Playlist
Show Playlist
Hide Playlist
Leukemia in Children: General Symptoms
-
Slides Leukemia Pediatrics.pdf
-
Download Lecture Overview
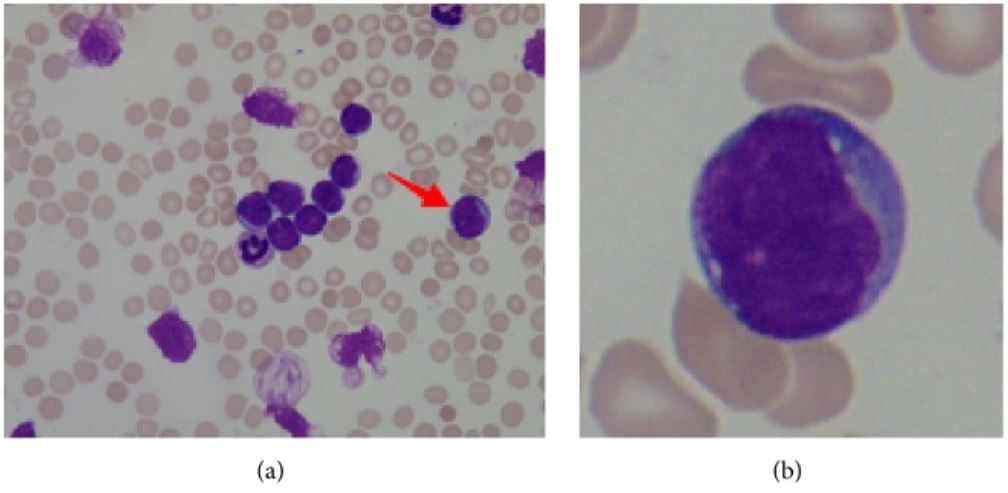
00:01 So, let's back off now and talk about what are the general symptoms of leukemia. 00:07 If a child has leukemia, what do they look like? Well, first of all, they're often lethargic. 00:14 They have less energy to get through their day. 00:17 Sometimes they have respiratory distress if there's a mediastinal mass that might be pressing on a trachea or something, but usually it's a non-specific find of lethargy, some fatigue, they may have increased bleeding if their platelet counts are down, and they may have increased rates of infections. 00:36 Children may present with bone pain as their chief complaint when they have leukemia. 00:40 Also, you may find on exam that they may have fever, pallor from an anemia, tachycardia from an anemia, and bruising and petechiae from low platelet counts. 00:53 They may have lymphadenopathy, hepatosplenomegaly, or in boys testicular enlargement from some tissues growing with cancer cells in them specifically the lymph and the splenic system. 01:06 They may have facial swelling, and wheezing, and tachypnea, if they happen to have a mediastinal mass. 01:13 And they may have CNS involvement which actually is not uncommon in ALL. 01:20 So, how do we diagnose this problem? Well, the first mainstay of picking up anemia is the CBC and frequently we'll find signs on the CBC that something isn't right. 01:33 We usually will see what we say is two cell lines down. 01:37 Sometimes, one cell line down but often that could be something else. 01:41 For example, if the patient has thrombocytopenia only, this could be immune thrombocytopenic purpura, not cancer. 01:49 We would treat that very differently. 01:51 But typically they'll have more than one cell line down which means they may have some anemia, some thrombocytopenia, some leukopenia, some leukocytosis at times with a very high white count, or neutropenia. 02:05 You also may see a particular type of cell called a blast. 02:09 When you see a blast on a CBC differential, you should be highly concerned that that patient might have cancer. 02:17 And you should probably refer that patient to a hematologist-oncologist. 02:21 In CML, we sometimes see very marked hyperleukocytosis with white counts in the 50 to a hundred range and we often see normal myeloid precursors on those CBCs. 02:35 Also in patients where we suspect they might have leukemia, we often will check a chemistry panel to look for signs of tumor lysis syndrome such as a high potassium or high phosphate. 02:48 So we will check that but that's not a great diagnosis mechanism though rarely you may see it. 02:54 Also, we could do, if the patient specifically had CML, we could look for the BCR-ABL gene, that's usually a little bit later on. 03:03 What radiology do we get? We usually get a chest x-ray and a chest x-ray can often show a large mediastinal mass like you can see in this patient with a widened mediastinum. 03:15 To confirm the diagnosis, we will do a bone marrow aspiration and a biopsy to try and get some of that bone marrow tissue. 03:24 That is then sent for cytology and you can actually identify the type of cancer off of cytology. 03:31 Additionally, we will often do a lumbar puncture to inspect for CNS involvement especially in ALL. 03:38 So who is at highest risk when they have leukemia? Who are the high-risk patients? Well, children more than ten years and less than one year are at higher risk. 03:49 The children between one and ten are at lower risk. 03:52 If their white count is very, very high, they're at higher risk. 03:55 If they have a T-cell phenotype, they're at higher risk, and if they have cytogenic changes in their leukemia cells, they're at higher risk, and lastly, makes sense, if they're not responding well to therapy, they're at higher risk. 04:09 So, what is the therapy we're giving? Well, it depends on the type of cancer, obviously. 04:16 In fact, there are complicated pathways and roadmaps that are established by multi-center groups that are how we treat these children in a very standardized way. 04:26 So, what you'll see is if you're taking care of one of these patients, they'll have a roadmap that will say things like for example, on day 7, they have to get intrathecal methotrexate. 04:35 On day 14, they'll get something else. 04:37 It's a very prescribed pathway. 04:39 We try very hard to follow the roadmap because it's been shown to have improved outcomes. 04:45 So, what does that roadmap involve? Well, in ALL, this is going to be a multi-agent chemotherapy with multiple agents, generally for 2 to 3 1/2 years, and also they will get some prophylactic intrathecal chemotherapy and/or radiation to sanctuary sites. 05:03 For AML, we will do multi-agent intensive chemotherapy for 6 to 9 months but some of these patients will weren't getting a hematopoietic stem cell transplant. 05:15 For CML, we're going to give single agent therapy with tyrosine kinase inhibitors for the BCR-ABL gene and a hematopoietic stem cell transplant for a poor response and for JMML, these patients often will require a bone marrow transplant. 05:34 So, what's the prognosis for these patients? Surprisingly good for ALL. 05:40 More than 80% and even as high as 95% of patients in low-risk groups are going to survive their ALL. 05:50 This is a great accomplishment we have in Pediatrics. 05:54 For AML, it really depends on the subtype of AML, but it's probably around 50% survival rate. 06:00 For CML, this is a lifelong disorder with tyrosine kinase inhibitor therapy and for JMML, survival of about 40% unfortunately with a bone marrow transplant which requires all the complications of bone marrow transplants. 06:15 But in general, most children have ALL and most children have a pretty good prognosis, it being cancer. 06:22 So that's my review of leukemia in children. 06:26 Thanks for your time.
About the Lecture
The lecture Leukemia in Children: General Symptoms by Brian Alverson, MD is from the course Pediatric Oncology.
Included Quiz Questions
Which of the following findings on a complete blood count is MOST concerning for leukemia?
- Blasts
- Leukocytosis
- Anemia
- Thrombocytopenia
- Neutropenia
A child with acute leukemia is least likely to present with which of the following findings?
- Mediastinal mass
- Fatigue
- Dyspnea
- Petechiae
- Pallor
Which of the following peripheral blood findings is most suggestive of chronic myeloid leukemia?
- Marked leukocytosis with normal myeloid precursors
- More than 5% blast cells
- Hypokalemia
- Morphologically abnormal granulocytes
- High leukocyte alkaline phosphatase score
Which of the following is the most appropriate initial treatment in chronic myeloid leukemia?
- Tyrosine kinase inhibitors
- Watchful waiting
- Anthracyclines
- Hematopoietic stem cell transplantation
- Radiotherapy
Which of the following best represents the 10-year survival rate in patients with acute lymphoblastic leukemia in developed countries?
- 80-90%
- 40-50%
- 60-70%
- 70-80%
- 30-40%
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
A complex topic made easy: the hallmark of a great teacher. Thanks a lot!