Playlist
Show Playlist
Hide Playlist
Anemia in Children: Severity and Diagnosis
-
Slides Anemia Alverson.pdf
-
Download Lecture Overview
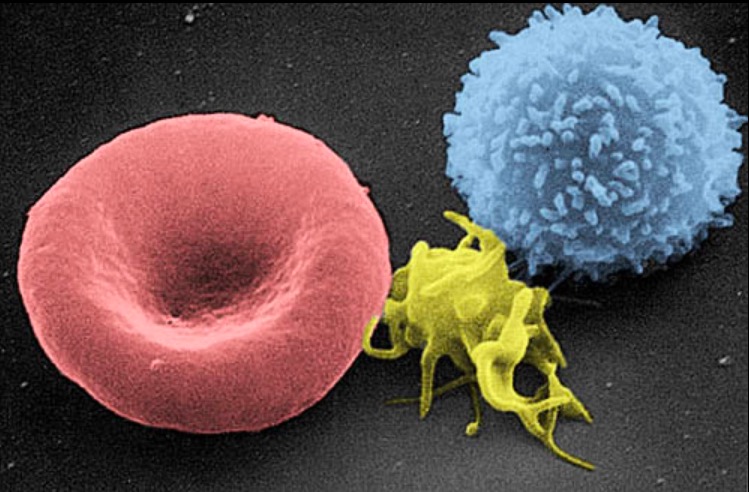
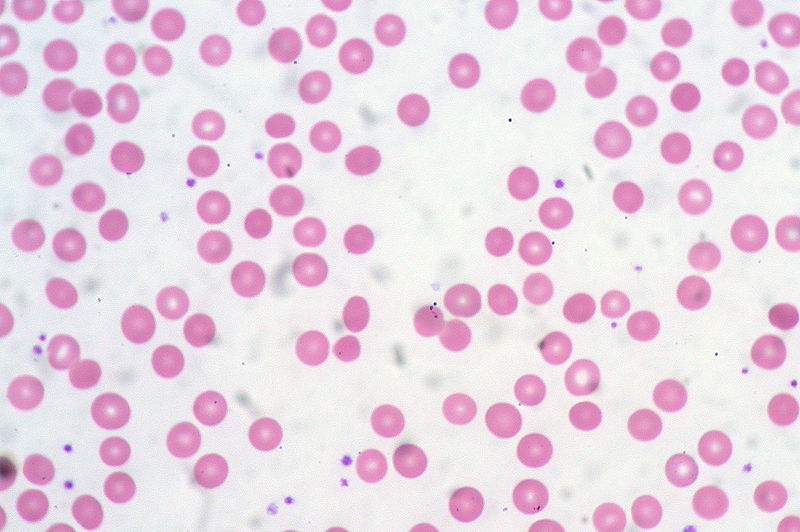
00:01 So let’s now turn page and say what do we know about the severity of anemia. 00:07 What are the symptoms and how do we judge those? Well, the signs and symptoms of anemia include decreased energy, fatigue, poor appetite, headaches, dizziness, palpitations, shortness of breath, lethargy and eventually unconsciousness. 00:23 And this is about the order in which things will present if anemia is continually worsening and not checked. 00:31 So it will start with a decreased energy and fatigue and end with unconsciousness. 00:37 Likewise, signs and symptoms can get worse with increasing severity. 00:41 So you might start with simply pallor on the skin, eventually failure to thrive. 00:45 You might see a flow murmur or hear a flow murmur. 00:48 A patient might begin getting orthostatic and then they’ll be baseline tachycardic. 00:53 They may, if their tachycardia is unchecked, develop hypotension, requiring difficulty with breathing and resulting in a need for intervention for their breathing and that can eventually lead to unresponsiveness. 01:08 So there are certain historical clues in patients with anemia that might lead you quickly to a diagnosis. 01:15 And I want to go through these key historical clues because there are things you should ask when you see a patient who you suspect has anemia. 01:23 In a patient who is 8-12 weeks of age, we expect anemia. 01:29 Why? Because this is called the physiologic nadir. 01:33 A baby is born with fetal hemoglobin. 01:36 They rapidly lose their fetal hemoglobin and have to replace it with adult hemoglobin. 01:42 Keep in mind, the half-life of the fetal hemoglobin is shorter than a half-life of adult hemoglobin and that the lifetime of a cell is about 80 days instead of 120 days. 01:53 As a result, the patient around 8-12 weeks of age starts losing that fetal hemoglobin and then the adult hemoglobin starts rising up. 02:02 And that leads a little dip point when children this age typically have low hemoglobins, around 9, 10, 11. 02:10 Patients who have pica may have iron deficiency. 02:14 Pica before the anemia may be a behavior phenomenon and maybe this child has lead poisoning from having eaten lead in the environment. 02:23 A really common one we see all the time is children who are fed too much milk. 02:28 These children will get iron deficiency by virtually being on a cow’s milk only diet because the iron is cow’s milk is less bioavailable and there is less of it. 02:39 Patients on a goat’s milk diet will have folate deficiency. 02:43 Patients with weight loss, maybe they don’t have a nutritional deficiency, although they might. 02:48 May be they have a systemic illness that is driving that weight loss. 02:52 For instance, a patient with Crohn’s disease may have antecedent weight loss for a few months beforehand and present with a normocytic anemia because of general dysplastic or rather suppression of the bone marrow that’s happening inside the bone marrow from just being inflamed. 03:09 Additionally, of course, we’re going to ask about lead environment in any patient when we’re worried about anemia because of the prevalence of lead poisoning in the United States. 03:19 So when we see a patient with anemia, we think in these boxes of increased destruction and decreased production and active bleeding, but when we get the labs back, we don’t get that information. 03:31 What we get back from the lab is the MCV and the RDW. 03:36 In any patient with an anemia, you must check both the MCV and the RDW because these are going to help you categorized the anemia and they are very valuable cues as to what’s causing the problem. 03:49 I’m going to go through this carefully. 03:52 In microcytic anemia, which is an MCV of less than 70, the leading causes are iron deficiency and lead poisoning. 04:02 These 2 things you must know. 04:04 They’ll definitely be on the test. 04:06 In a patient with a normocytic anemia, this could be acute blood loss or this could be anemia of chronic disease. 04:15 Patients who have general inflammation who aren’t making red blood cells very often, but the red blood cells they can make are generally normal. 04:24 Likewise, in patients with large red blood cells with an MCV over 85, they are more likely to have a B12 or folate deficiency. 04:34 Those are incredibly important and highly likely to be on your test. 04:39 Okay. 04:41 So let’s understand the RDW because I think it can be confusing to some people. 04:47 Here are two individuals. 04:49 This is a histogram of the size of their red blood cells. 04:52 You can see that on average, the green person has a slightly lower MCV, but there is a narrow distribution of the sizes of those red blood cells. 05:04 On the contrary, the person with the red line has a higher hemoglobin, but there is a larger population of both small and large cells. 05:14 So the hemoglobin is right here. 05:17 This is the MCV. 05:19 This is the average size of those red blood cells and you can see the person with the graph in red has a slightly larger size of their red blood cells than the person with a graph in the green, but there is a lot of overlap. 05:31 To assess how wide those curves are, we use the RDW. 05:36 So the person in the red has very high RDW and the person in the green has very narrow RDW. 05:44 This is a very unique situation. 05:47 This is a patient who has both iron deficiency which makes small red blood cells and folate deficiency which makes big red blood cells. 05:56 If you saw this patient, you would say their MCV is normal. 06:01 It’s right down the middle, but clearly this is not a distribution and so you would see a really huge RDW. 06:08 That would be your clue that something is going wrong. 06:13 What about the reticulocyte count? So the reticulocytes are baby red blood cells. 06:19 They are just few steps before the erythrocyte. 06:22 So a low reticulocyte count implies that the cells aren’t being made. 06:29 An example would be very recent and rapid destruction or blood loss. 06:33 If I acutely bleed out, it will obviously take a week or so before I’m starting to be able to make reticulocytes. 06:40 It could also mean, however, a decreased production. 06:44 If there are fewer cells coming down the pike, there will be fewer reticulocytes. 06:49 A high reticulocyte count implies that the bone marrow is doing its best to replace your loss. 06:56 So if I have a chronic indolent autoimmune hemolytic anemia where I’m constantly breaking down my red blood cells in a pretty reasonable rate, I may have a high reticulocyte count because I am trying very hard to overcome that loss or for example, a slow progressive loss like a chronic GI bleed.
About the Lecture
The lecture Anemia in Children: Severity and Diagnosis by Brian Alverson, MD is from the course Pediatric Hematology. It contains the following chapters:
- Severity of Anemia
- Anemia – Diagnosis
Included Quiz Questions
A goat milk only diet results in which of the following dietary deficiencies?
- Folate deficiency
- Iron deficiency
- Lead poisoning
- Vitamin B12 deficiency
- Vitamin C deficiency
Which of the following is not a sign or symptom of anemia?
- Bradycardia
- Poor appetite
- Lethargy
- Unconsciousness
- Flow murmur
A 5-year-old child has anemia and a history of eating raw rice. Which type of anemia does the child have?
- Iron deficiency
- Folate deficiency
- Lead poisoning
- Thalassemia
- Hemophilia
A child’s blood profile shows macrocytic RBCs (MCV of 98). Which of the following types of anemia does the child have?
- Folate deficiency anemia
- Systemic lupus erythematosus
- Iron deficiency
- Lead poisoning
- Thalassemia
Which of the following conditions cause a low reticulocyte count?
- Aplastic anemia
- Autoimmune hemolytic anemia
- Chronic GI bleed
- Thalassemia
- Sickle cell anemia
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |