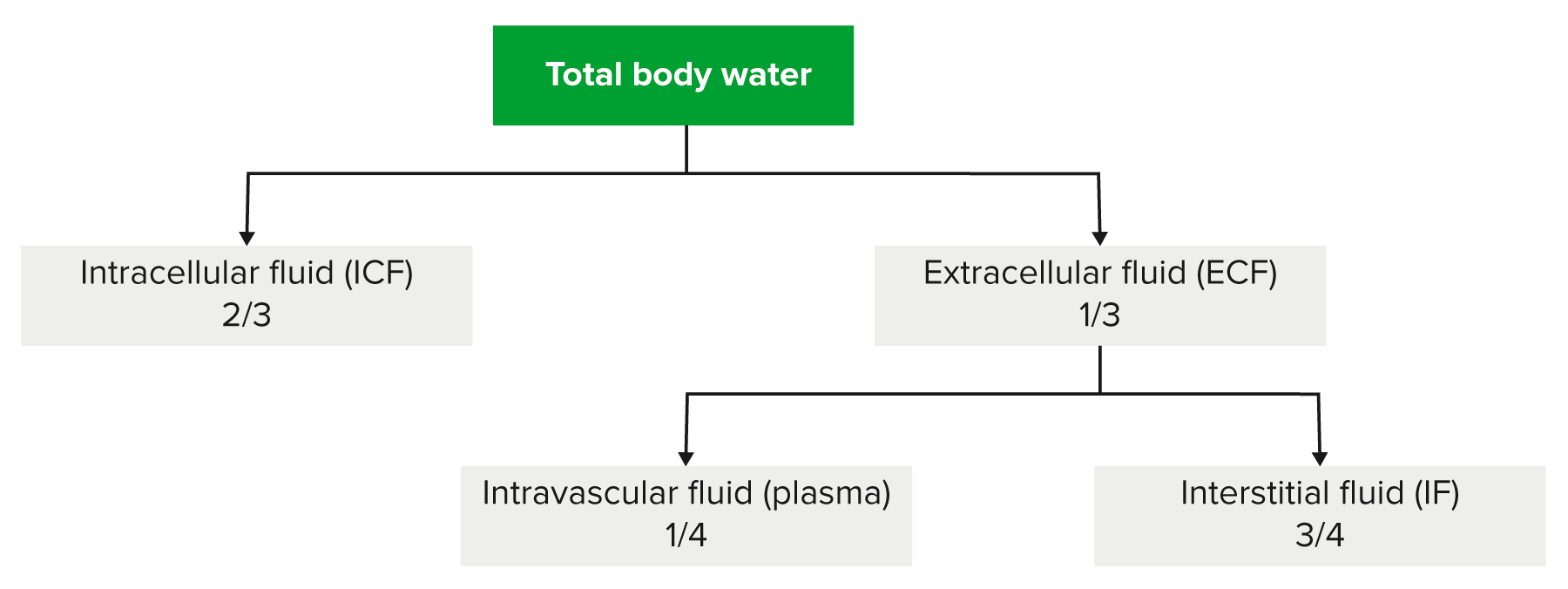
00:01 Ladies and gentlemen, we’ll take a look at Critical Care in Pulmonology. I do need you to pay attention to this lecture series. It will integrate many of the systems that we have discussed and put it into a table format in which, for example, if your patient comes in with lack of proper oxygenation of his or her tissues, well, what kind of signs and symptoms are you going to be looking for? We begin our discussion by looking at this table and on the first column, we have our ‘Shocks’ that we will walk through and then everything to the right of this that you see in the table, are going to be signs and symptoms and also the measurements and tests that are going to be relevant for the type of shock that the patient is unfortunately experiencing. 00:55 Welcome to Critical Care. The first type of shock, now, in general, when you think about shock, it’s a fact that the tissue is not being properly oxygenated for whatever reason. And we will go through many types of shocks, but ultimately please understand whatever that the pathogenesis was, the tissue was what was suffering the consequences. The first instance, well, we have Hypovolemic. What does that mean? Well earlier, when we had discussed Nephrology and we were talking about two major wheels of control or cycles of control. One was dealing with control of osmolarity, the other one was dealing with the wheel or cycle of volume. Do you remember that? If not, then it will be a good time for you to take a look at those two cycles where we were monitoring osmolarity and if it’s physiologically monitoring, then it is ADH, as you know, that would be measuring osmolarity. Are you clear? Whereas if it is volume, then it would be Aldosterone and company, your RAAS System, that would then be controlling or monitoring and regulating your volume. Okay. Every once in a while, if there’s such massive volume loss where the patient is losing greater than 10% of his or her volume, maybe massive haemorrhage. Then what cycle or which component of regulation will then be sacrificed? It will be the osmolarity because volume becomes of utmost priority and we discussed that when we had walked through the regulation of ADH and Aldosterone on osmolarity and volume respectively. It is imperative that you have that foundation in your head firmly implanted before you take a look at Hypovolemic. 02:47 The other big concept that you need to take away from Physiology would also be your method of reflex and how the body is desperately trying to do what? Well, Hypovolemic, you’ve lost your blood quite a bit. Let's go ahead and call this greater than 10%. So, now, at this point, you’re obviously going to release your RAAS System in desperation. 03:10 You’ll have your Angiotensin II. The Angiotensin II will do it. 03:14 Then do that crossover that I was referring to. Remember the volume becomes of utmost priority. And what about your blood pressure in this patient of Hypovolemia? Good, decreased. 03:26 Let’s go back to that reflex now. So, there are a couple of things occurring simultaneously. 03:32 The first thing would be the reflex, then followed by the hormone response, right, in that order. Reflex is extremely quick and the reflex that I’m referring to here would then be the baroreceptor reflex, isn’t it? So, if your patient comes in, presents with, number 1, decreased blood pressure. Next, as soon as that occurs, then where is your blood? Oh, my goodness! It’s on the floor. Pick it up. No, you can’t. It doesn’t work like that. So, there it is on the floor and there isn’t much blood in your blood vessels. So, tell me about that stretch, decreased. Now, before we move on, you tell me, close your eyes. What kind of outflow would you want from your autonomic nervous system so that you could then compensate for the decreased blood pressure? Good. You want the sympathetic nervous system, don’t you? So therefore, you have decreased stretch and you tell me, are you referring to a sinus or a body here? Baroreceptors are in sinuses. 04:27 Good. Next step, which sinus are you referring to? Carotid or aortic? Good. Carotid is more sensitive. Next step. Which cranial nerve is it? Nine or ten? Glossopharyngeal, nine. So far so good. So, you have decreased stretch, glossopharyngeal, decreased firing, and the medulla is going to then increase outflow of sympathetic. How can you confirm that in your patient? I want you to take a look at the column where it says ‘Diagnosis’. 