Playlist
Show Playlist
Hide Playlist
Thyroid Hormone Function
-
Slides ThyroidFunction EndocrinePathology.pdf
-
Download Lecture Overview
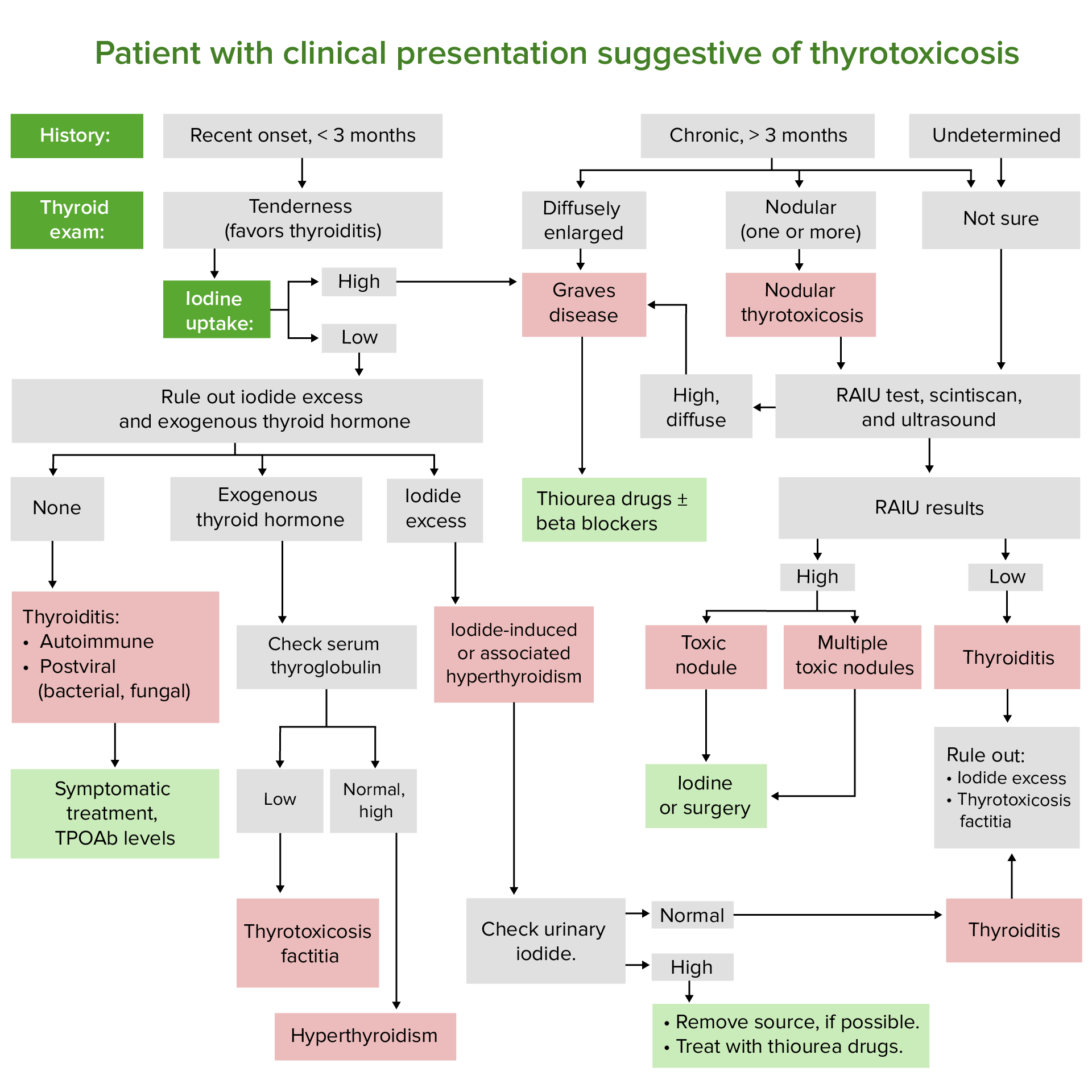
00:01 With this discussion of integrated thyroid hormone functioning, first it’s important for us to map out this illustration. 00:09 Begin by looking at the blood side, the blood side would be the basolateral membrane. 00:13 In the basolateral membrane, you have a symport, but moving in the same direction. 00:19 The two elements moving in would be sodium and iodide… symport. 00:24 The numbers here will then correspond with the explanations that are upcoming, but it is first imperative that you have a good picture in your head of what quickly an integrated thyroid hormone synthesis would look like. 00:40 Once you get to iodide and sodium inside your follicular epithelial cell, which is the middle portion, with the help of, what’s the receptor that you would have here on your thyroid gland, the TSH receptor, which is acted upon by TSH or that receptor could be pathologically be stimulated by TSI, thyroid stimulating immunoglobulin. 01:04 Next, once you have the iodide inside, then you have a very important enzyme that you would be paying attention to, go ahead and skip over to number three and four. 01:13 I’m not going to walk you through in great detail the physiology. 01:16 It’s important that you are able to locate a very important enzyme that’s critical for thyroid hormone synthesis and that being your peroxidase and that has a number of key functions or responsible for key steps in thyroid hormone synthesis. 01:34 There are drugs here that would inhibit that enzyme and we have pathologies such as Hashimoto in which you might have antibodies that are attacking your peroxidase therefore rendering your thyroid hormone synthesis null and void. 01:53 On a sad note, I’d like for you to take a look at the follicular epithelial cell and pay attention to now here a very important binding globulin of your thyroid hormone; locally, it’s not delivered obviously… the thyroglobulin. 02:08 And the thyroglobulin has important functioning as we shall see critically and what you will be responsible for in terms of clinical significance. 02:18 Now that you have your thyroglobulin and the help of peroxidase and you have the proper form of iodine, then you will then bind your DIT and MIT, you combine your DTI/MIT to form your T3 and your DIT and DIT would then form your T4… where are you? You are in your colloid in other words the follicular lumen and what does this look like histologically? Histologically, we showed you that homogenous, eosinophilic, pink like area in the middle of your thyroid cell responsible for storing your thyroid hormone. 03:00 When is time for you to recruit your thyroid hormones? You’ll notice that your thyroglobulin and your MIT and DIT will be brought back into the follicular epithelial cells and then you have certain deiodinases and every once in a while you get a question in terms of… you can have patients that are actually deficient of that deiodinase and if you’re deficient of that deiodinase now this would be centrally acting by that I mean, working in the thyroid gland, but then you also have peripherally acting deiodinases that is critical to convert your T4 into T3. 03:37 And if you’re deficient of that enzyme for all intent and purposes you don’t have proper functioning thyroid hormone so your patient is presenting as hypothyroidism. 03:49 Keep that in mind, I’ll repeat that point one more time. 03:53 Into circulation, you have T4 with much greater ratio being released than T3. 04:01 Overall picture of your integrated thyroid hormone functioning, this is the picture that you want to have in mind as we now go through the explanations. 04:09 Number one, you’ll pay attention to TG; TG is a thyroglobulin; clinical significance… oh, yes. 04:17 On biopsy provides proof of thyroid origin of the tissue… number one. 04:22 What kind of tissue? Thyroid tissue, do not confuse this with thyroid binding globulin which came from where? Liver. 04:30 This is thyroglobulin, where are you? Thyroid tissue, period. 04:34 Next, what about the significance? Three important determinants: number one, the mass of thyroid tissue present; thyroglobulin will actually tell you, “Well, how much of my thyroid tissue is actually responsible for that particular pathology?” Next, the presence of injury to the thyroid, for example, you wish to further examine or investigate a cold nodule within the thyroid gland; a cold nodule to you especially in a young male is going to be incredibly concerning because you’re worried about? Good, thyroid cancer. 05:09 By far, the most common will be papillary cancer of the thyroid gland and you then perform an FNA, fine needle aspiration and then clinically, you then measure the thyroglobulin to see as to, “Well, how much of my thyroid gland have I damaged?” What about radioactive iodine? RAI is radioactive iodine therapy, we’ll talk about this in great detail. 05:34 You’ll be using radioactive iodine for two purposes: number one, you’ll be using it for diagnostic purposes and then number two, you’ll be using it maybe perhaps to treat your patient with Graves’ disease; in other words, radio ablative therapy. 05:49 Now, granted there are two isotopes of that iodine radioactively in which you would then use it for either diagnostic or your therapeutic purposes, but you’re not responsible for the isotopes; don’t spend time memorizing the isotopes. 06:05 Now, you want to do that on your own, by all means do so. 06:08 My point is this, so there is Graves’ disease perhaps in your patient, you know about pretibial myxedema, palpitations, so on and so forth and maybe there’s indications to actually start destroying your thyroid tissue… welcome to radioactive iodine or radioactive ablative therapy and thyroglobulin can be used here to measure how much of my thyroid tissue is being injured. 06:35 Thirdly, the degree of TSH receptor stimulation… receptor stimulation on your thyroid gland. 06:44 Secondary hyperthyroidism… what does that mean to you? In secondary hyperthyroidism, you might have an adenoma functioning in the anterior pituitary releasing too much TSH… what is that going to act upon? The TSH receptor; thyroglobulin can be used to measure its activity. 07:02 Recombinant human TSH, if perhaps that’s necessary what kind of TSH receptor? Do not forget about beta hCG. 07:10 Beta hCG, what if you had, let’s say, well, you tell me about a placental pathology that you know about. 07:19 Placental, yeah… how about choriocarcinoma, hmm? With choriocarcinoma, what are you going to produce in great abundance… beta hCG. 07:30 Could the patient then behave like a hypothyroidic patient? Absolutely, because our beta hCG, if you remember at the beginning of our endocrinology discussion with a little bit of physio and biochem, there we’re talking about structure similarity between beta hCG and TSH. 07:49 Also, what if the patient actually had Graves’ disease, this with TSH antibody. 07:57 You’re going to use thyroglobulin clinically to measure how much activity is taking place with thyroid gland… very important. 08:07 On the flip side of things, what if you have antithyroglobulin? So, this is not going to be Graves’, this would be something like Hashimoto. 08:15 With Hashimoto, you have antithyroglobulin and antibodies, but this may then provide misdiagnosis because the thyroglobulin that you’re measuring here, can’t tell the difference. 08:26 Clinically, laboratory wise, there are certain things that still come across being non specifics, so thyroglobulin is thyroglobulin. 08:35 Unfortunately, we don’t have specific methods or could be misinterpreted as being hyper or as it was actually antithyroglobulin antibodies which was causing the pathology in this particular patient. 08:52 Clinical relevance… continuing our discussion, the sodium-iodide symport. 08:59 Where is it located? On the basolateral membrane. 09:02 It is influenced by whom? TSH receptor. 09:06 There is something called a radioactive iodine uptake, RAIU; it could be used for either diagnostic or radio ablative therapy. 09:12 As I told you, not responsible to know the specific isotopes. 09:15 If you want to look it up, do so on your own. 09:18 But, this sodium-iodide symport is controlled by TSH receptor, that’s important because you’ll be using this clinically, how? Well, in Graves’ disease, how much TSI are you producing? A lot, and it’s going to bind to TSH receptor on the entire thyroid gland. 09:35 So, therefore, every single sodium iodide symport is being stimulated. 09:42 If you’re using your radioactive iodide as being diagnostic then you can imagine that that entire thyroid gland is taking up the iodide. 09:51 What is radioactive anything look like on a imaging study? Bright, it will be lucent, right? So, if you are suspecting Graves’ and every single TSH receptor is stimulated and it’s taking up all that iodide, you can only imagine that on imaging study, it will not be black, but it will be bright and it will be “lit up”. 10:21 Deficiency of iodine results in increased sodium-iodide symport activity, why? If… not so much in developed countries, but in developing countries, perhaps there might be lack of access to iodine and you’re worried about lack of T3, T4 production. 10:40 So, therefore, the sodium-iodide symport is going to start increasing its activity. 10:45 Could you find a goitre in this instance? Sure, you can. 10:50 Competitive inhibitors of sodium-iodide symport, the drugs that you should already know include thiocyanate and perchlorate. 10:59 Let’s move on to the most important enzyme here, the thyroid hormone synthesis, especially from a pathologic point of view. 11:08 What if you have antibodies other than attacking peroxidase? Hashimoto, but why didn’t you say that you could have antibodies attacking thyroglobulin? Sure, you can. 11:19 Point is anywhere along the line if you disrupt the synthesis of your thyroid hormone, aren’t you resulting in Hashimoto? Yes, you are. 11:29 Lymphocytic infiltration of the thyroid gland, we will talk further and we’ll refer to this as being type 4 hypersensitivity; could be type 2 as well. 11:37 Keep that in mind, anytime that you have an antibody that is attacking something as another type 2. 11:43 You have drugs that you need to make sure that you’re familiar with known as propylthiouracil methimazole PTU is also interesting because it also peripherally is going to inhibit the conversion, conversion of what? T4 to T3. 12:01 What is the name of the enzyme responsible for that conversion? It’s called deiodinase. 12:05 So, PTU is an interesting drug, quite effective not only with inhibiting that enzyme peroxidase in your thyroid gland toward the indications in which maybe perhaps you want to use PTU… Graves’ disease, right, hyperthyroidism and in addition, peripherally, if you inhibit the conversion of T4 and T3 aren’t furthering retarding or delaying the functioning of your thyroid hormone… absolutely. 12:36 Number four, organification is inhibited by high levels of iodine. 12:42 All that I wish to say here is I’ll mention Wolff-Chaikoff effect and number five is your deiodinase. 12:52 All these numbers that you’re seeing here correspond with the previous illustration that I mapped out for you very clearly. 12:59 And number five is the deiodinase and we have centrally acting and peripherally acting; in the picture that is going to be your centrally acting. 13:08 It is the enzyme responsible for converting T4 into T3. 13:12 Now, in periphery, there are certain types of deiodinases based on the location as to where you want to convert your T4 to T3 and you have numbers or locations called 5 and 5-prime and you have 5-prime deiodinase, 5 deiodinase and that’s your type I, type II, type III… that’s a lot of detail from physio, but for path at least understand that you have centrally and peripherally acting deiodinase and some of these deiodinases not only would be converting T4 into active T3, but you tell me what’s the name of that inactive T3 that you’re hopefully quite comfortable with or familiar with? Reversed T3. 13:58 Hence, you see rT3. 14:01 You want to think of it as being inactive T3, it converts your T4 into T3 who does deiodinase, what type? At this point, I’m not going to go into that, but you have certain deiodinases in which you are increasing reverse T3 and when you increase reverse T3, you have less activity of thyroid hormone and therefore, your patient is going to behave more so like a hypothyroid patient… hypothyroid patient. 14:31 Reverse T3 is inactive. 14:37 Our next topic here is going to walk you through a little bit more detail as far as the molecular functioning of your hypothalamal pituitary thyroid axis. 14:50 We talked about the thyroid follicular cell, I showed you an illustration earlier where we dove into greater detail. 14:59 Here’s a capillary so that obviously will be the blood side responsible for bringing and delivering your iodide to the sodium-iodide symport and what hormone is responsible for influencing the sodium-iodide symport? TSH, TSH receptor complex. 15:20 In Graves’, how would you then describe that type of uptake of radioactive iodide? Diffused uptake versus we’ll talk about later a hot nodule. 15:32 A hot nodule would be focal and what would be the entire thyroid gland that is “lit up” in the middle is your homogenous area of eosinophilic or pinkish, but in this case, we’re just showing you something like oranges, but homogenous so colloid. 15:53 Now, we’ll get into further detail of something that I mentioned earlier to you with the genes. 16:00 Let me set up this picture to the right. 16:03 We are blowing up a follicular epithelial cell. 16:07 What you’re seeing here is a thyroid gland on your left; in the middle, is a thyroid follicular cell that is being blown up a little bit more and then further amplified all the way to the right and that’s a spectrum. 16:21 What you’re focusing upon here, I’m not going to obviously go through everything, but I want you to focus upon TSH receptor here and you must know that this is G-coupled, which one? If you’re thinking cyclic AMP… GS. 16:36 GS, cyclic AMP upregulates thyroglobulin. 16:40 Now, why is this important? If you do have an adenoma with your thyroid gland and such, then understand that many time, and this is what I mentioned earlier, is the fact that you might have a GS type of constitutive activation and if you do then you may result in certain pathologies in which you then increase your thyroid hormone functioning. 17:08 Location of this cell, peripheral. 17:10 So, this is not the thyroid gland, get away from it. 17:13 This is a peripheral cell, maybe it’s a bone, maybe it’s the heart, maybe it’s the liver… it’s the peripheral cell. 17:21 The first order of business is to make sure that you convert your T4 into T3 that brings us to what enzyme? Deiodinase. 17:27 What kind of T3 are you producing here so that you can promote activity? Not reversed T3. 17:35 T3, there you go, there’s that membrane and there’s no G-protein here, do you see the G-protein? No, why? Thyroid hormone is lipid soluble. 17:46 Not only that but where’s the receptor of your thyroid hormone located? In the cytoplasm. 17:55 You see where it’s… that lighter shade of beige, that’s a cytoplasm. 18:01 You’ll notice that T3 does not bond to receptor there because there isn’t one for thyroid hormone in the cytoplasm. 18:09 There is a topic that we had earlier with the table that I showed you and if-if you have a hormone that is lipid soluble and where-where is its receptor located? Either in the cytoplasm or nucleus. 18:21 The receptors in which it’s in the cytoplasm would be for the adrenocortical hormones. 18:26 Here, we have a receptor down in the nucleus, T3 gets right down into the nucleus. 18:31 You’ll notice that it binds to its receptor there in the nucleus. 18:35 If a coactivator, this then brings about the respective expression that is required for that particular organ. 18:43 Maybe it’s the bone, therefore responsible for linear growth and so on and so forth.
About the Lecture
The lecture Thyroid Hormone Function by Carlo Raj, MD is from the course Thyroid Gland Disorders.
Included Quiz Questions
What results from a deiodinase deficiency?
- They will be unable to peripherally transform T4 to T3.
- They will be unable to convert iodine to iodide.
- They will be unable to form complexes with thyroglobulin.
- They will have low circulating levels of T4.
- They will have low levels of tyrosine.
What is NOT determined by the presence and amount of thyroglobulin?
- The amount of anti-thyroglobulin antibodies in serum
- Thyroid origin of the biopsied tissue
- The mass of thyroid tissue present
- The presence of injury to thyroid tissue
- The degree of TSH-R stimulation
What centrally inhibits peroxidase?
- Methimazole
- RAI
- Thiocyanate
- rT3 deiodinase
- Perchlorate
What may be present in a patient with a normally functioning thyroid gland but symptoms of hypothyroidism?
- Excess rT3
- Graves disease
- Excessive anti-thyroglobulin antibodies
- Inhibition of peroxidase synthesis
- Thiocyanate overdose
Which statement regarding thyroid hormone function in peripheral cells is FALSE?
- T3 is transformed into T4 by deiodinases.
- T3 is lipid-soluble.
- Thyroid hormone receptors are located in the nucleus.
- The thyroid hormone requires a coactivator to promote the expression of genes.
- Organification is inhibited by high levels of I-.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |