Playlist
Show Playlist
Hide Playlist
Inguinal and Femoral Hernias
-
Slides Hernias Surgery.pdf
-
Download Lecture Overview
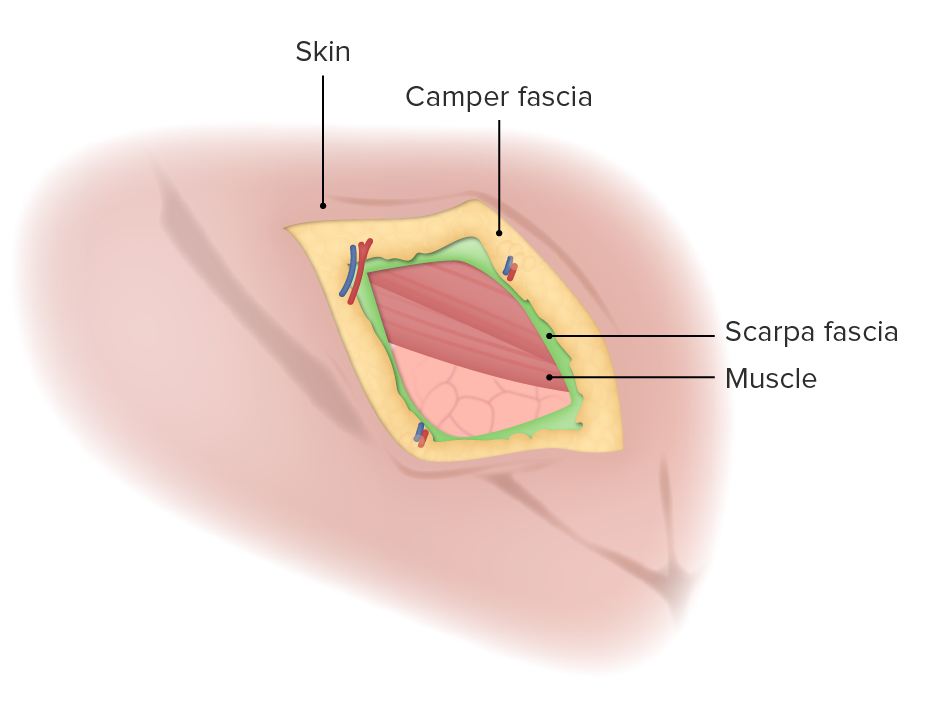
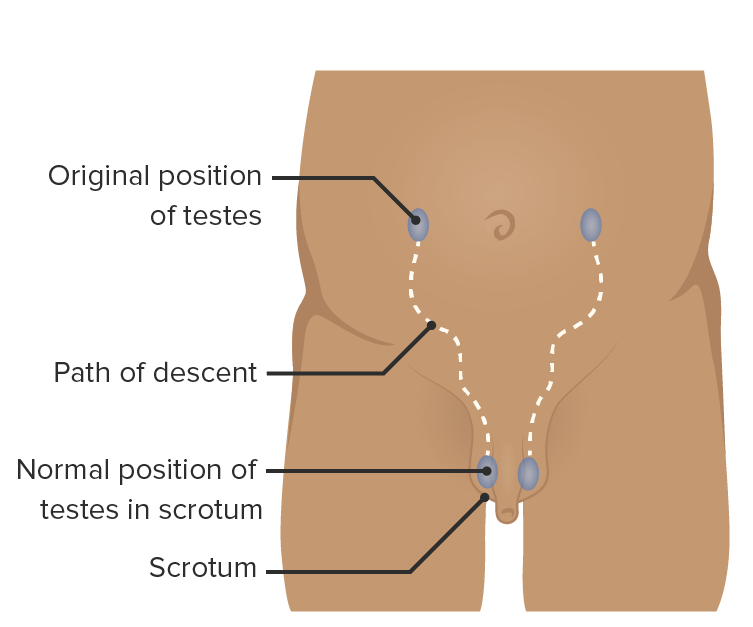
00:01 Let's begin our discussion of inguinal and femoral hernias. 00:06 This is the classic Hasselbeck triangle. 00:09 You'll notice, there are two triangles formed divided by the epigastric vessels. 00:15 To the left of the screen is the medial side of the abdomen. 00:19 Medial to the epigastric are known as direct hernias. 00:23 Lateral to the epigastric vessels are indirect hernias. 00:28 There are some different types of hernias in the groin. 00:31 We've talked about the indirect through the indirect ring. 00:35 A direct hernia, which is medial to the epigastric vessels, and the femoral hernia, which is below the inguinal ligament. 00:45 What are some of the findings or historic or physical findings associated with inguinal hernias? Let's discuss some of the high frequency findings. 00:55 First, a bulge. 00:57 This is the initial picture you are seeing. 00:59 This patient has a large inguinal bulge. 01:02 This patient also likely has been chronically incarcerated as a large defect like this did not happen overnight. 01:11 Additionally, there's variable presentations of nausea and vomiting. 01:16 The nausea vomiting occurs either because of the discomfort due to the intestinal contents going into the scrotal sac or through the inguinal canal. 01:25 Or it could actually represent a small bowel obstruction. 01:29 The bowel obstruction point of transition actually in the inguinal canal. 01:34 And lastly, obstipation. 01:36 Obstipation means the inability to pass flatus or have bowel movements. 01:42 Again, a potentially late sign of a bowel obstruction. 01:46 What are some risk factors for hernias? Commonly heavy lifting. 01:51 Whether it's part of an exercise regimen or part of daily work, people who have repetitive, heavy lifting, are a high risk. 01:59 Chronic cough patients. 02:00 What are some possible diagnoses for patients for chronic cough? Smokers, COPDiers, and patients with asthma. 02:09 Constipation, particularly in chronic in nature, and obesity. 02:15 The question is, what do these things have in common that risks the patient of having an inguinal hernia? Well, it's basically anything that increases Valsalva maneuvers, and intra abdominal pressure puts the patient at increased risk of developing hernias. 02:33 Let's go over the decision tree making for the diagnosis of inguinal hernias. 02:37 The vast majority of the time, I can diagnose an inguinal hernia based on physical examination alone. 02:44 These physical exam maneuvers include invagination of the inguinal canal. 02:49 How is that performed? Warn the patient. 02:52 Insert if one finger through the scrotum and into the inguinal canal. 02:57 That's why it's called an invagination. 02:59 Warn the patient that it can cause some discomfort. 03:01 Have the patient perform a Valsalva maneuver. 03:04 You all remember, you see it on TV. 03:06 Turn your head and cough. 03:08 They don't have to cough. They just have to bear down and produce a valsalva maneuver to see whether or not we can elicit the hernia in the office. 03:17 If the physical examination is not so clear, sometimes you may need cross sectional imaging like a CT scan of the abdomen and pelvis. 03:24 This is particularly true when it's an equivocal exam where there are limitations to your examination. 03:29 Whether the patient can't tolerate it, or they're too morbidly obese that your exam can't be trustworthy. 03:34 This is also the case in females since physical examination is limited. 03:40 Here's a management schema of inguinal and femoral hernias. 03:45 As a surgeon, I consider hernias both inguinal and femoral as either reducible or not. 03:52 And the reducible hernias, you can buy a little bit of extra time. 03:55 The patients who are not reducible may need surgery more urgently. 03:59 Let's look at a patient who has reducible hernia. 04:03 Those patients, I can offer an elective repair, and I counsel the patient. 04:08 If the bulge comes out and you can't push it back in, you develop signs of obstruction such as nausea, vomiting, or lack of bowel movements, or flatus. 04:17 Those are signs to instruct your patient to return to the emergency department. 04:23 If the patient is not reducible, that's a different story. 04:26 Those patients are then thought of as either strangulated or incarcerated. 04:31 Recall earlier in this lecture. 04:34 Strangulated patients means that the blood supply to content of the hernia are compromised. 04:40 Those patients need urgent repair or emergent repair rather. 04:45 If the patient's simply incarcerated, and it's an acute incarceration I would recommend an urgent repair. 04:52 And select patients particularly high risk patients, chronically incarcerated patients, the decision to proceed with surgery is one that you have with the patient. 05:03 Let's discuss a little bit about how to do an open inguinal hernia repair? In the subsequent slides, you'll see the exposure after incising external oblique aponeurosis. 05:15 Once you open up the external oblique aponeurosis underlying it is the spermatic cord. 05:19 The cord contains important spermatic cord vessels, vas deferens, and of course, your hernia sac. 05:30 Once the hernia sac is reduced, we, it's standard to place a piece of mesh. 05:36 Mesh is usually medical grade plastic that buttress is your repair as the tissues have already demonstrated, they have some inherent weaknesses of their own. 05:48 Question for you. 05:49 Do all inguinal hernias need to be repaired? I'll let you think about this.
About the Lecture
The lecture Inguinal and Femoral Hernias by Kevin Pei, MD is from the course General Surgery.
Included Quiz Questions
Which of the following statements is correct?
- Direct inguinal hernias protrude medial to the inferior epigastric vessels.
- The origin of the indirect inguinal hernial sac is located within The Hesselbach triangle.
- The boundaries of The Hesselbach triangle are the external iliac artery laterally, the rectus sheath medially, and the inguinal ligament inferiorly.
- Femoral hernias protrude at the internal inguinal ring.
- Indirect inguinal hernias protrude medial to the inferior epigastric vessels.
Which of the following is a risk factor for hernia development?
- Chronic cough
- Young age
- Female gender
- African ethnicity
Which of the following statements is correct?
- Patients with a reducible inguinal hernia may be managed with elective surgery and patient counseling.
- Patients with an acutely incarcerated inguinal hernia may be managed with elective surgery.
- For most patients with strangulation, additional imaging is necessary prior to surgical exploration and repair.
- Patients with a strangulated hernia may be managed with IV fluids, antibiotics, and watchful waiting.
Customer reviews
4,5 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
2 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
very well explained and pictures and slides are beautifully made
Need a few questions to make sure we learned what is important.
It is an impartant topic and is explained well.. Grate work shown in it in all aspects
Good talk I would have liked the discussion to also include post operative complications as well as recurrence rates following hernia repair.