Playlist
Show Playlist
Hide Playlist
Insulin Types and Glycemic Excursions – Diabetes Medications
-
Slides DiabetesMedications EndocrinePharmacology.pdf
-
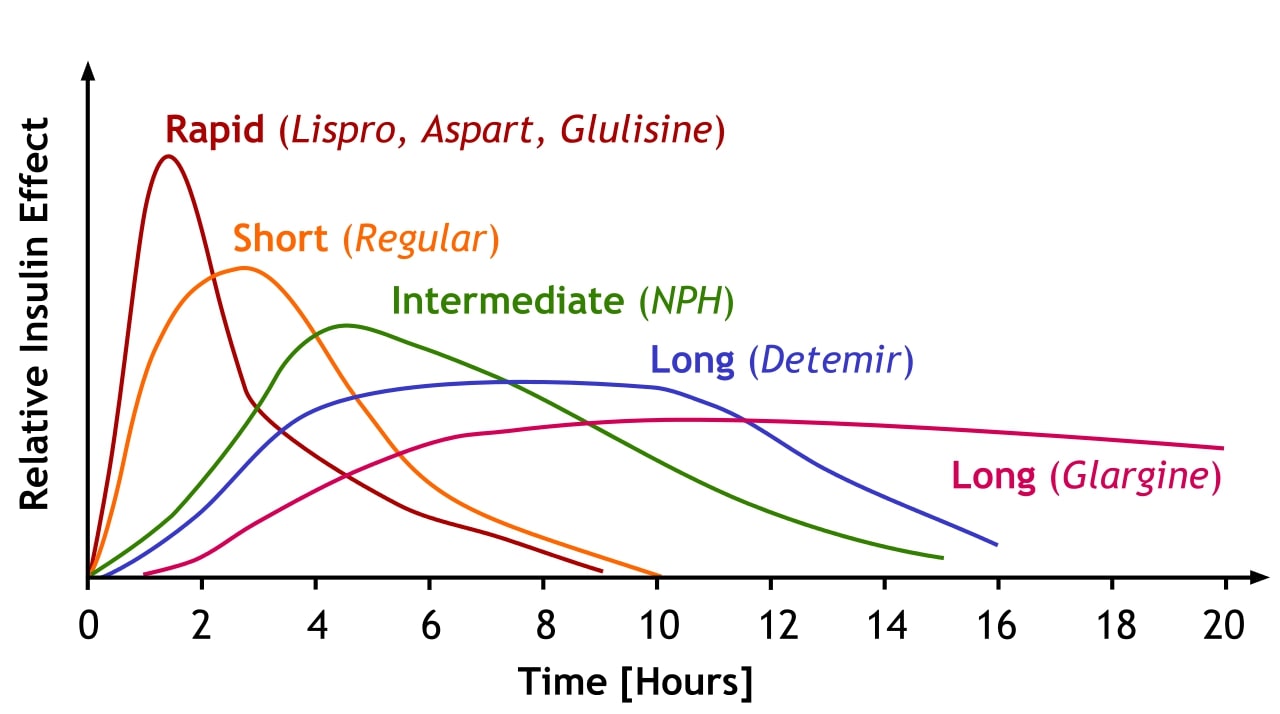
Download Lecture Overview
00:01 Now we have different kinds of insulins that are available on the market. 00:06 Let's start off with the very rapid-acting insulins. 00:09 So there are three types. 00:10 There is aspart insulin, there is lispro insulin and there's glulisine insulin. 00:16 Now I'll show one of them for illustration purposes. 00:19 You can see that there's a very high onset of action, very quick and a very short offset of action. 00:26 Now, these curves are not pharmacologically correct. 00:30 They are only used for illustration purposes. 00:32 Don’t take the curves as being gospel, they are more like squares or rectangles if you will, so don’t get upset if the curves don’t match what you see in your textbooks. 00:44 The short acting insulin includes the things like regular insulin or humulin so you can see that the peak is a little bit later than the rapid-acting insulins, they last a little bit longer and anywhere from 30-60 minutes is the peak and anywhere from 6-9 hours is the duration of action. 01:03 The intermediate insulins was quite frankly aren't used that much anymore, can be the NPH type of insulins. So the peak is between 1-4 hours, it could be longer and it lasts a little bit longer perhaps 8-12 hours. 01:18 Finally, we have the long-acting insulins. 01:21 Now the long-acting insulins can be up to 24 hours long. 01:24 Now, again, don’t pay attention to the shape of the curve so much as the length of the curve. 01:29 Levemir is a great example that peaks or starts off at about 30-90 minutes and lasts for about 24 hours. 01:37 And the same thing goes with Lantus or glargine insulin, there's not really a peak time with this particular product. 01:43 It’s plotted out on slightly different vertical axis simply to show the differences in time duration, not to show the concentration duration. 01:52 If we plotted them out according to concentration, they would all land on top of each other, so don’t pay too much attention to the shape of the curve. 02:01 Now, you can see the bottom line there – we've got 24 hours in our time course. 02:07 We're gonna shorten that up and add in a few more hours. 02:10 That’s because we're going to be talking about some new insulins. 02:13 The ultra-long acting insulins and these are new that have come out probably -- they came out, started coming out in late 2018, early 2018 in some countries, started to come out in early 2019 as well. 02:26 Glargine modified, also known as Toujeo, is a ultra-long acting insulin. 02:33 We also have some inhalational insulins that I don’t think are particularly successful, let’s just say. 02:40 The first products were taken off the market, the newest product which is called Afrezza or Afrezza depending on what country you live in, is now available. 02:51 They started out in mid to 2019 so they're available but they have some limitations. 02:59 So here we go back to our insulin chart. 03:02 You can see that we've shortened the axis to extend it out to 48 hours. 03:08 Now we have the other insulins there in gray. 03:12 We're gonna talk about the long-acting, lasting 24 hours. 03:15 There's detemir, there's glargine and now we have the Toujeo insulin which is the ultra-long acting modified glargine insulin and of course we have the new insulin degludec, which is also known as Tresiba in some countries. 03:32 So now we have insulins that are going to 36 or even 42 hours. 03:37 These agents are particularly useful because there's less hypoglycemia associated with them as long as they're taken every 24 hours. 03:45 Now if you have a drug that’s taken – that gives you a 42 hour window of action, how do you take and how and why do you take it every 24 hours? Well, although the effects are additive from one day to the next, you end up having a very steady state of insulin. 04:03 The interesting thing is, is that if patients miss a dose they can take it up to 8 hours later and not really significantly affect the profile of their insulin. 04:14 When patients who were taking the very long-acting insulins did delay their insulin dosages, they had the same amount of hypoglycemic events as the 24 hours insulins, but when they took it every 24 hours their rates of hypoglycemic were actually lower than the 24 hour long insulin drugs. 04:36 So the new drugs do have some benefit, they actually do work a little bit better and because they are a little bit more concentrated, the volume that you take in under your skin is actually less. 04:48 Now let’s get back to the inhaled insulins. 04:51 When these came out we were very excited about them. 04:54 I was excited about them just from a pharmacology perspective because the brilliance in getting an intravenous product marketed as an inhaled product was just astounding to me – it was just a brilliant piece of pharmacological science. 05:09 It is a powder that is inhaled and the powder lands on the lungs and gets absorbed. 05:16 The onset is about half an hour for peak action. 05:22 It’s generally considered a meal-time insulin so you take it up to three times a day. The cartridges come in three different forms. 05:30 They come as 4-unit cartridges, 8-unit cartridges and 12-unit cartridges, so you can start to see the limitation in terms of dosing. 05:38 One of the problems that we started to see is pulmonary issues. 05:42 We'd had reduced pulmonary function and chronic lung disease patients really not doing well with the inhaled insulin. 05:49 That just kind of make sense – if you have less lung tissue to absorb the drug, you’re not gonna absorb the drug as well as a person with perfect lungs. 05:58 It is not recommended in patients who have diabetic ketoacidosis and the reason being is because the onset of action is not as predictable as an intravenous or subdermal insulin. 06:10 Finally, in smokers, we’re really not sure how well this is going to work. 06:15 Smokers can have any number of changes in the lung that can interfere with the absorption of insulin. 06:22 Now, it does cause a decline in lung capacity so we know that that the FEV has reduced in patients who were put on this medication and it also may cause an acute bronchospasm so those patients who are prone to things like asthma may actually have a triggering of their asthma. 06:39 Finally, there was a small but definite increase in lung cancer which I think has effectively quashed the market. 06:49 Not enough data on pregnant women, so we don’t know if this drug is safe, so we’re not recommending it at this point in time. 06:58 Now, this particular agent, all of the precautions that apply to insulin like be careful of hypoglycemia, be aware that patients who don’t eat are gonna be more prone to hypoglycemia because it still works even if you haven’t eaten – so all of those same precautions that we take with regular insulins or all of the insulins, you have to take with this insulin as well. 07:25 Glycemic excursions. 07:27 So in terms of glycemic excursions, we often worry about the spike after each meal, so the short-acting insulins are particularly useful for treatment of glycemic excursion. 07:39 When we give insulin we often, especially in our brittle patients, we will give a basal insulin that covers their 24-hour needs and then a meal time insulin that covers the excursion. 07:50 Now the excursions are often different between one meal and another. 07:55 Breakfast seems to have the greatest excursion and lunch seems to have the least, so often our dosing reflects that. 08:04 Sometimes, we’ll use two types of insulin – the long-acting insulin plus one short-acting and we only give that short-acting insulin at breakfast. It’s not very many patients but some of them actually respond quite nicely and they tend to have a nice sugars all day even though you’ve only given one short-acting dose. 08:25 Well, that’s it for the insulins. I hope that you found that useful. 08:28 If you are worried about your exams, don’t be. I know that you’re gonna do well. Show them what you know.
About the Lecture
The lecture Insulin Types and Glycemic Excursions – Diabetes Medications by Pravin Shukle, MD is from the course Endocrine Pharmacology. It contains the following chapters:
- Activity Profiles of Different Types of Insulins
- Glycemic Excursions
- Question: Drugs in Diabetes
Included Quiz Questions
What is NOT a short or rapid-acting insulin?
- Glargine
- Lispro
- Aspart
- Regular
- Glulisine
What is a characteristic specific to glargine?
- Does not have a peak time
- Lasts 12 hours
- Specially designed to prevent an allergic reaction
- Due to its formulation, glargine has multiple concentration peaks throughout the day.
- Lasts 48–72 hours
What best represents the term glycemic excursion in a patient with diabetes?
- Blood glucose values, usually postprandial, significantly exceed the 24-hour mean blood glucose value.
- The change in blood triglycerides when measured just before the start of a meal and just after a meal is finished.
- The change in blood cholesterol when measured just before the start of a meal and just after a meal is finished.
- The amount of insulin required to maintain blood sugar in an acceptable range, especially after meals.
- The distance aerosolized insulin must travel in the formulations of inhaled insulins.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like how Dr. Shukle delivered his lecture. I'm a medical student and this lecture is very useful. I'd probably finish the whole course today. Godspeed!
well structured and planned on teaching the course. Would recommend to others.