Playlist
Show Playlist
Hide Playlist
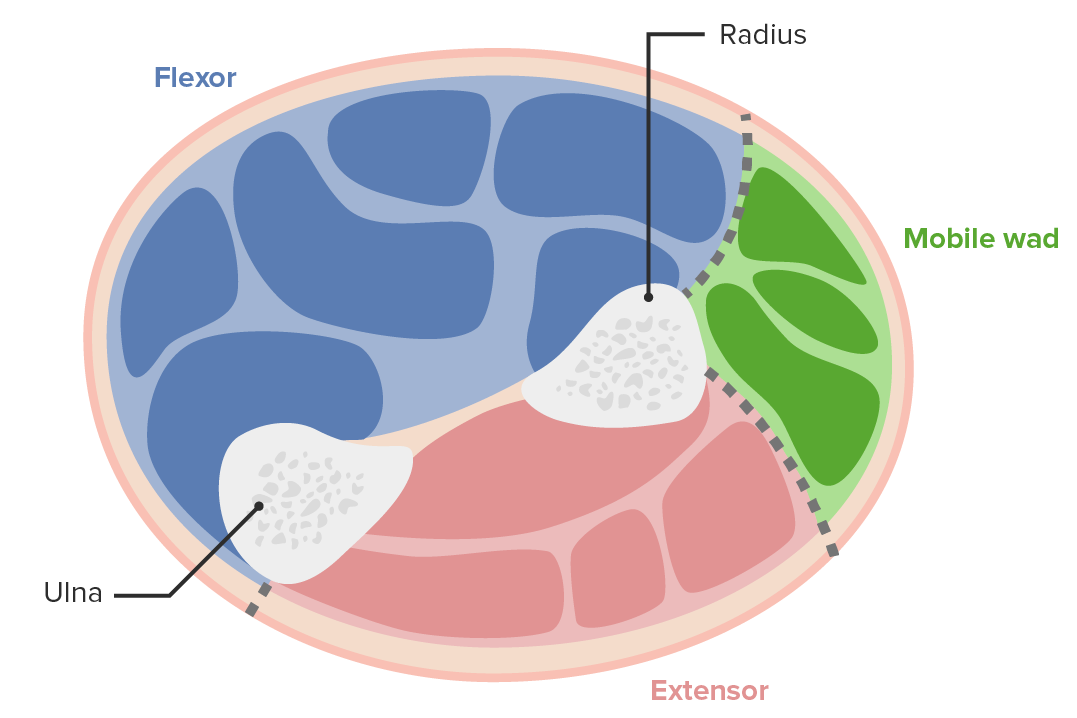
Compartment Syndrome
00:01 Compartment Syndrome, definition. 00:04 There are few things they will ask you in the exam. 00:08 The wordings they've been looking for is micro circulation is affected not the micro circulation. 00:16 Then myoneural necrosis, osseo-fascial compartment. 00:20 So these are the things they will be asking you. 00:25 In compartment syndrome, what is an increase in the interstitial fluid, within the fascial compartment, between the bone and the fascia? Needs to compromise of the micro circulation. 00:35 So what they are trying to get is you can have a normal peripheral pulse and the patient can have a compartment syndrome. 00:41 Okay, so just because somebody has got peripheral pulse doesn't mean they haven't got. 00:46 Yeah. 00:49 Absolutely, you're right, this is only for the limbs, absolutely, limbs, also a fascial compartment. 00:53 Yeah. 00:54 Have you been asked to abdominal compartment syndrome part A? I don't think, no, Part B has been asked, but not in Part A. 01:01 Part A is, certain things don't happen. 01:06 Part A, you get the compartment syndrome in the limbs, and usually there are still lower limb. 01:11 Very rarely the upper limb bone in the hand. 01:15 It's exactly the same principle except that there is no bone. 01:24 Pain, patient has been shocked as well. 01:27 Yeah, because... 01:33 Have you seen many? Have you seen any? No, it hasn't been asked in the exam but having said that they can... the principle is the same for compartment syndrome. 01:53 Causes... 01:56 this other ones. 01:57 Of which the first two are the most important one, fracture. 02:02 Trauma, bleeding. 02:04 Although others are... 02:07 or some of there recognized causes of compartment syndrome. 02:15 Escharotomy, escharotomy, will do that when you do burns. 02:20 No, that's okay. 02:22 What's the first symptom? Pain. 02:24 Next? Okay, pain on passage to the affected compartment, that's your first one. 02:33 And then you can paraesthesia, this is an order. 02:35 This is a same 6 pieces you get in critically schemically but this is the order. 02:40 Sensory loss occurs before motor loss, that's a MCQ question. 02:44 And microvasculature is affected before the microvasculature. 02:47 So, you can paraesthesia first, before paralysis. 02:50 And you could pallor first before pulselessness. 03:03 Okay. 03:05 What's normal compartment pressure in the lower leg? Wow, that's too high normal pressure in you. 03:12 No, it's 0 to 5. 03:14 Yeah. 03:15 You know the... 03:17 32 second off. 03:19 Normal more pressure is 0 to 5, Compartment pressure in your exam, this is what I am going to clarify. 03:27 It is agreed that anything about 30 to 40, you consider releasing the compartment. 03:32 You think it's compartment syndrome. 03:34 How are the current guideline is a differential pressure. 03:37 So what that means is, if you have a patient who's in shock, who's got a diastolic blood pressure of... 03:48 40, so the blood pressure 70 over 40. 03:53 Instead of the normal 120/80, you can't let the compartment pressure rise to... 04:00 set 12 here, because the differential pressure between that is 28. 04:06 So in other words, the differential blood pressure between the diastolic pressure and your compartment pressure should not exceed 30. 04:16 So differential pressure. 04:17 So if we have a patient with a normal blood pressure, you can allow their compartment pressure to go up to 35. 04:23 Because your differential pressure is still 45. 04:26 The the rationale is that much pressure is sufficient to push the fluid through into the... push the food into the circulation. 04:37 Okay, so the differential pressure is what is important. 04:39 The differential pressure between the diastolic pressure and the compartment pressure shouldn't go less than 30. 04:49 So if this keeps on increasing or if this keeps on falling then that serious trouble. 04:55 Okay. 05:07 The compartment syndrome? No, even if you're associated... here, you mean? Well, tricky because let's say we put it to 90 or 50, but if this keeps on going up, what do you do? If this goes to 14, 15, 16, 17, 18, so this will maybe buy you some time but nothing more than that. 05:31 If the patient has got compartment syndrome, nowadays you don't even measure compartment pressure. 05:35 You just go in by on clinical suspicion. 05:39 But if you go by absolute value, then you have to go by those numbers. 05:44 Again the guidelines say you have to measure the compartment pressure before you release a compartment because the patient ends up with severe complication post fasciotomy, which will end up with an amputation later. 05:58 Then, the always a question is how do you know the patient had compartment syndrome? How did you decide? What was your objective finding? You can't say just I did a bit of (inaudible) and had I thought the patient compartment syndrome so that's why they suggest to measure it, just for our records.
About the Lecture
The lecture Compartment Syndrome by Stuart Enoch, PhD is from the course Trauma and Post-OP Management.
Customer reviews
2,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
too many interruptions in the video. Lots of people talk and you cant hear it.