Playlist
Show Playlist
Hide Playlist
Step 2: Options for Diagnostic Testing and Clues to Severe Disease
-
Slides Headaches Introduction to Headaches.pdf
-
Download Lecture Overview
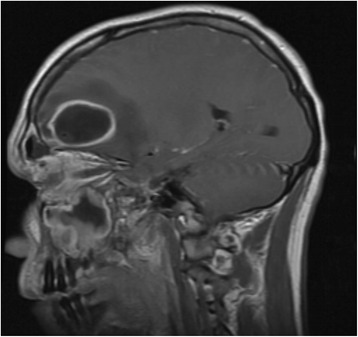
00:01 And so those are some of the clinical features that we use to drive in on the paroxysmal headaches, and that gets us to our next step, our second step in the evaluation of these patients, do I need imaging? Do I need to intervene acutely now or can I move right to treatment based on my clinical suspicion from the history and physical exam? And the answer to this is yes, you do need to do imaging and additional evaluation or intervention if the patient may be suffering from a secondary cause of headache. 00:30 If it's a primary headache syndrome, we often move past imaging evaluation and acute intervention to treatment. 00:36 So, what are some of the interventions and evaluations that we would do for secondary causes of headache? Well, again, we can think about those based on those categories that we recently discussed. 00:47 For thunderclap headache we'd look for subarachnoid hemorrhage with the CT, a non-contrast CT or dissection with CTA imaging, CT angiography, or a lumbar puncture to evaluate subarachnoid hemorrhage, so we'd look for those potential causes of thunderclap headache. 01:02 For headache with vision disturbances ESR, CRP are used to evaluate for giant cell arteritis. 01:07 For the neuralgiform headaches we often do an MRI of the brain, sometimes with the MR angiography to look for a blood vessel or an aneurysm that may be pushing on a nerve, pushing on the trigeminal nerve and causing trigeminal neuralgia, or on another nerve, a cranial nerve that's causing a neuralgiform headache. 01:25 And then for high and low pressure headaches, we typically think about MRI imaging for tumors. 01:30 MRI is important to evaluate for pseudo tumor which we'll learn about in another lecture and venous sinus thrombus, a clot within a blood vessel, can be seen with an MRI or MR venography which we often conduct. 01:42 So that's some of the test that we would do to evaluate emergently for a secondary cause of headache. 01:48 And we can think of this in the opposite way. 01:50 We can think about some of the test that are available to us in the headache types that they would evaluate. 01:54 Imaging like CT and MRI are important for evaluating tumor, hydrocephalus, increased intracranial pressure, hemorrhage, venous sinus thrombosis, vascular malformations, and sinusitis. 02:06 Lumbar puncture looks for things in the CSF space, so subarachnoid hemorrhage, encephalitis or meningitis, and then benign intracranial hypertension, that's where the CSF is not abnormal, there's non-infection or blood, but there's increased pressure because of increased CSF production and this presents with a high pressure headache. 02:27 And then, low pressure headache or intracranial hypotension is diagnosed with low pressure as evaluated by the opening pressure on a spinal tap or lumbar puncture. 02:36 Angiography can evaluate some of the vascular causes, aneurysmal subarachnoid hemorrhage and that reversible cerebral vasoconstriction syndrome, that can present with a thunderclap headache. 02:47 ESR, CRP, or blood test, temporary biopsy can be used to evaluate for giant cell arteritis. 02:53 Polysomnography is a test we'll do for some patients that have paroxysmal headaches that could be from obstructive sleep apnea, and then, rarely, we'll do EEG or skull films, but those are primarily not used in the evaluation of headache and just in very rare selected cases. 03:08 What are some of the clues to more serious causes of headache that require acute intervention? And this list is not something to memorize in detail, but some things to be thinking about when evaluating patients or clinical vignettes that would clue us into acutely evaluating the patient. 03:26 The sudden first or worst headache of someone's life. 03:29 Simultaneous or subsequent neurologic deficit so headache with a neurologic deficit either at the same time or in close proximity. 03:39 Focal neurologic deficits or signs of increased intracranial pressure. 03:43 Fever, meningeal signs, a headache that is side-locked, that is only on one side needs to be evaluated for underlying structural cause, but then maybe from a paroxysmal headache, like the ones that we talked about. 03:57 Onset after age 50, new onset headache in someone over the age of 50 is a tumor until proven otherwise and requires imaging. 04:05 Vomiting days to week before the headache suggest high pressure headache or some type of mass lesion. 04:11 Altered consciousness always requires imaging because we can't trust the patient's history often because the patient doesn't able to provide it. 04:19 Behavioral changes. Paroxysmal hypertension could suggest some other secondary cause. 04:25 Endocrine changes could suggest a problem in the pituitary or sellar region that could be a tumor or a venous abnormality or a vascular abnormality that needs to be evaluated with imaging. 04:36 Onset after Valsalva, Valsalva or bearing down in- reduces the venous flow out of the brain, increases the stuff, the veins, the CSF, the brain that is in the cranial vault, and suggest a high pressure cause of headache. 04:51 Onset with change and position suggest may be a high or low pressure headache. 04:55 Changing in the pattern or response to therapy, something that previously responded in therapy, but isn't currently. 05:01 And something that's just not a standard syndrome, those are the things that require additional evaluation and they should prompt emergent or urgent imaging. 05:09 And so, in summary, some of the headaches that require imaging are the first and worst, the headaches with papilledema, headache with focal neurologic findings, headache with fever and neck stiffness, and headache after trauma. 05:23 Those five conditions should really prompt us to think about imaging and the important take homes from that list that we just reviewed.
About the Lecture
The lecture Step 2: Options for Diagnostic Testing and Clues to Severe Disease by Roy Strowd, MD is from the course Headache.
Included Quiz Questions
What test or tests are indicated in the evaluation of a patient with a headache that is concerning for giant cell arteritis?
- ESR, CRP
- MRI
- CT scan
- Lumbar puncture
- Angiography
What is essential in evaluating a patient with a suspected subarachnoid hemorrhage?
- Lumbar puncture
- Polysomnography
- EEG
- ESR, CRP
- X-rays
What symptom associated with headache indicates the need for urgent imaging with CT or MRI?
- Papilledema
- Photophobia
- Nausea and vomiting that occur with a patient's headache
- Visual aura
- Onset at age 18 with no prior headache history
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |