Playlist
Show Playlist
Hide Playlist
Step 1: Primary and Secondary Headaches and Types of Headaches
-
Slides Headaches Introduction to Headaches.pdf
-
Download Lecture Overview
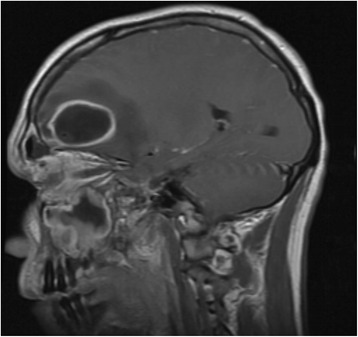
00:01 The first step is, is this a primary or secondary headache syndrome? So what do we mean by that? Well, a primary headache syndrome is one where the headache doesn't come from any underlying pathology, there's not a cause for the headache, it's just there, and typically we're going to focus on treating it. 00:18 That's different from a secondary cause of headache or a secondary headache syndrome where there is a cause, and our number one job is to find that cause, what's causing the headache and manage it, either medically or surgically. 00:30 What's the etiology for these, well primary headache syndromes have no known etiology, they're primary. 00:37 There's an unknown etiology, they're coming from something related around the brain and we need to focus on treatment and not what's the cause. 00:43 That's different from the secondary headache syndromes which often have an underlying etiology and our job is to figure that out. 00:50 If we think about what these require, a primary headache syndrome typically does not require imaging evaluation or emergent evaluation or additional diagnostic testing, and we focus on treatment. 01:01 Whereas with secondary headache syndromes, our job as clinicians, is to figure out what imaging test or what evaluation or what intervention do we need to do and we'll approach clinical vignettes similarly. 01:12 As I've said, our focus for primary headaches is typically on treatment, whereas, for secondary headache syndromes it's diagnosis first and then treatment. 01:20 The epidemiology of these, the vast majority of headaches are primary headaches. 01:26 They're migraine or tension type or cervicogenic headache or obstructive sleep apnea, that's the majority of headaches. 01:32 Secondary headaches are rare, but they can be life-threatening so we need to know how to focus on those, evaluate them, diagnose them, and treat them. 01:40 And some of the examples of the primary headache syndromes, as I've said are migraine, tension type, and cluster headache, of secondary headaches are brain tumor, subarachnoid hemorrhage and glaucoma. 01:50 And we can use this to categorize those questions that we ask patients. 01:56 And when I'm asking questions to a patient or questions on a clinical vignette, we start with our questions to look for secondary causes of headache. 02:04 The emergent or thunderclap causes which are secondary causes that we need to evaluate and explore. 02:09 Headaches with vision disturbances often have an underlying cause that will need to find. 02:14 The neuralgia formed headaches we should look for a potential cause, and high and low pressure headaches, often have a secondary cause that must be explored. 02:22 And that's different from the paroxysmal headaches which are often primary headache syndromes, but the last of the questions that we ask the patients, and typically, our focus then becomes treatment as oppose to diagnostic investigation. 02:33 So let's walk through some of the causes of these different categories of headaches, and think about what we're going to do to evaluate those or to treat those. 02:42 In that emergent and thunderclap group of conditions, we think of subarachnoid hemorrhage, sentinel bleed, epidural or subdural hematomas, RCVS, which is reversible cerebral vasoconstriction syndrome, and presents with headaches and sometimes focal neurologic deficits. 02:59 Arterial dissection and giant cell arteritis, these are emergent problems. 03:03 We need to evaluate these and diagnose them quickly so we can manage the patient appropriately. 03:09 What about headaches with vision disturbances, giant cell arteritis and glaucoma are the two prominent causes of headache, where there are oft, also prominent visual changes, either blurry vision or a loss of vision or an altitudinal defect where patients can't see above or below the meridian, or a really red swollen painful eye in glaucoma. 03:28 Causes of a neuralgiform headache include occipital neuralgia, trigeminal neuralgia, and glossopharyngeal neuralgia. 03:35 Glossopharyngeal neuralgia actually doesn't always present with headache and sometimes can present with syncope, but it's an important neuralgiform condition that can cause headache. 03:44 And then any nerve can become irritated or dysfunctional, we can have supraorbital neuralgia or preauricular neuralgia, and all of those present with neuralgiform pain. 03:53 Numbness, tingling, and paresthesias that are prominent symptom complex. 03:57 As well as zoster and herpes can affect the face and present with headache. 04:02 What about the pressure headaches? What conditions fall on those categories? Where there can be low pressure and high pressure headaches? Low pressure typically comes from intracranial hypotension, too little CSF in the cranial vault, that can develop from a dural tear in the spine, in the spinal cord, and the spinal fluid slowly leaks out of the spinal cord, there's less CSF in the cranial vault and patient present with low pressure headaches. 04:29 When they stand up the headaches bad, when they lie down, the headache is much better, that positional component. 04:35 And then, there are also high pressure causes. 04:37 A tumor is extra mass on the brain and causes too much pressure and head pain. 04:42 There's pseudo tumor cerebri, which we will learn about, and venous sinus thrombosis which is a blood clot that causes too much blood, venous blood, in a backup of blood contributes to pain. 04:55 And then that last category, paroxysmal headaches, we divide into those with prominent autonomic findings, and then those without autonomic findings. 05:03 The autonomic paroxysmal headaches are the TACs, the trigeminal autonomic cephalalgias, and that includes cluster headache, paroxysmal hemicrania, and SUNCT, short lasting unilateral neuralgiform headache with conjunctural injection and tearing. 05:19 And then the non-autonomic headaches include migraine, tension type, cervicogenic headache, chronic daily headache, and they're a number. 05:28 So this is a good categorization of scheme we can use to approach patients and clinical vignettes and understand how to organize all of those many causes of headache. 05:39 What are some of the paroxysmal causes of headache? The chronic recurrent headache syndromes and how might we go about diagnosing them based on clinical exam, because the clinical exam is really what's going to tell us that this is a paroxysmal headache and we're going to focus on treatment, and we'll just summarize some of those common causes in the clinical features that point us in that direction. 06:01 So first is migraine. This is often a unilateral headache, a pressure pain that presents with prominent photophobia. 06:09 The pain is worsened or brought on or induced by bright lights or loud noises, photo and phonophobia. 06:15 Patients typically have prominent nausea and vomiting. 06:18 Patients may have an aura prior to the onset of headache. 06:21 They may have visual disturbances, where there's a scotoma, a black spot in their vision that they can't see or a scintillating scotoma, around that dark spot is bright wavy lines. 06:32 That aura often proceeds the head pain and tells us that the patient may develop head pain. 06:37 Importantly with migraine, we don't see autonomic findings as prominently as some of the other conditions that we'll talk about. 06:44 No lacrimation or rhinorrhea, stress increases these headaches and they can response to triptans which is an abortive treatment. 06:51 Migraine differs from tension type. 06:53 Migraine is often characterized by photophobia, phonophobia, even osmophobia. 06:59 Headaches, they're induced by different changes in smells or putrid, pungent smells, and migraine has prominent nausea/vomiting in aura, we see none of those typically being the case for tension type, no photophobia, phonophobia, nausea, vomiting or aura, we just don't see those findings. 07:17 Tension type headaches tend to be bilateral, a band-like sensation around the head which you can see on the schema here and often not prominent autonomic features like lacrimation or rhinorrhea. 07:28 Those headaches differ from cluster headache, which we'll learn about and cluster headache is not one of the migraine variants. 07:36 It doesn't, we don't tend to see photophobia, phonophobia, nausea, vomiting, and aura, those typical features of migraine. 07:43 But it is a paroxysmal headache where we see prominent autonomic features. 07:47 So patients have lacrimation, rhinorrhea, conjunctival injection, prominent autonomic features that are usually locked to the same side as this unilateral headache which is often positioned behind the eye. 07:59 Again, as you can see in the schema, this is strictly unilateral headache. 08:03 It can respond to triptans as well as oxygen and not indomethacin. 08:08 Cluster differs from hemicrania continua. 08:11 Hemicrania continua is a unilateral headache, just like a cluster. 08:16 We can see some of those migrainous features, photo/phonophobia, nausea, vomiting, though as not prominent often as migraine. 08:23 It is an autonomic cephalalgia, so patients have lacrimation and rhinorrhea and strictly unilateral. 08:30 Hemicrania continua though differs because it is indomethacin responsive and that indomethacin response is an important diagnostic and therapeutic intervention for these patients. 08:42 What about some other rare and kind of more fun causes of headache that are important to know, so when you diagnose patients with these rare conditions, there's a condition, primary stabbing headache, this is exactly like it sounds. 08:56 It is a very quick, sharp, stabbing pain like a knife being dug into the brain that presents with short stabs and clustered episodes of a stabbing pain, and it is indomethacin responsive, an important, again, diagnostic and treatment intervention. 09:13 Exertional headache as it sounds, it's a headache induced by absorption or stress. 09:18 It can be an indomethacin response so it shouldn't be confused with hemicrania continua or primary stabbing headache and varying degrees of nausea, vomiting, photophobia as many of us may have experienced.
About the Lecture
The lecture Step 1: Primary and Secondary Headaches and Types of Headaches by Roy Strowd, MD is from the course Headache.
Included Quiz Questions
What is an example of a secondary headache?
- Headache due to a brain tumor
- Migraine headache
- Headache due to stress or tension
- Headache due to alcohol withdrawal
- Cluster headache
What is an example of a neuralgiform headache?
- Headache due to herpes zoster/shingles
- Migraine headache
- Tension headache
- Cluster headache
- Headache due to a brain tumor
What type of headache is described as chronic, recurrent, unilateral pain associated with sensitivity to light and sound, often accompanied by nausea and vomiting?
- Migraine headache
- Cluster headache
- Headache due to a brain tumor
- Headache due to sleep apnea
- Trigeminal neuralgia
What type of headache is described as unilateral facial/head pain associated with lacrimation and rhinorrhea, and responds to oxygen therapy?
- Cluster headache
- Migraine headache
- Headache due to a brain tumor
- Tension headache
- Primary stabbing headache
What is the most common type of primary headache?
- Tension headache
- Headache due to sleep apnea
- Migraine headache
- Trigeminal neuralgia
- Cluster headache
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |