Playlist
Show Playlist
Hide Playlist
Acute Pancreatitis: Definition, Etiology and Diagnosis
-
Slides Pancreas and Biliary Tract.pdf
-
Download Lecture Overview
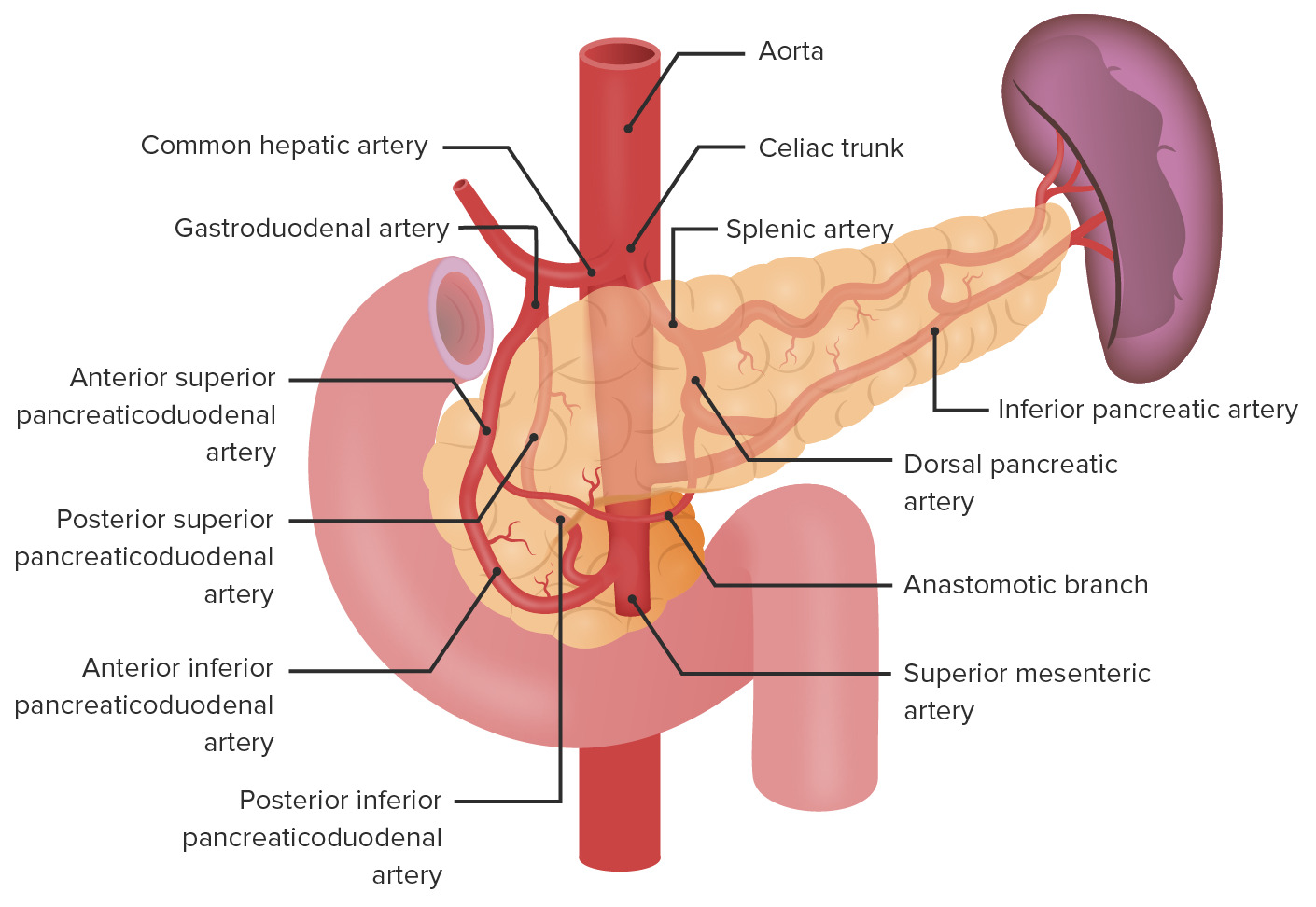
00:02 Acute pancreatitis, by definition, everything in your pancreas is going absolutely crazy. In your head, you should be thinking about the pancreas and divide it into two physiologic organs. And by that, I mean you divide it into exocrine pancreas and you divide it into endocrine pancreas. 00:23 Initially, when there's damage that has taken place to the pancreas, all these enzymes that are being released and, in your head, you should also be thinking about, "Whoa, those enzymes from the pancreas that are responsible for protein digestion include trypsin, carboxypeptidase, endopeptidase and so forth, trypsin being the most potent. 00:43 If you're dealing with the enzymatic or exocrine pancreas and you wish to metabolize your lipid and then that discussion takes you to lipase. 00:51 In any case, that's a lot of enzymes within the pancreas, is it not? And all these enzymes are being released locally, you might have utmost enzymatic destruction resulting in a term called autodigestion. 01:07 Important etiologies that we'll take a look at: alcohol being quite common. 01:11 This pain that the patient's feeling is not only epigastric, but then also radiating to the back. When the time is right, I will then then give you a list of differentials quickly to have you differentiate between different types of epigastric pain. 01:25 Gallstones could also be a possible cause of pancreatitis and we'll talk about that in greater detail and it's a nice little story. 01:32 In other words, you had a gallstone that was in my gallbladder, ended up in my biliary tree and eventually makes its way to the the second part of the duodenum in which it may then cause what's known as compression atrophy. 01:45 Other causes also, hypercalcemia, may cause damage to the pancreas. 01:49 And, for example, if you have a patient that has a type 4 type of hyperlipidemia or even worse case, a type 1 hyperlipidemia. 01:58 And if that lipoprotein lipase is not present, "Up goes my chylomicron. Oh my goodness, my triglyceride levels are ridiculously high! Thousands." The first organ to be damaged here would be the pancreas. 02:12 Drugs, I'll give you a list of drugs here that cause acute pancreatitis. 02:16 We have AZA or azathioprine. We have pentamidine, and we have hydrochlorothiazide, being important drugs. There's more to come. 02:25 Infections such as mumps. With mumps, even though it might be rare, you want to keep this mind because it may then cause parotitis, orchitis. 02:39 It might be in my best interest not to grab my testicles. 02:42 We have coxsackievirus and we also have parasites that may all cause acute pancreatitis. 02:51 Embryologic issue that you might have called pancreatic ductus divisum and remember with the proper embryologic development you have though, the ventral head and the dorsal head, and all these may then result in an abnormal type of division called a ductus divisum or there might be inherited autosomal dominant disorder resulting in acute pancreatitis. 03:16 Interesting enough, you were performing a procedure in which you were trying to identify the pathology in your bile duct. In the process, you actually ended up causing damage to the pancreas, that's a risk factor when implementing endoscopic retrograde cholangiopancreatography. That post exam, you might actually bring about damage to the pancreas or just straight up blunt trauma to the abdomen. 03:48 Important etiologies for acute pancreatitis: Vascular, we have ischemia or perhaps vasculitis resulting in acute pancreatitis. 03:58 Miscellaneous include, well, importantly, cystic fibrosis. So imagine a child that has extremely viscous fluid within his or her ducts. 04:12 Most likely a child of Caucasian decent and with that viscous type of fluid within the ducts, not only could it result in what's known as your bronchiectasis and eventually result in pneumonia because you have increased thickness there, but they might have increased thickness within the pancreatic ducts. So therefore, anatomy, the pancreatic duct is moving towards the second part of the duodenum. 04:34 The fluid is moving in that direction. 04:36 If you end up having all those viscous fluid within your duct, and imagine now, that you may then cause backup congestion and compression and eventual acute pancreatitis, an important point, or the two types of ulcers that we discussed earlier. 04:53 If your patient is giving you the following symptoms initially: "Hey, doc. I have this pain at midnight, late at night when I'm asleep. 05:05 I have to go downstairs to the kitchen, and I have to open up the fridge and I end up having a pretty decent amount of cake that we had for yesterday's birthday and actually, the pain then went away." So initially, what I'm giving you here are the symptoms of duodenal peptic ulcer disease in which the pain then has been relieved by eating but then eventually what may then happen, if not properly taken of care of, is that this may then perforate. And when it perforates, imagine where you are. A duodenal peptic ulcer disease, where are you? Think. 05:39 First part of the duodenum. If you were to perforate through, you may then cause damage to the gastric duodenal artery and, in fact, then bring about damage to the pancreas. Important. Miscellaneous? Yes, but incredibly clinically important. 05:54 Signs and symptoms. As I told you, I'll give you some important epigastric pain issue. Here, with acute pancreatitis, the patient is definitely feeling pain in the abdomen, but then it radiates to the back because of the rectoperitoneal type of journey of the head of the pancreas towards the tail, meaning to say that it's going to be up with the spleen, is it not? If this gets damaged, then the patient is also expressing pain in the back as well I just gave you another epigastric pain where the pain then went away after consuming food and that's your duodenal peptic ulcer disease or you could have a patient with epigastric pain and it and it does not radiate to the back, in which the pain gets worse immediately after eating and that will be gastric type of peptic ulcer disease. 06:41 Epigastric pain, their differentials become important here. 06:43 Low-grade fever, nausea and vomiting or signs and symptoms that you can expect, but you'd be finding that with any type of -itis, so obviously giving you more information. 06:56 There might be tachycardia, orthostasis or perhaps even ileus due to obstruction. 07:02 And a couple of important things here, these might be rare in clinical discovery; however, keep in mind because if you find something like this in a stem of a question or you see a picture of what's known as Cullen's sign. 07:14 In other words, there'll be hemorrhage around the umbilicus. C-U-U-M. 07:22 Cullen is bleeding around the umbilicus or there might be hemorrhage in the flanks and the flanks will be the sides of your body, out back towards the hips and basically where you find you kidneys. 07:36 Are we clear? And around there, if you ended up finding hemorrhage, we then call this more or less hemoperitoneum or rectoperotineal hemorrhage. This will be referred To as being your Grey-Turner's sign. 07:48 Rare as it may be, keep this in mind because remember on your boards, they have to give you specific information so that you're moving in a certain direction and you're choosing one answer choice over the other with almost utmost confidence. Now that's it. 08:03 Obviously, there's always going to be a little bit of doubt, trust me. 08:07 Always, but that's okay though as long as you choose the most educated answer then you'll be in good shape, you move on. 08:17 Lab testing for acute pancreatitis specifically, keep in mind that amylase and lipase may be found, but which one's more specific for acute pancreatitis? In fact, it's lipase. 08:27 One thing interesting once again that we'll see is that the enzymes that you would find to be elevated in acute pancreatitis may not correlate with the severity of the disease. We had this very discussion when we did liver disease and the transaminases. Even though the transaminases being elevated would tell you that the patient most likely has liver disease. 08:47 It does not correlate with the severity. Same concept here as well. 08:54 Serum liver function test: if elevated, may then suggest gallstone pancreatitis. 08:58 We will talk about gallstones in great detail. And with gallstones, at least think about this before we actually get to the details. 09:07 You can have a stone that begins in the gallbladder. 09:10 Let's say it's cholesterol stone or a pigment stone if there is bulirubin. 09:14 That stone may then escape from the cystic duct and you are then moving throughout the biliary tree and as then moves through the biliary tree, which is then technically called your your choledocholithiasis, understand that you might have compression issues and also injury that might be taking place to adjacent organ, including the liver and then also including the pancreas. 09:39 We'll talk more later, it's important. 09:41 Imaging studies. You will do an abdominal and, stop -- chest x-ray. 09:46 What' Now, understand what's going on here, don't just memorize this. 09:50 Where is the pancreas located? Right, in the abdomen. Okay. 09:54 Then why the chest? Is there such a thing in which you have a hernia in which the pancreas comes up in the thorax? Are you kidding me? I suppose anything is possible, but listen, this is why you're doing a chest x-ray. 10:06 This pancreas has been damaged, okay? You do an abdominal x-ray and you might find 'a sentinel loop.' Stop. The pleural effusion and ARDS have nothing to do with the abdomen and why is it associated with pancreatitis? Enzymes. What does ARDS mean? Acute respiratory disease syndrome. It means that the alveoli had been destroyed. There's every possibility that enzymes being released from the pancreas into circulation may then cause damage to the lung extensively to the point where the pleural cavity may then develop fluid and the alveoli may then perish. Is that clear? Therefore, what you're looking for in a chest x-ray would be atelectasis. 10:56 CT: Useful for evaluation of complications, normal in about 30% of your patients, however. 11:03 ERCP: Reserved for therapeutic interventions, and by that we mean that - Remember, ERCP itself, even though you're trying to explore what's going on with with pancreas and what's causing damage, in the process you might actually cause damage to the pancreas, so be careful with ERCP. 11:21 So it could be diagnostic, but then also be an etiology of lesion. 11:27 MRCP, obviously playing a much greater role. We have MRI, is what the MR stands for, and it's non-ivasive, increasingly replacing the ERCP for obvious purposes.
About the Lecture
The lecture Acute Pancreatitis: Definition, Etiology and Diagnosis by Carlo Raj, MD is from the course Pancreatic and Biliary Tract Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT a common risk factor for acute pancreatitis?
- Smoking
- Alcohol
- Hypertriglyceridemia
- Gallstones
- Hypercalcemia
For which of the following genetic diseases is acute pancreatitis a common complication?
- Cystic fibrosis
- Hemochromatosis
- Wilson's disease
- Phenylketonuria
- IgA deficiency syndrome
A 20-year-old man occasionally consumes alcohol and has a serum triglyceride level of 1,000 mg/dL. He was diagnosed with acute pancreatitis, and his cousin was treated for acute pancreatitis and alcoholic cirrhosis 1 month ago. What is the probable cause of this patient's acute pancreatitis?
- Hypertriglyceridemia
- Alcohol
- Drugs
- Hereditary pancreatitis
- Gallstones
A patient who presents with congestive cardiac failure developed muscle weakness after treatment. After a few days, she presented with acute pancreatitis. Which drug is the probable cause of the acute pancreatitis?
- Hydrochlorothiazide
- Spironolactone
- Digoxin
- Propranolol
- Furosemide
A 10-year-old boy presents with swelling and pain in the parotid regions and testicles. He began to develop epigastric pain. What is the MOST likely cause of epigastric pain?
- Acute pancreatitis
- Acute cholecystitis
- Acute hepatitis
- Acute appendicitis
- Acute peptic ulcer disease
Which procedure can cause acute pancreatitis as a complication?
- ERCP
- MRCP
- Upper GI endoscopy
- Ultrasound-guided FNAC
- X-ray of the abdomen
What is the sign on clinical examination that shows discoloration around the umbilicus?
- Cullen's sign
- Cushing's sign
- Caput medusa
- Kosher's sign
- Sitkovsky's sign
Which of the following is NOT associated with Grey-Turner's sign?
- Chronic pancreatitis
- Acute pancreatitis
- Blunt trauma to abdomen
- Retroperitoneal hemorrhage
- Ruptured ectopic pregnancy
At which of the following sites can a gallstone become impacted, leading to acute pancreatitis?
- Sphincter of Oddi
- Right hepatic duct
- Left hepatic duct
- Cystic duct
- Neck of the gallbladder
An increase in which of the following enzymes indicates acute pancreatitis?
- Pancreatic amylase
- Salivary amylase
- Pepsin
- Gamma-glutamyl transferase
- AST
Customer reviews
4,7 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Such personality! Loved your lecture Dr. Raj! Keep up the good work!
the lession is very insteresting, but i think i could be explained a little better, showing and explaining an image of CXR of atelectasis, sentinel loop AXR. Also it coulde be better if hidroclorotiazied mecanism way of producing muscle weakness is explained after answering the question of the quizz, and the indications of the ERCP explained. Thanks
The review was easy to understand with clear explanation. I also appreciated the test sample after the lecture. It tested my knowledge regarding the subject matter thank you