Playlist
Show Playlist
Hide Playlist
Trauma: Initial Survey and Management
-
Slides InitialSurveyandManagement Surgery.pdf
-
Download Lecture Overview
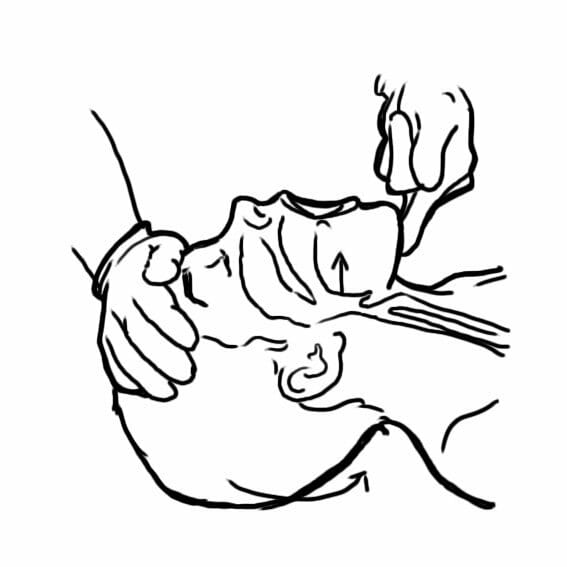
00:01 Welcome back. 00:02 Thanks for joining me on this discussion of the initial survey and management under the section of trauma. 00:08 Right off the bat to let you know, trauma is a very favorite question of the USMLE examination. 00:13 So we’re going to spend a fair amount of time discussing possible injury patterns. 00:19 Let’s start with a clinical scenario. 00:21 You’re presented with a 32-year-old man who is drinking alcohol and sustained a front-end collision with an incoming traffic. 00:30 Here is what his car looked like after the fact. 00:33 What’s going on in your mind? The question is, “Did the passenger make it?” I’ll give you a few seconds to think about this. 00:45 In trauma, no matter how severe or the mechanism of injury, we always follow the ATLS protocol or the Advanced Trauma Life Support System and the priorities are easily delineated for us using alphabets. 01:02 A for airway, B for breathing, and C for circulation. 01:08 Let’s stop for a moment. 01:10 In the initial survey and management, there are hard stops. 01:15 At every step along the way, we don’t move on to the next system if something needs to be addressed. 01:23 For example, if the airway is not intact, one needs to obtain a definitive airway before moving on to the next step in sequence. 01:34 A, again, is for airway. 01:37 In assessing airway, we are evaluating the patency of the airway delivery conduit. 01:42 This includes the mouth, the posterior pharynx, upper airways, and the trachea, and several divisions of the trachea. 01:52 What can potentially compromise the airway? A patient who has a Glasgow Coma Scale of less than 8. 01:57 We’ve all reviewed the Glasgow Coma Scale, but the Glasgow Coma Scale is basically an assessment of the patient’s neurological status. 02:06 Additionally, clear and obvious facial trauma particularly with active bleeding may pose a risk for an airway compromise. 02:14 And lastly, direct laryngeal trauma such as a hanging victim or direct blow to the neck can cause compromised airway. 02:23 Additional risk of airway compromise is a burn patient. 02:30 To secure an airway, we first bag mask the patient. 02:34 Bag masking the patient allows us to deliver oxygen. 02:39 Remember, there is a disadvantage of bag masking a patient. 02:42 Significant amounts of air enters the stomach and poses a threat to vomiting patients. 02:48 We then achieve definitive airway by performing an endotracheal intubation. 02:55 Sometimes, endotracheal intubation is impossible. 02:59 In which case, we would have to do an emergency surgical cricothyroidotomy as depicted by this image. 03:07 A needle or a knife is inserted through the cricothyroid membrane. 03:13 Remember, cricothyroid membranes, in neck anatomy, is actually named from a caudal to cranial direction. 03:22 Next, after airway has been ascertained, we move on to breathing. 03:26 B for breathing. 03:29 In breathing, we are evaluating whether or not the patient is moving air to allow ventilation. 03:35 Just because the patient has an intact airway, meaning the conduit is not obstructed, does not necessarily mean that the patient is actually moving air through the conduit. 03:47 What are some reasons why someone might not be moving air despite having an intact airway? For example, a very high spinal cord injury can render the diaphragm paralyzed. 03:58 Somebody who has significant traumatic brain injury may be comatose or have their respiratory centers damaged. 04:06 Injury to the diaphragm or the ribs can significantly alter the patient’s ability to move air. 04:11 When you have secured airway and ascertained the breathing or patient is moving air, we then move on to C for circulation. 04:21 In circulation, we evaluate the heart’s ability to pump blood and oxygenate or perfuse the tissues. 04:28 How do we evaluate circulation? Well, quick checks of mental status. 04:33 If the patient is oriented and conversational, they likely have perfusion to the brain. 04:39 Check their pulses. 04:41 For a patient to have distal pulses such as the radial pulse or DP pulses or dorsalis pedis pulses in the feet, they have to at least have enough of a pressure head. 04:50 And lastly, to assess whether or not somebody has intra-abdominal bleeding, we perform what’s called a fast examination. 04:58 Let me pose a question to you. 05:00 What is a very quick way to assess A, B, C all at once? I’ll give you a second to think about this. 05:09 It’s quite easy. 05:10 All you have to say is, “Hi sir. Can you tell me your name?” And if the patient is able to tell you their name, it suggests, number one, that their mental status is intact. 05:22 A, the airway conduit is intact. 05:24 B, air has to be moving to the conduit and pass the vocal cords for them to answer. 05:30 And C, they have enough of a perfusion to the brain to be able to answer your question. 05:37 What if there’s a clinical change during the survey, at any point during the survey? I’ll give you a few seconds to think about this. 05:48 If there’s a clinical change during your initial assessment, it’s always prudent to go back to the beginning of your ABCs. 05:54 Start with airway again. 05:56 Make sure that the patient’s conduit has now been obstructed. 05:59 Remember, sometimes if the patient has altered mental status during the clinical examination, the tongue may fall back obstructing the airway. 06:07 Next, reassess breath sounds. 06:09 Listen to their breaths to make sure the air is moving. 06:12 And lastly, re-continue on circulation assessment. 06:17 After you’ve completed an initial survey and your ABC, the last two letters are actually D and E. 06:24 D for disability and E for exposure. 06:27 D is the section which will be discussed later, it is where we assign the patient of Glasgow Coma Scale. 06:32 And E exposure is thoroughly taking a look from head to toe of the examination in completely exposed patients. 06:39 Remember, in a completely exposed patient, hypothermia can institute within minutes. 06:45 Make sure you cover the patient. 06:47 Now we can move on to a secondary survey. 06:50 A secondary survey is a fancy name for basically a head to toe examination of the patient. 06:56 We also obtain an abbreviated history. 06:58 It’s called an ample history to the most pertinent information that we need to help manage the traumatic patient. 07:05 And lastly, we like to call for a transfer center to a higher level of care for definitive trauma resuscitation. 07:13 Let me pose another question to you. 07:16 You must be wondering, “What happened to our initial patient?” Well, thankfully because of your initial assessment and management, the patient survived. 07:26 Important clinical pearls. 07:27 The patient may have an intact airway but may not be actually breathing. 07:32 Remember, the airway is just the conduit. 07:34 The breathing has the mechanics of moving air through this conduit. 07:39 In a high-yield fact, any time your clinical scenario shows clinical change or deterioration, make sure you go back to the beginning of your ABCs. 07:49 Thank you very much for joining me on this discussion of the initial assessment and management of traumatic patients.
About the Lecture
The lecture Trauma: Initial Survey and Management by Kevin Pei, MD is from the course Surgery: Trauma. It contains the following chapters:
- Initial Survey and Management
- Primary Survey: Airway
- Primary Survey: Breathing
- Primary Survey: Circulation
- Secondary Survey
Included Quiz Questions
Which of the following is the first step in the management of a trauma patient?
- Check for airway obstruction
- Cervical spine immobilization
- Assess breathing effectiveness
- Assess the mental state of the patient
- Assess the patient’s circulatory state
What is the quickest way to assess a patient's airway, breathing, and circulation in a patient who is alert?
- Ask the patient to say their name
- Assess the mental state of the patient
- Check the patient’s BP
- Assess the patient’s response to pupillary light reflexes
- Assess the patient's oxygen saturation
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
It was very concise with many important points to remember. Very well explained!
Clear, simple and short lecture. very useful for doctors/students who want to focus on important information
liked it very much , and I can not wait to learn more