04:54 So, the patient now comes in with decreased blood pressure. Sympathetic nervous system is doing everything in its power to do what? Vasoconstrict. If you vasoconstrict your cutaneous blood vessels, then how does your skin then feel? Cold, clammy. Does that make sense? So, you put all this together here, didn’t you? Okay, so hypovolemia – haemorrhage, dehydration, 3rd spacing. Do not memorise that, understand it. Here, once again, go back to your basic concepts of Physiology where you know that you have excuse me, you have two compartments physiologically for total body water. The two major components are or compartments are ICF, two-thirds, ECF, one-third. What if you pathologically now introduced a third compartment? What do you mean? There should never be one, right? So, let’s say, there is burns or pancreatitis. This would then mean there’s fluid leakage into a third compartment, perhaps excessively. And so therefore, could this result in Hypovolemia? Sure. Would you have a decrease in blood pressure? Absolutely. What happens to your stretch? Decreased. Increased sympathetic and you have cold and clammy. Okay. Those two down, let’s go into this concept of preload. Okay, where’s all the blood? Oh, my goodness! It’s on the floor. Okay. If all this blood is on the floor and it’s not in your system, tell me how full is your heart? Not very full. You understand the concept? So, preload, we can safely say, is decreased in Hypovolemic shock. Next, well, how would you go about measuring the preload in your heart? If it’s the left side, you’d be using your PCWP, pulmonary capillary wedge pressure, and if it’s the right side, maybe perhaps your central venous pressure. Point is, if your blood is on the floor, you don’t have much of it in the heart, you’ll have decreased preload. Is that understood? Next, well, what about that cardiac output? Once again, it’s not in the heart, decreased cardiac output. Now, what about your sympathetic nervous system? We said that it is causing vasoconstriction. What will then happen to your systemic vascular resistance? In other words, TPR is what we’re looking at there, in that second to last column. Identify it. 07:16 And if your TPR increases, another way of saying this, please know, clinically is, systemic vascular resistance and with this type of vasoconstriction, you are then affecting preload or afterload? Afterload. And what will happen here? Increased. Clear? What's your treatment right off the bat? Patient comes in with Hypovolemia of such a dramatic fashion, IV fluids. What might you want to give that’s cheap and easy? Crystalloids or colloids? Crystalloid. And this being something like normal saline, 0.9% saline. You see as to how this table is integrating everything that we’ve talked about. So, as you go through here with critical care in Pulmonology, understand the entire system is being affected.
About the Lecture
The lecture Hypovolemic Shock by Carlo Raj, MD is from the course Pulmonary Critical Care.
Included Quiz Questions
Which of the following is part of the compensatory response to hypovolemia?
- Activation of the renin-angiotensin-aldosterone system
- Activation of the parasympathetic nervous system
- Inhibition of antidiuretic hormone secretion
- Increased firing rate of the baroreceptors in the carotid sinuses
- Increased release of atrial natriuretic peptide
Which of the following clinical manifestations is present in patients with hypovolemic shock?
- Cold extremities
- High blood pressure
- Neck vein engorgement
- Lower limb edema
- Increased urine output
Which of the following hemodynamic parameters is elevated in patients with hypovolemic shock?
- Systemic vascular resistance
- Left atrial pressure
- Cardiac output
- Pulmonary capillary wedge pressure
- Mixed venous oxygen saturation
Which of the following is the best option for the management of hypovolemic shock?
- Intravenous crystalloid fluids
- Inotropic agents, such as dopamine
- Nitroglycerin plus aspirin
- Broad-spectrum antibiotics
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |