Playlist
Show Playlist
Hide Playlist
Leukemia: Acute Myeloid Leukemia (AML) – White Blood Cell Pathology
-
Slides Leukemia White Blood Cell Pathology.pdf
-
Download Lecture Overview
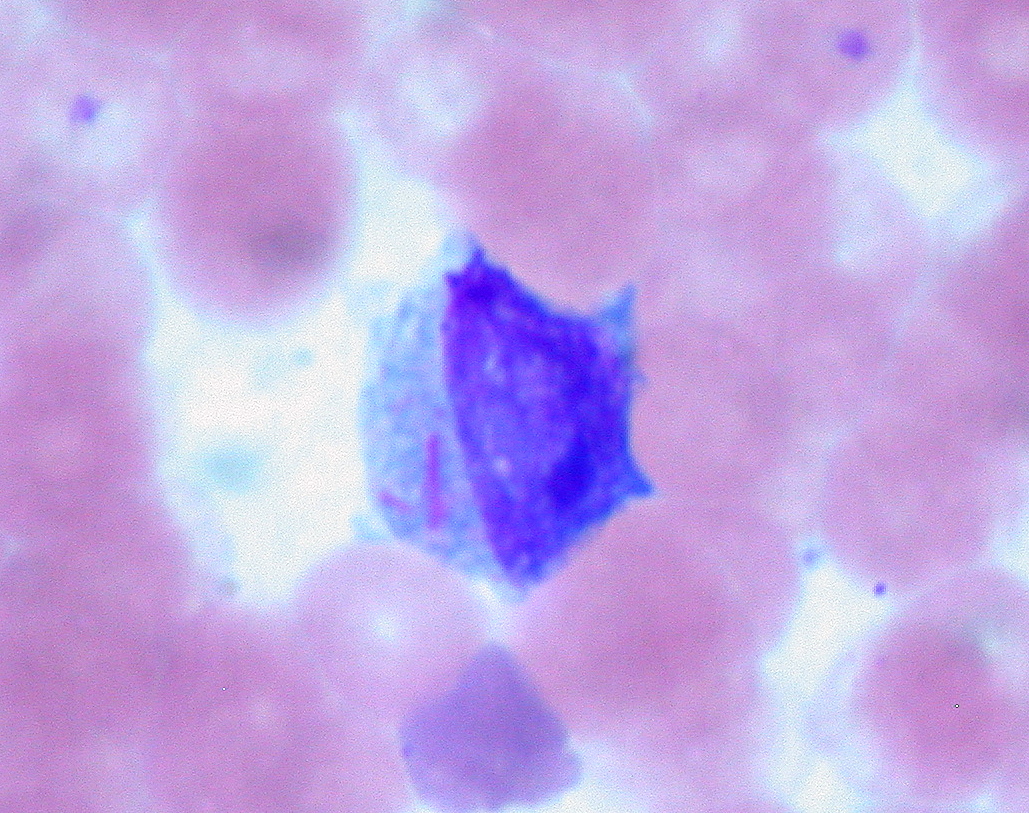
00:00 Our topic is AML, acute myelogenous leukemia. 00:03 Our focus here will be, in fact, M3. 00:06 You must memorize if you haven't already for M3. 00:10 Translocation 15;17. 00:12 And why that’s important to you is the fact that you can actually treat a patient with AML, M3 type with a drug vitamin actually. 00:21 A vitamin derivative known as ATRA, all trans retinoic acid. 00:25 How is it possible that you can specifically treat M3 with ATRA and really none of the others? The translocation 15;17 gives rise to in M3 a retinoic acid receptor alpha, RARA. 00:38 Excuse me? RARA. 00:42 Receptor for vitamin A alpha is what that is. 00:46 Retinoic acid receptor alpha. 00:49 Excuse me, sometimes you got to laugh, otherwise it makes it quite difficult. 00:54 8;21 is another one. 00:56 This is M2. 00:57 Please know this as being myeloblastic if I were you, myeloblastic. 01:01 Promyelocytic is M3. 01:03 Myeloblastic is M2. 01:05 Translocation number is 8;21. 01:11 Genetic abnormalities with AML lead to defects in stem cell maturation. 01:16 And by definition, what kind of blasts are you going to find or what percentage of blasts are you going to find in your bone marrow here? Greater than 20% blasts by definition, by definition. 01:30 A quick note about myelodysplastic syndrome and why is it even here? Myelodysplastic syndrome, to make your life easier, you need to think of this being preleukemic. 01:42 The method by which your patient most likely develop myelodysplastic syndrome was the fact the patient was actually receiving treatment. 01:50 While receiving treatment, unfortunately, the patient starts developing myelodysplastic syndrome. 01:56 We call this preleukemic. 01:57 Preleukemic specifically for AML. 02:01 So that means that this patient is going to have a blast count above 10, but less than 20, in the middle. 02:09 Let’s take a look. 02:10 May precede AML, myelodysplastic syndrome. 02:15 Where are you? In the bone marrow. 02:16 Myelodysplastic syndrome. 02:19 The diagnosis for myelodysplastic syndrome, because we as clinicians are getting better for diagnosing our patient, we are finding tons of patients that have MDS only because we are asking the proper questions and we know exactly as to what we’re looking for. 02:34 It's not that incident is increasing or is the prevalence and such. 02:40 It’s just the fact that we know how to identify your MDS and by doing so, you’re actually perhaps might be preventing a leukemia from taking on. 02:50 Tends to occur in older individuals. 02:52 Especially common in those treated with prior chemotherapy. 02:57 Look for that patient. 02:58 Look for that patient please with myelodysplastic syndrome. 03:02 Presents with -- Well, the first thing that you’re going to find because your bone marrow has been affected is your pancytopenias. 03:08 The symptom that the patient is going to first exhibit is going to be fatigue and tiredness. 03:14 You, as a clinician though, are worried about what in this patient? Neutropenia, therefore you’re worried about, once again, susceptibility to infection. 03:24 And now, you do have shifting to the granulocyte, but remember please preleukemic. 03:29 So you’re not going to find a blast count greater than 20, less than 20, but pretty damn close. 03:36 Dysplasia in one or more lineages. 03:39 Myelodysplastic syndrome, it’s getting ready to go on to acute myelogenous leukemia. 03:48 Now, characterized by abnormal myeloid blasts. 03:51 Large nuclei and prominent nucleoli. 03:53 What does this mean? Let’s get back to task of hand. 03:56 I took a little bit of pause there and inserted myelodysplastic syndrome because I need you to understand that myelodysplastic syndrome would be-- For you, consider to be a preleukemic issue. 04:10 Specifically for AML and look for the patient elderly and prior chemotherapy, myelodysplastic. 04:17 Now, the blast cell, what is it? The blast is a large nuclei and prominent nucleoli. 04:23 It’s a blast. 04:23 It’s huge. 04:25 And on bone marrow aspirate, you'll find there to be greater than 20% blast with AML. 04:32 Let’s talk about M3 in great detail. 04:34 M3 is a promyelocytic type of myeloid cell. 04:38 Acute promyelocytic leukemia. 04:41 Cytoplasmic granules with occasional, occasional, known as Auer rods. 04:46 Now, what are Auer rods? Auer rods are going to stain for and look for this description, peroxidase, okay? Myeloperoxidase. 04:56 A couple of times when myeloperoxidase becomes important for you on your boards. 05:01 Myeloperoxidase enzyme, responsible for creating your bleach in neutrophil. 05:07 Remember that, myeloperoxidase. 05:09 You go from hydrogen peroxide into bleach or hypochlorous acid, number one. 05:14 Number two, Auer rod, stains from myeloperoxidase. 05:19 And number 3, if I was to tell that your patient maybe, well, staining for what’s known as your -- We have c-ANCA and p-ANCA, right? And with this, one of those ANCAs will be myeloperoxidase positive. 05:34 Do you know which one? Good. 05:38 This, in fact, is going to be your p-ANCA, which is also called MPO ANCA or myeloperoxidase. 05:46 On the boards for you, three different times that are important for you clinically, myeloperoxidase. 05:50 Auer rod is one of them. 05:52 What is it? It’s a needle-like structure. 05:54 It’s an azurophilic granule stain with antibody against, there you have it, myeloperoxidase. 05:59 Do not forget that, ever. 06:02 Because the description of that Auer rod might actually come back to be positive for myeloperoxidase. 06:06 And if you aren’t paying attention, you miss a question unnecessarily. 06:09 Now if you see one, it’s the most likely M3. 06:13 Now, could it be the other AMLs? Sure it can. 06:17 Sure it can. 06:18 But if your patient has 15;17 translocation and you find that the treatment for 15;17 with ATRA, all trans retinoic acid, tends to be effective, then you this is an Auer rod. 06:32 If you take a look at this picture here, you see the needle-like structure that the arrow is pointing to. 06:37 The needle-like structure that the arrow is then pointing to, in fact, is an Auer rod. 06:41 It then is positive for your myeloperoxidase. 06:45 This will be a picture for your acute myelogenous leukemia. 06:49 And these are the large nuclei with nucleoli. 06:51 These then represent the blast, the blast, the blast. 06:55 But this however is actually being identified in your peripheral blood smear. 07:00 The blast could be located in your bone marrow. 07:02 They are in fact greater than 20%. 07:07 Here’s my FAB classification. 07:08 I want you to get a decent idea of the different types of myeloid cells that you can create from M0 all the way down to M7. 07:18 Before going on though, I want you to take a look at M3, acute promyelocytic leukemia. 07:27 Anything before M3, well you could have AML type 2 and that’s myeloblastic. 07:32 And then, I want you to move on further. 07:34 Here’s M5, monocytic. 07:37 This is the one that I’d like for you to know as having gingival hyperplasia. 07:42 Gingival hyperplasia with M5. 07:46 And we have M6, you produce more RBCs. 07:48 By the time you come to M7, platelets. 07:50 I don’t care how you do this. 07:51 From M0 to M7, you’re going to the myeloid lineage. 07:55 Our focus has been, thus far, specifically on M3, translocation 15;17, retinoic acid receptor alpha. 08:03 The fact that you can find Auer rods, I gave you all that information. 08:07 Apart from that though, I cannot guarantee, they’re not going to ask you about the others. 08:11 So give yourself a nice little organization. 08:13 Next up, after M3 will be monocytes. 08:18 M5 is gingival hyperplasia. 08:20 After that is M6, the RBC. 08:22 And by the time you come to M7, megakaryocyte and if I were you, I’d make sure that I know what a megakaryocyte looks like in your bone marrow. 08:31 They like the one a lot. 08:32 So please be able to identify megakaryocyte in a bone marrow for M7. 08:37 This is a FAB classification for all acute myelogenous leukemia and your age group here is between 15 to 60. 08:47 AML, what’s going on? Anemia, fatigue, tiredness, susceptibility to infection, leukopenia, bleeding, thrombocytopenia, bone marrow infiltration, bone pain. 08:58 Things we have talked about already because you’re invading the bone marrow. 09:02 Excuse me, actually, the cancer is originating from the bone marrow. 09:06 So the bone marrow is infiltrated and then you’re dumping the cells into your circulation, welcome to leukemia, right? And at some point in time, it could just then enter the lymph node and present as lymphoma. 09:20 Yes it can. 09:23 M3 can be treated with ATRA which stands for all trans retinoic acid. 09:28 Why? Because the translocation 15;17 will give you, the clinician, the receptor to then treat it properly which is retinoic acid receptor alpha. 09:41 How many letters in DIC? One, two, three. 09:44 Correct. 09:45 DIC could also manifest from M3. 09:50 Once again, one last time, do not forget what M3 stands for. 09:54 Acute promyelocytic leukemia or promyelocytic leukemia, PML. 10:00 Don’t lose the question because you weren't thinking or or you know I mean like don’t look at things just unidimensional. 10:08 Look at things as from a three-dimensional point of view. 10:10 What else could they call this? How else could they call this? Oh, I know this information. 10:15 It’s stuck in my head. 10:16 I just need to bring it forward. 10:18 I’m here to try to help you do that.
About the Lecture
The lecture Leukemia: Acute Myeloid Leukemia (AML) – White Blood Cell Pathology by Carlo Raj, MD is from the course Leukemia – White Blood Cell Pathology (WBC).
Included Quiz Questions
Which of the following cytogenetic abnormalities are associated with acute promyelocytic leukemia?
- t(15;17)
- 11q23 abnormalities
- t(14;18)(q32;q21)
- t(11;14)(q13;q32)
- t(8;21)
Which of the following translocations is associated with acute myeloblastic leukemia?
- t(8;21)
- t(14;18)
- t(9;22)
- t(11;14)
- t(15;18)
Which of the given values represents the percentage of blast cells in pre-leukemic conditions?
- Less than 20%
- Greater than 20%
- Less than 5%
- Greater than 25%
- Less than 10%
Which of the following is seen in acute promyelocytic Leukemia-M3?
- Auer rods
- Bence Jones protein
- Cabot rings
- Bart hemoglobin
- Balbiani rings
What does the FAB classification categorize M6 as?
- Acute erythroid leukemia
- AML with maturation
- Acute megakaryocytic leukemia
- Acute promyelocytic leukemia
- Acute myelomonocytic leukemia
Which of the following subtypes corresponds to acute promyelocytic leukemia?
- FAB subtype M3
- FAB subtype M5
- FAB subtype M7
- FAB subtype M4
- FAB subtype M6
Which of the following classes of acute myeloid leukemia can be treated with all-trans retinoic acid?
- Acute promyelocytic leukemia
- Undifferentiated acute myeloblastic leukemia
- Acute monocytic leukemia
- Acute erythroid leukemia
- Acute myeloblastic leukemia with minimal maturation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
6 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent direction, subject is completely understood by the end of the lecture
Excellent explanation, easy to follow and understand. Professor Raj takes a topic so difficult and makes it look easy and fun.
Thank you so much, that was great and well explained.
Great lecture to understand such a difficult subject, Thank you Dr.Raj