Playlist
Show Playlist
Hide Playlist
Osteoporosis: Introduction & Causes
-
Slides Osteoporosis EndocrinePathology.pdf
-
Download Lecture Overview
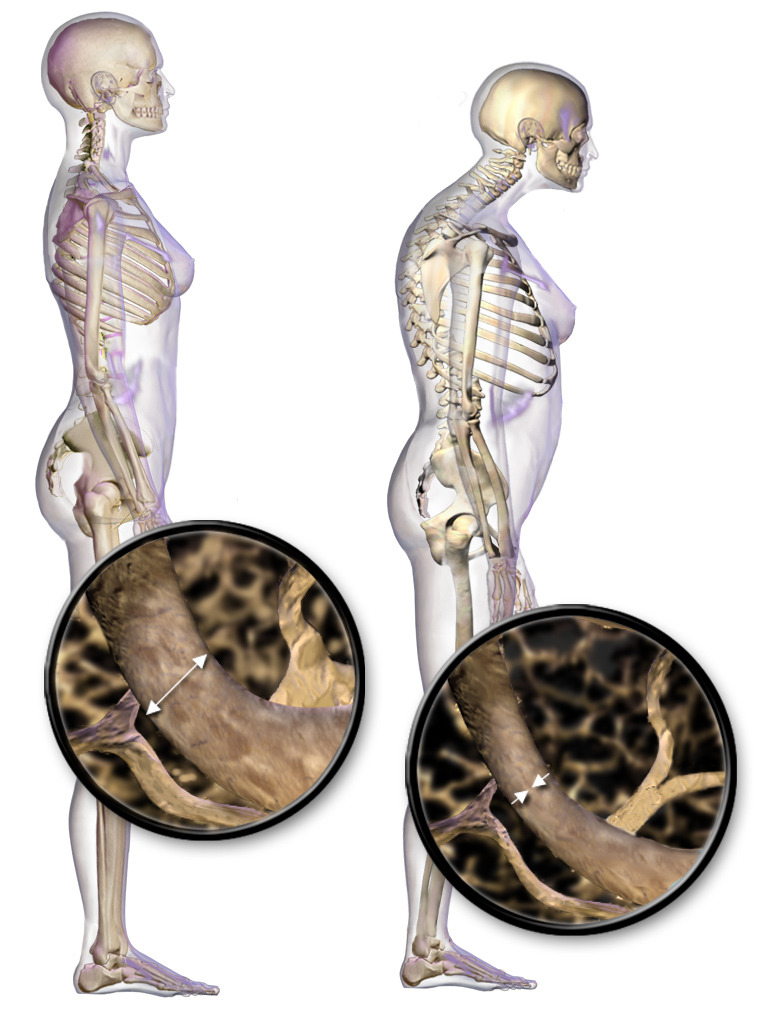
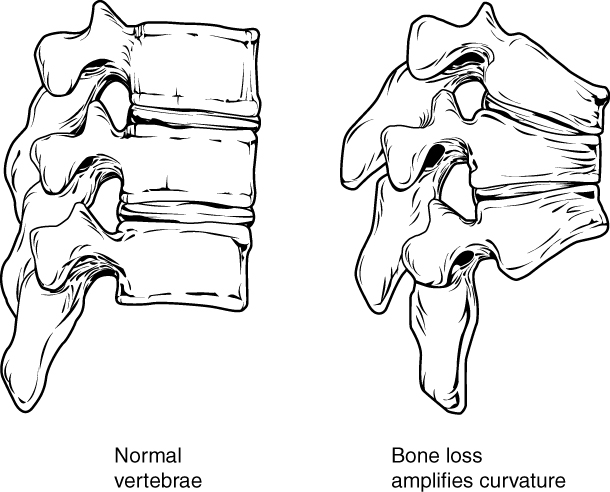
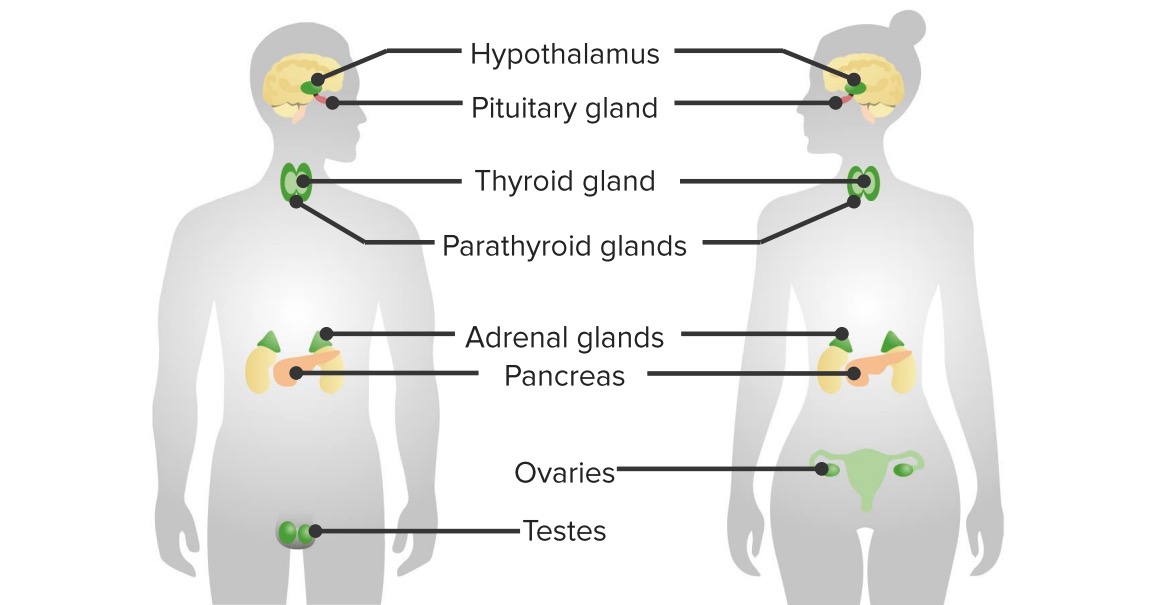
00:01 Topic here is osteoporosis. 00:04 Allow the name to speak to you. 00:06 Increase in porosity within the bone, what may then cause it? Well, to begin with, take a look at the picture on the left and we notice that, here, that the bone and the trabeculae and such… oh, everything is intact. 00:22 On the right, you’ll notice that this kind of looks like a beehive. 00:26 What that basically means is that you have your trabeculae that get very, very thinned out. 00:31 Think of this perhaps as being in the vertebrae and if this type of thing... thinning is taking place in the trabeculae with all these pressure upon the vertebrae, you might then have [sound] compression fracture because of weakening, weakening, weakening. 00:45 So, with osteoporosis, it’s skeletal disorder characterized by compromised bone strength predisposing to increased risk of fracture, maybe perhaps compression factor of the vertebrae. 00:59 Bone remodelling, what does that mean to you? Well, last time I talked about this was the balance between osteoclasts and osteoblasts. 01:06 This is absolutely required so that you have proper bone integrity. 01:10 The equilibrium between the formation of… by osteoblasts and the resorption, meaning to say, removal of the calcium from the bone by osteoclasts. 01:18 Well, that balance has been lost and when such an imbalance takes place, why? Well, maybe a female, as you know, as she hits menopause at the age of 50, she has decreased estrogen. 01:31 So, therefore, this decreased protection of the bone may result in imbalance… osteoporosis. 01:36 Usually, on average, a peak bone mass is achieved by 30; anything after that, well, it depends on how the patient has been taking care of himself or herself. 01:48 Around the fourth and fifth decade, later on, so we’re talking about 40’s and 50’s, the bone loss occurs automatically due to age at approximately 0.5 percent per year. 02:00 Loss is accelerated in women due to loss of estrogen and the reason for that is, if you remember your pharmacology here, there’s a particular drug called denosumab, I would recommend that you go back and take a look at that drug. 02:12 It is a drug that actually binds to RANK ligand and what I mean by that is remember receptor activated nuclear kappa Beta, RANK, responsible for proper osteoclast activation or osteoclastogenesis. 02:28 What RANK ligand blockers do is not form excessive osteoclasts. 02:37 Estrogen helps to block or control the amount of osteoclastogenesis that’s taking place. 02:44 Therefore, osteoporosis is not a big deal during reproductive age in a female. 02:52 Once the female hits menopause, estrogen drops. 02:54 Therefore, for the protection or the regulation of osteoclastogenesis has also been lost. 03:00 May then result in loss of trabeculae, we call this micr- oh, osteopenia and then may result in microfractures and also compression fractures, especially of the vertebrae. 03:11 And of course, whenever you’ve heard of osteoporosis, you’re always worried about this elderly female who may then slip and fall maybe because she’s out shovelling the snow in the winter and she slips on ice and when she does, she has… experiences a hip fracture.
About the Lecture
The lecture Osteoporosis: Introduction & Causes by Carlo Raj, MD is from the course Bone Disease.
Included Quiz Questions
Which statement best describes the process of bone remodeling in osteoporosis?
- Imbalance in bone remodeling favoring osteoclast activity
- Decrease in estrogen leading to increased osteoblast activity
- Bone remodeling that results in the deposition of large amounts of weak bone material
- Inability to mineralize an osteoid
- Increased osteoclast activity due to increased estrogen levels
How is estrogen protective of bones?
- It controls the number of activated osteoclasts.
- It stimulates bone resorption.
- It helps to control calcium homeostasis without bone resorption.
- It increases in later decades of life.
- It increases the expression of RANK-L.
What is NOT a characteristic of osteoporosis?
- Pancytopenia
- Loss of microarchitecture of bone
- Loss of trabeculae
- Microfractures
- Compression fractures
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |