Playlist
Show Playlist
Hide Playlist
Stroke: Pathophysiology
-
Slides Stroke and intracranial hemorrhage.pdf
-
Download Lecture Overview
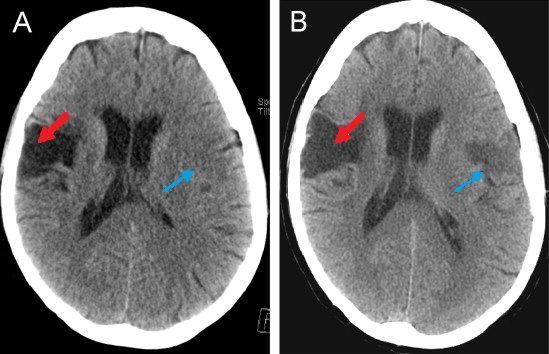
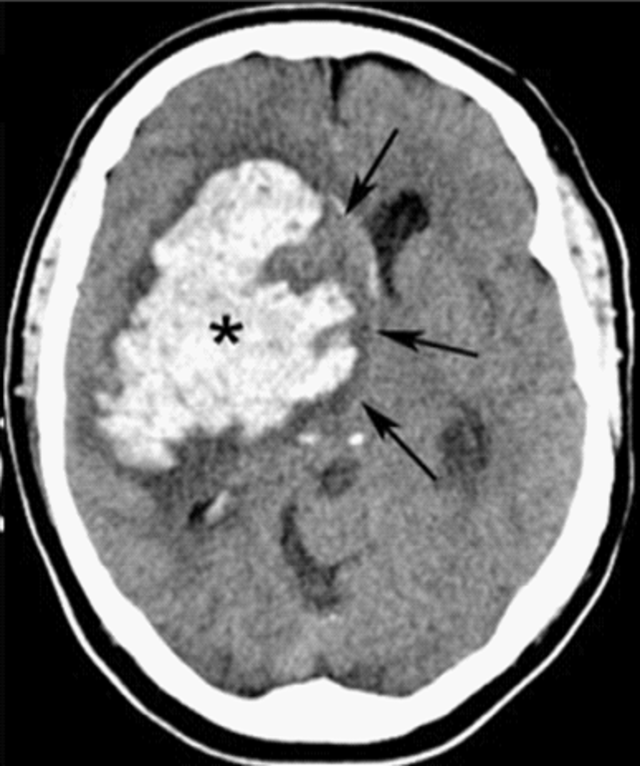
00:01 But let's turn a little bit to understand what's going on at the level of the brain in patients who suffer an ischemic stroke. 00:08 When we think about the brain, the brain tissue requires constant perfusion. 00:12 About 20% of all cardiac output will be diverted up to the brain through the carotid arteries, and it's very critical that the brain receives adequate blood flow and blood supply, that's both for nutrient delivery and clearing toxic substances. 00:27 When I think about stroke, I like to think about the amount of blood flow going to each part of the brain in that area of ischemia or infarction. 00:36 We see here that normally, for normal brain function, the brain requires sufficient cerebral blood flow or CBF. 00:44 We measure CBF or blood flow based on the milliliter per milligram of brain per minute of perfusion, and normally somewhere between 50 and 55 or greater than 50 milliliters per milligram per minute of cerebral blood flow is sufficient and required for normal brain function, that brain is going to do exactly what it should. 01:06 When blood flow is reduced, and when we see blood flow in the range of 30 to 35 mL per mg per minute, we start to see that brain tissue can become dysfunctional in some way. 01:18 The cells are quiescent, we can see normal cellular processes, sodium-potassium channels work, there's exchange of ions, but the cells won't do what they're performed to do and we can start to see neurologic dysfunction and patient symptoms in those quiescent areas that are at risk of further ischemia if the blood clot is not intervened upon. 01:42 As blood flow continuous to drop as we enter that core area of infarction in an ischemic stroke, we see blood flow drops to 15 to 20. 01:51 Blood flow of less than 18 is what's considered required and necessary for penumbric tissue. 01:57 This is tissue that does not work, we're starting to see loss of normal cellular function, normal-sodium potassium channels, and if the clot is not intervened upon penumbric tissue will die and become infarcted. 02:11 When we look at intervening in an acute stroke, we're trying to save that penumbric tissue and that's our critical goal. 02:18 Patients will have symptoms from areas of ischemia and penumbra, low blood flow and we want to restore that to bring their symptoms, resolve their symptoms and bring their function back. 02:30 And then as blood flow continuous to drop in the center of the core of that area of ischemia and really of infarction, we see infarcted tissue. 02:38 When blood flow drops below 10 mL per mg per minute, tissue dies and we begin to see the lack of ability to recover that cellular function and that neurologic function in those patients. 02:52 We're looking to keep the infarcted core as small as possible and save as much penumbra when managing patients with an acute stroke. 03:00 Biochemically, there are also changes that occur as cerebral blood flow drops, and here you can see a list of a number of those changes. 03:09 We don't really need to remember all of these details and I'll walk you through some of the critical things that are both clinically relevant and important when understanding clinical vignettes. 03:19 There are morphologic change that we see as penumbric tissue becomes inflamed with reduced blood flow and then ultimately infarcted and dies, and you can see the biochemical changes that are occurring within the cell, as we get increasing reduction in blood flow. 03:36 Let's dive into this deeper and we're going to walk through the steps of what happens at the level of the cell in the setting of an ischemic stroke. 03:45 And we're going to walk through some of the steps, ischemia, infarction, cytotoxic edema, ionic edema, vasogenic edema, and necrosis; and I think these are important to understand and clinically relevant, because we will do different interventions at different times to try and rescue and reverse this process or visualize what's going on. 04:07 Normally, we see or hear in the brain, there are endothelial cells with a patent lumen, blood flowing through. 04:14 We see interstitial space that surrounds the neurons and astrocytes, and sodium channels are contained in their, along their appropriate concentration gradient so that neurons are able to fire. And this is the normal condition. 04:28 In the setting of an acute infarct, we see a blockage to the blood vessel. 04:32 There is reduced perfusion and blood no longer perfuses or goes to that area of brain. 04:39 One of the first things that happens is the loss of sodium-potassium channels, and sodium-potassium channel function on the surface of neurons, astrocytes and all of the cells in that area of reduced blood flow and perfusion. 04:53 Sodium-potassium channels are important for giving all cells energy, and when cells lose perfusions, that's one of the first things that starts to be dysfunctional. 05:03 We see increase in sodium within the cell and the cells begin to want to swell as water wants to follow sodium across it's concentration gradient. 05:15 So the second thing that happens is an influx of water into the cells and we can see here within this neuron, it's loss sodium-potassium ATPA's function. 05:25 Sodium has moved into the cell and water is now following and the cells are swelling. 05:31 We call the process cytotoxic edema or cellular edema, and this is really important. 05:36 The cytotoxic edema begins immediately at the time of an ischemic infarct and that's what we're looking at when look on an MRI scan. 05:45 This is how we're visualizing the territory of infarcted tissue. 05:49 Next, we see a shift from cytotoxic edema to ionic edema. 05:55 In this phase of the stroke, we start to see water that begins to be pulled into the brain. 06:01 There's some controversy around where the water's coming from. 06:05 Convention suggest that water's being pulled from inside the blood vessels, but the CSF space is also an area of copious fluid and we may see some influx of water from the CSF space. 06:17 Regardless, we see sodium increase in the interstitial space and then water follow sodium, so water begins to infiltrate into the interstitium, in and around the neurons and the astrocytes. 06:30 There's increased compression and we are beginning to see some swelling of the brain. 06:35 This is also important that early ionic edema is what we look for on a CT scan to indicate a developed stroke, a stroke that is beyond that acute intervention stage and has reached the second stage of ionic edema. 06:51 Next, we see movement towards vasogenic edema. 06:54 As the stroke evolves, the blood vessels began to become dysfunctional and break up and necrose, we also see that at the level of the neurons and the astrocytes. 07:04 The cells have lost their ability to maintain energy and their cellular function and membranes, and the cells began to lyse and apoptose. 07:12 As that happens, the blood vessels becomes leaky and we see water able to rush down it's osmotic gradient from inside the blood vessel to out in the interstitium. 07:23 Vasogenic edema is edema or swelling that comes from the blood vessel, it's vasogenic. 07:29 This increases the total amount of volume in the brain and as a result, we can see cerebral edema, mass effect in the brain, and in severe cases, herniation midline shift and patients can die from that degree of increased in pressure on the brain. 07:46 This occurs later after a stroke and we'll talk about that timeline, three to five or up to seven days after a stroke, and this is a critical period to monitor patients. 07:56 Overtime we see that process continues. 07:59 The cells continue to die and we can see areas of necrosis. 08:03 This occurs late after a stroke and at that point, seven days, sometimes up to 10 days, if this area is re-perfused, we can see a risk of hemorrhagic transformation, through those leaky blood vessels and capillaries and in to this necrotic debris, we can see infiltration of blood in large territory of hemorrhage, and that is also a critical window to be mindful of and evaluate for patients. 08:31 So, let's take a look at that table format and understand how this pathophysiology in the understanding of stroke physiology, helps us to manage and intervene in patients. 08:42 We said the first thing that happens is ischemia. 08:45 The cells are not dead, the sodium-potassium channels are starting to not work, but there is still some cellular function. 08:51 And this is when acute intervention is important. 08:54 We will learn that time is brain, and the time we're talking about is preventing that ischemic tissue which can be saved from becoming infarcted tissue. 09:03 The second process that's happening early within minutes of the blockage of the blood vessel is that core area of reduced perfusion will become infarcted. 09:14 This is where we want to intervene as quickly as possible, and if not able to, that infarcted core will begin to expand. 09:21 The next step within the first few hours, or starting within minutes and extending out to the first several hours to days of the stroke is the cytotoxic edema, and this is what we look at on the MRI. 09:33 On MRI, we look at diffusion-weighted image and the diffusion-weighted image is sensitive at finding areas of cytotoxic edema, of cell swelling. 09:43 When the cell swell, they become packed, there's poor movement of water, there's poor diffusion of water, and the diffusion weighted images look for diffusion. 09:52 When diffusion is abnormal, we see that in that on that MRI that diffusion weighted image, and that's what we use to diagnose and evaluate the extend of stroke later on we start to see ionic edema and then vasogenic edema and necrosis and now you can see here that process beings at day 1 extends out to day 5 or 7 with vasogenic edema and we see necrosis even beyond that. 10:17 And that's a critical period to evaluate patients particularly those with large territory strokes. 10:22 The larger the territory, the larger the vasogenic edema. 10:26 The larger the territory of stroke the more necrosis. 10:29 And for those patients there's a higher risk of edema swelling mass effect and herniation in the five to seven day period, and ultimately, hemorrhagic transformation, seven to even more days after that. 10:40 So, importantly, we can see from this table how a stroke evolves overtime. 10:46 When we're thinking about intervention, one of our goals is to reduce the size of the stroke, prevent the stroke from happening, and prevent this cascade of events from being initiated. 10:58 If we can do that, if we can reduce infarction or prevent infarction and reduce the size of ischemia, we won't see this downstream cascade occur.
About the Lecture
The lecture Stroke: Pathophysiology by Roy Strowd, MD is from the course Stroke and Intracranial Hemorrhage.
Included Quiz Questions
What is the normal rate of cerebral blood flow?
- Normal CBF is > 50 ml per 100 g brain tissue per minute.
- Normal CBF is > 10 ml per 100 g brain tissue per minute.
- Normal CBF is > 30 ml per 100 g brain tissue per minute.
- Normal CBF is > 75 ml per 100 g brain tissue per minute.
- Normal CBF is > 100 ml per 100 g brain tissue per minute.
What is described by the term "penumbral tissue?"
- An area of ischemic tissue surrounding the tissue affected by a stroke that is still potentially salvageable
- An area of normally perfused brain tissue
- An area of non-functioning brain tissue that has suffered infarction due to a stroke
- An area of the brain that has previously been affected by a stroke
- An area of brain tissue that has not been affected by a recent stroke
What is a very serious complication due to brain edema and mass effect after a stroke?
- Brain herniation
- Sodium/potassium channel dysfunction
- Penumbral tissue transformation
- Venous sinus thrombosis
- Thalamic infarction
How long after a stroke is the greatest risk of hemorrhagic transformation due to reperfusion?
- Hours to days after the event
- Days to weeks after the event
- Weeks to months after the event
- Months to years after the event
- Seconds to minutes after the event
What is meant by the phrase "time is brain?"
- Acute intervention during a time of cerebral ischemia can prevent a brain infarction and its associated clinical manifestations.
- Acute intervention after a brain infarction can prevent the extension of the stroke.
- Prevention of a stroke by risk factor modification saves brain tissue.
- Acute intervention after a brain infarction can prevent hemorrhagic transformation.
- Human brain tissue is rapidly and irretrievably lost as a stroke progresses and therapeutic intervention cannot prevent deterioration.
After acute occlusion of a cerebral blood vessel, what is the next step in the cascade of events?
- Sodium/potassium channels in the cells become dysfunctional
- Water influx into brain cells causes edema
- Brain swelling is seen on CT or MRI imaging
- Blood vessels become dysfunctional causing vasogenic edema and apoptosis
- Infarction and necrosis of brain tissue result
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I loved how he took his time breaking the pathophysiology of the ischemic stroke in a way that I don't need to look up any terminology to understand him better