Playlist
Show Playlist
Hide Playlist
Burns
-
Slides Burns Surgery.pdf
-
Download Lecture Overview
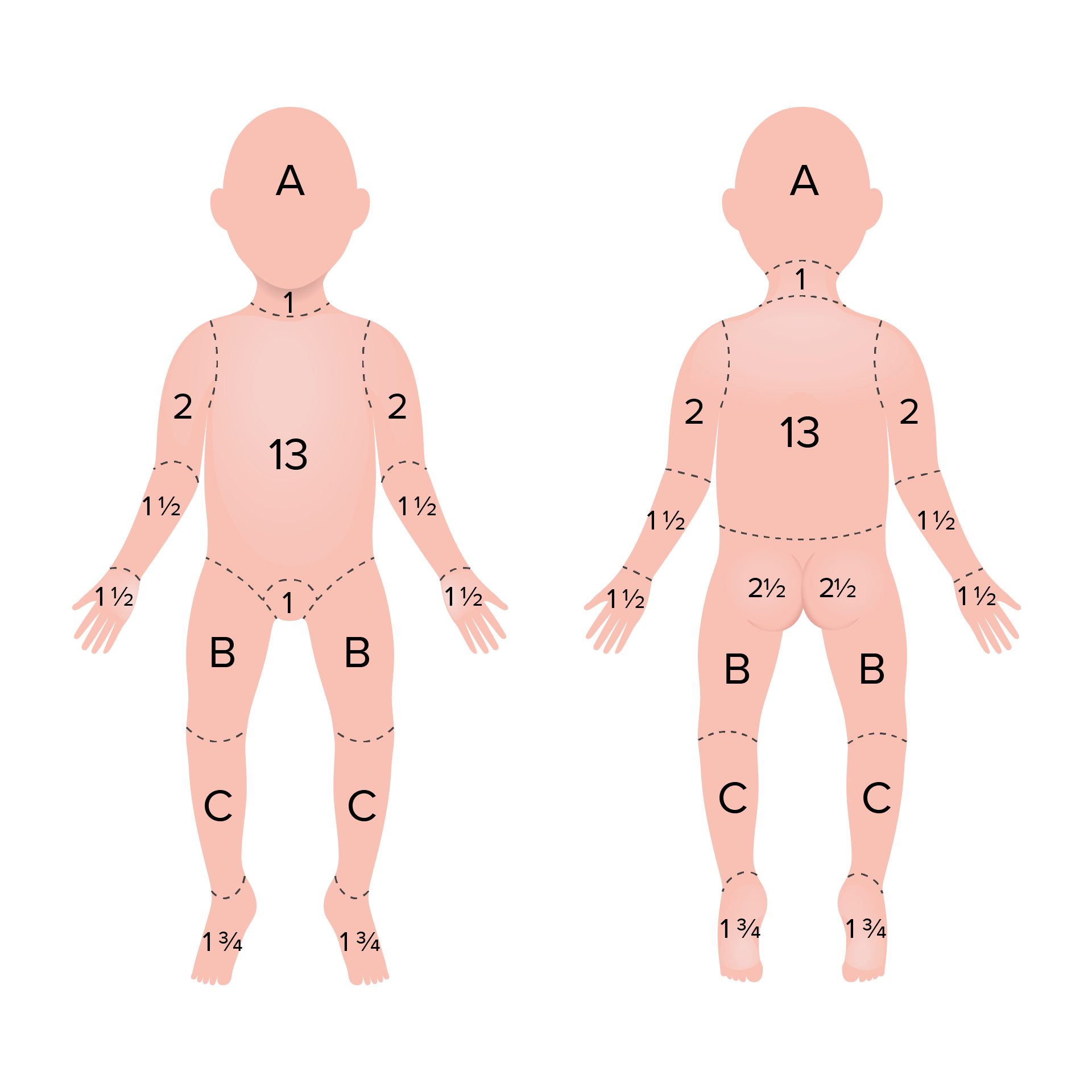
00:01 Thanks for joining me on this discussion of burns in the section of trauma. 00:05 Let’s start with the clinical scenario. 00:08 A 24-year-old man who was drinking and smoking at home at the same time unfortunately he fell asleep and the curtains in his apartment in the house set on fire. 00:18 His neighbors noticed the smoke and called the firefighters. 00:21 And this is what his house looked like. 00:24 What are you thinking? If you were to have received a call like this and this is what it looked on the scene, how would you think to prepare to receive this patient? What would your initial management plans be? What are your management priorities? I’ll give you a second to think about this. 00:46 That’s right, just like any other patient in trauma, it’s the ABCs or airway, breathing and circulation. 00:53 Of course, particularly for burn patients, airway and breathing are extremely important and very important for the initial management. 01:01 I'd like to pose another question to you. 01:04 What are some signs of inhalational injury? Remember, anybody who’s in a house fire or in the surrounding of smoke is at risk for inhalational injury and as a clinician it’s very important for you to have recognized the signs. 01:18 I’ll give you a second to think about the answer. 01:20 That’s correct, soot around the mouth or stridor. 01:25 If the patient is complaining about difficulty speaking or breathing, they may be late signs and you should achieve adequate airway. 01:33 This may be indication that the patient’s upper airway is edematous. 01:38 Now, let’s quickly review the rules of Nine. 01:43 There’s no point to remembering it. 01:44 Just remember that the body parts are divided both in the front and the back, as well as the extremities in the head into percentages multiples of 9%. 01:54 This gives you a rough estimate of how much percent body surface areas actually involved in the burn. 01:59 Which will be important when you try to calculate resuscitative fluid formulas. 02:05 Let's briefly discuss burn classifications. 02:07 First degree or superficial thickness burns typically appear red and dry. 02:12 They are very painful and are limited to the epidermis. 02:16 Second degree or superficial partial thickness burns appear at splotchy, painful blisters along with significant swelling. 02:24 It primarily affects the papillary region of the dermis. 02:28 Third degree or deep partial thickness burns appear as white or leathery skin. 02:34 These burns impact the reticular region of the dermis and are relatively painless. 02:40 Finally, fourth degree or full thickness burns results in a charred skin that is totally insensate. 02:48 It penetrates all subcutaneous tissue layers, including bone and can result in eschar formation. 02:55 Speaking of which, how do we resuscitate the patient? Well, it’s governed by Parkland’s Formula. 03:01 Parkland’s formula states that we shall resuscitate our burn patient with approximately 4cc of crystalloid fluid multiply their body weight in kg by the percent body surface area that you’ve estimated based on the rules of nine. 03:16 And how do we know the patient’s adequately resuscitated? Well, we titrate in to an adequate urine output as defined approximately 0.5 to 1cc per kg per hour of urine. 03:29 Now, let me change the scenario for you a little bit. 03:34 And give you something to think about. 03:36 Let’s say that you've evaluated a trauma patient, in this case a burn patient, and now the patient has been admitted to the surgical intensive care unit for monitoring. 03:45 The patient has been relatively stable the next few days but on the third day in the hospital, the ICU nurse calls you to the bedside and says the patient is hypotensive. 03:55 The patient is registering a blood pressure of 80/60. 03:58 What’s going on in your mind? What’s some possible differential diagnosis? I’ll give you a second to think about this. 04:07 That’s right. 04:09 The patient maybe septic from an infected wound particularly gram negative sepsis. 04:15 Remember, this is an important association and very high yield. 04:19 If the patient has a burn and becomes septic shock, make sure you start appropriate antibiotics. 04:27 Silver sulfadiazine and silver nitrate are effective broad-spectrum, antibacterial and antifungal agents that can be used topically on burns Next, patient also needs quick and adequate debridement of the soft tissue that may be infected. 04:44 Remember, you must culture the skin and the burned sites and treat with appropriate antibiotics. 04:49 But don’t over treat with antibiotics if there is no evidence of wound infection. 04:54 What if the patient becomes difficult to ventilate? For example, that same burn patient that you've evaluated in the trauma bay in the ICU is subsequently intubated but now the respiratory therapists tells you he’s got a high peak airway pressure and you are having a difficult time ventilating the patient. 05:11 What’s going on? I’ll give you a second to think about this. 05:16 Particularly with patients with circumferential thoracic burns. 05:24 The patient may be having ARDS, or adult respiratory distresss syndrome or potentially compartment syndrome of the thorax due to eschars. 05:33 How do we treat eschars in induced compartment syndrome? With an escharotomy. 05:41 I know this picture looks kind of gruesome and it looks like a very painful procedure. 05:46 Luckily for the patient, because of the full thickness burns causing that eschar, the escharotomy itself is actually not painful. 05:54 It’s very important to perform the escharotomy in a timely fashion to reduce the peak airway pressures and thoracic compartment syndrome. 06:02 Let me post another question to you. 06:05 What is a potential complication with long term burn wounds that are not healing? I’ll give you a second to think about this. 06:14 This is another high yield, important piece of information to remember. 06:17 That’s right! Marjolin’s ulcer. 06:20 Marjolin’s also a name for squamous cell cancer as the result of a burn wound. 06:26 And here you see a picture of a Marjolin’s ulcer. 06:29 Remember, excision is usually necessary and it usually takes place under an excisional biopsy, meaning it’s potentially diagnostic and therapeutic. 06:40 Now, it’s time to review some important clinical pearls and high yield information. 06:44 Remember, burn resuscitation is titrated to an adequate urine output. 06:49 So, the Parkland’s formula is just the starting place. 06:53 And remember, patient’s who sustained circumferential burns particularly of the thorax, maybe developing compartment syndrome from eschars and need an urgent release, this is called an escharotomy. 07:08 Thank you very much for joining me on this discussion of burns.
About the Lecture
The lecture Burns by Kevin Pei, MD is from the course Surgery: Trauma.
Included Quiz Questions
Which of the following is Parkland’s formula for burn resuscitation?
- 4 cc of fluid x weight (kg) x percent total body surface area of burned skin; administered over 24 hours
- 5 cc of fluid x weight (kg) x percent total body surface area of burned skin; administered over 48 hours
- 4 cc of fluid x weight (Ib) x percent total body surface area of intact skin; administered over 48 hours
- 6 cc of fluid x weight (kg) x percent total body surface area of intact skin; administered over 24 hours
- 4.5 cc of fluid x weight (Ib) x percent total body surface area burn; administered over 24 hours
What type of malignancy is a potential long-term complication of burn wounds?
- Squamous cell carcinoma
- Adenocarcinoma
- Basal cell carcinoma
- Lymphomas
- Ductal carcinoma in situ
Which of the following is the best objective measure for monitoring fluid resuscitation in patients with significant burns?
- Urine output
- Serum lactate
- Pulmonary artery occlusion pressure
- Central venous pressure
- Noninvasive blood pressure measurements
Customer reviews
4,3 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture, it has everything you need to know, very well explained, you can understand everything very fast with no doubt
Very well explained all the most important points. Would be nice to see more photos.
I would have loved to learn how the management of burns differs according to the SA affected. Moreover, a discussion on chemical and electrical burns would have also been fantastic