Playlist
Show Playlist
Hide Playlist
Derma Case: 71-year-old Woman with a Progressive Skin Rash
-
Slides Bullous Diseases.pdf
-
Download Lecture Overview
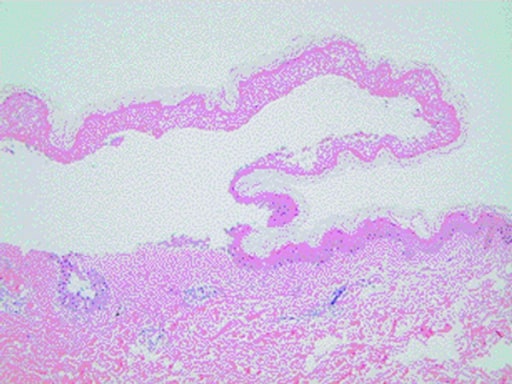
00:02 So the next thing we're going to talk about is bullous disorders. 00:05 Let's jump into a case. 00:07 This is a 71-year-old woman with a past medical history of obesity, who's presenting with progressive skin rash. 00:14 She reports she noted the development of itchy hives, randomly distributed over her body, several months ago. It seemed to wax and wane, leaving reddish patches on her skin. 00:26 5 days ago, she noticed a tense, fluid- filled blister on her right thigh that seemed to emerge from one of those red patches, followed by 2 similar lesions on her torso. 00:36 Now, she denies any lesions in her mouth, no fevers, no chills, no nausea. 00:41 She takes only atorvastatin and lisinopril, and denies taking any new medications. 00:47 Social History: non-smoker, she drinks a couple beers most days of the week. 00:52 Non-contributory family history, and on review of systems, no dyspnea, no eye symptoms, no joint pain. 00:59 So, highlighting a few key aspects that we think of when addressing a new case, the time course appears to be slowly progressive. We've been seeing these symptoms slowly evolve over several months. 01:11 The pattern of skin involvement seems kind of random. There's no particular predilection and it's not symmetric. 01:17 Skin inflammation does appear to be present with some developing blisters in different areas. 01:23 And there doesn't appear to be any evidence of systemic involvement at this time, based on a pretty negative review of systems. 01:32 Physical exam. She's got a temperature of 37.1°C, heart rate's 72, blood pressure 135/71. 01:40 Head and neck exam: normal conjunctiva, no lymphadenopathy, no oropharyngeal lesions. 01:46 And then on the skin exam, we see scattered, non-tender, erythematous, eczematous patches in both sun-exposed and unexposed areas. There are numerous tense bullae, 1-3 cm in size, on her torso and on her extremities, containing either serous or hemorrhagic fluid. 02:05 Some of those bullae are emerging from erythematous patches. Others are emerging de novo, from normal skin. 02:12 And just a slight rubbing of the affected skin does not lead to any exfoliation. 02:17 I think we'll learn about the significance of that in a little bit. 02:20 And no evidence of significant edema. 02:22 The picture shown here is not a picture of our patient, but a representative photo of what we're looking at. 02:30 So, based on the information we have thus far, which of the following is the most likely diagnosis? Let's take a look at each one. 02:38 So, Stevens-Johnson syndrome. Now, Stevens-Johnson syndrome, we know that half of the time, 50% of cases are not related to drug exposure, and they're either idiopathic or they might be related to some prior antecedent infection, most commonly, mycoplasma or potentially, HSV. 02:56 Stevens-Johnson syndrome is characterized by lesions that may initially include erythematous patches, as we're seeing in our case. And it really lies on a spectrum from Stevens-Johnson syndrome up to toxic epidermal necrolysis. 03:10 So it's something to still keep on our list, for sure, even though we're not getting a story of any new medications and no obvious prior infections. 03:18 Porphyria cutanea tarda. There are a number of different porphyrias that are out there. 03:23 This is the one that has the most common skin manifestations. 03:26 It is a skin disease associated with adulthood. 03:30 And it's essentially caused by a disruption of the normal heme biosynthesis pathways. And that's the same for all the porphyrias, depending upon where the disruption and the heme biosynthesis pathway occurs, that's when you're going to get a different phenotype of porphyria, whether it's variegete porphyria or acute intermittent porphyria or, in this case, PCT. 03:50 Importantly, it is characterized by the gradual progression of pruritus with vesicles and bullae, but it really tends to occur in sun-exposed areas, because it's the intersection between sun exposure and these toxic porphyric proteins that lead to the manifestations of disease. 04:09 We're not really getting much of that in this case, but we'll keep it on the list for now. Next up, bullous pemphigoid. 04:16 It does affect the elderly. Our patient is in her 70s It does cause tense bullae, and we'll talk about why in a moment. 04:24 And so, I think we'll need to keep that one on our list. 04:27 Pemphigus vulgaris. This is a potentially very severe disease process that can have significant consequences. 04:34 It's often associated with significant mucosal involvement. 04:38 Our patient, at the moment, is not appearing to have any mucosal involvement, but we'll keep that one on the list, nonetheless. 04:44 We have to make sure we rule it out. 04:46 And then staphylococcal scalded skin syndrome is definitely characterized by diffuse, ill-defined, erythematous patches, as was the case in our patient. 04:55 And then they can progress to extensive epidermolysis or sloughing of skin, and bullae, though there is something about staphylococcal scalded skin syndrome, that just doesn't seem appropriate for our case. 05:06 We'll have to come back to that one. Let's highlight a few key points here. 05:12 So, this is clearly a 71-year old-woman. And when we think about something like bullous pemphigoid, which is perhaps right now the highest thing on my list, it is a disease of the elderly, is really an equal male to female predominance there. 05:28 There is, oftentimes, with bullous pemphigoid, a prodrome of pruritic hives, some papules, some eczematous patches, which can be present for months before you even see any of those bullous lesions occur. And that is something that we're getting from our patient. 05:45 Thirdly, one of the characteristic features of bullous pemphigoid, in contrast, to say, pemphigus vulgaris, is the absence of mucosal involvement. 05:54 It can occur, but it's much less likely to be seen with bullous pemphigoid. 05:59 Fourth, no fevers, chills, or nausea. That's also typical of bullous pemphigoid. 06:04 Some of those other things on our list, very frequently, have systemic involvement, but constitutional symptoms and things like that would not be a part of bullous pemphigoid. 06:12 So all these factors are really steering us towards that diagnosis. 06:16 Likewise, in terms of our head neck exam, normal conjunctiva, no oropharyngeal lesions, further supports the idea that the mucosa are not typically involved. The lesions are non-tender, which would also suggest a less inflammation, kind of, process. 06:32 Sun-exposed and unexposed areas, again, that's going to steer us away from porphyria cutanea tarda, which you'd really only see in sun-exposed areas. 06:42 The fact that the bullae are tense, this is a very, very important point in this case. We'll come to why in a moment, but it has to do with where the defect is occurring, in terms of the skin layers. At this point, with tense bullae, we know that the epidermis, which is outside of the dermis, appears to be intact, and we'll talk more about that in a second. 07:04 And there's this classic test that I was alluding to before. 07:07 When you rub the affected skin and it does not separate, you're not immediately separating the dermis from the epidermis, or separating the epidermis itself, that's called a negative Nikolsky sign. 07:18 And the Nikolsky sign can be something that can help us steer us towards one disease or another, and we'll talk about that as we go through this conversation. 07:29 So, with all that information in mind, it looks like we're looking at bullous pemphigoid.
About the Lecture
The lecture Derma Case: 71-year-old Woman with a Progressive Skin Rash by Stephen Holt, MD, MS is from the course Allergic and Immune-mediated Skin Disorders.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |