Playlist
Show Playlist
Hide Playlist
Dysmenorrhea in Adolescent Girls
-
Slides Dysmenorrhea Pediatrics.pdf
-
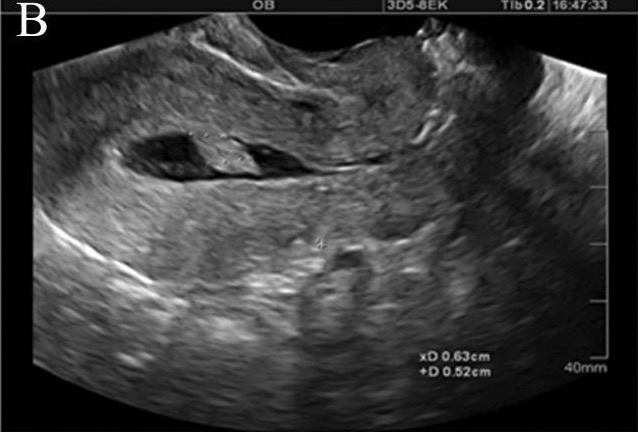
Download Lecture Overview
00:01 In this lecture, we will discuss dysmenorrhea in adolescent girls. So, painful menstruation is an incredibly common complaint in adolescent girls. About half of all girls will complain of this. 00:14 In 10%, it can be even debilitating for up to three days while they’re having their period. 00:20 This is the most common gynecological complaint from adolescent patients. 00:25 So, we have primary dysmenorrhea which has a clear physiologic etiology. There is no identifiable pelvic pathology. This is 90% of the cases where it just hurts. Then there’s secondary dysmenorrhea which is associated with an underlying pelvic pathology. This is in about 10% of cases. 00:48 So, let’s talk about primary dysmenorrhea first. Basically, patients have a release of prostaglandins from the endometrium after their progesterone withdrawal. This results in potent vasoconstriction and uterine contraction. That causes ischemia and pain. Secondary dysmenorrhea, however, can be caused by a number of underlying pathologic conditions. Examples include endometriosis, a congenital Müllerian anomaly, pelvic inflammatory disease, adhesions from a prior surgery, an ectopic pregnancy, ovarian cyst or ovarian torsion, or uterine fibroids, or the presence of an inserted uterine device or IUD. Any of these can cause dysmenorrhea. So, when we see a patient with dysmenorrhea, we want to make sure we take a good history. We want to interview the adolescent alone. This is true for all adolescent interactions. This is because in front of their parents, they may not be totally forthcoming with all of the issues that are affecting them. 02:00 So, we’ll want to ask them a few questions. Questions about what is the timing of this pain. 02:04 Can they describe the pain? Is it cramping or sharp? What are the symptoms present? Were the symptoms present since menarche or is it just a recent phenomenon? Do NSAIDs provide relief that’s common in a primary dysmenorrhea? Is there a previous abdominal or pelvic surgery that happened which will lead us towards perhaps some bands or something internally that’s causing a problem? Are they sexually active and are they appropriately using condoms? Do they have an IUD or do they have any other associated symptoms? Then we’ll want to do a complete physical exam for these girls. So, the physical exam on a patient with primary dysmenorrhea is usually completely normal. But if they have abdominal pain, we want to check and we will usually see a mild suprapubic tenderness especially during the period. We may see some rebound tenderness if there is a secondary cause or something else going on. The pelvic exam should be done to externally appreciate the genitalia and make sure there’s no lesions or any other problems. 03:12 Then we should do a bimanual exam. This is important to identify pelvic inflammatory disease with say, cervical motion tenderness. It’s also important to appreciate the adnexa to make sure there’s no ovarian mass or cyst or uterine malformation or fibroid. Lastly, a rectovaginal exam is done to evaluate for endometriosis. Lastly, we’ll want to do some diagnostic testing. Lab data is generally to rule out causes of secondary causes of dysmenorrhea. So for example, we’ll check a pregnancy test. 03:49 Do test for gonorrhea and chlamydia, or assess for nongynecologic pain such as doing a urine culture for UTI or check stool for other pathogens or check a CRP or a sed rate for some sort of underlying inflammatory condition. A pelvic ultrasound may be important if we’re worried about abnormalities of the Müllerian system. Likewise, laparoscopy could be helpful in severe cases of endometriosis. 04:17 So, how do we treat endometrial pain? Well, the first line is NSAIDs. Sometimes that’s enough. 04:24 In patients with severe periods, we can control them with oral contraceptives or alternatively, we could do injective prostaglandins. This typically can be done every three months. 04:36 Lastly, we can recommend other alternative therapies such as warm packs or acupuncture, although there’s limited data on the efficacy of these approaches. For patients with underlying pelvic pathology, this may require surgical intervention such as ablation of endometriosis during a gynecologic surgery or we may need to give them antibiotics to manage their pelvic inflammatory disease. 05:03 We may want to control endometriosis with oral contraceptive pills or if patients are having problems managing their endometriosis, we may turn to GnRH agonists as well. So, this is a brief review of how we approach dysmenorrhea in adolescent girls. Thanks for your time.
About the Lecture
The lecture Dysmenorrhea in Adolescent Girls by Brian Alverson, MD is from the course Adolescent Medicine. It contains the following chapters:
- Dysmenorrhea
- Physical Exam Findings
Included Quiz Questions
Which of the following is NOT a cause of secondary dysmenorrhea?
- Vasoconstriction due to endometrial prostaglandins
- Endometriosis
- Pelvic inflammatory disease
- Ectopic pregnancy
- Fibroids
Approximately what percentage of all cases of dysmenorrhea in adolescents is primary?
- 90%
- 50%
- 30%
- 40%
- 10%
Which of the following is the most appropriate 1st-line pharmacotherapy in a 13-year-old girl with primary dysmenorrhea?
- NSAIDs
- Oral contraceptives
- Acetaminophen
- Transdermal patch
- Selective serotonin reuptake inhibitors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It makes very clear a topic which was not so clear for me before. Thank you!