Playlist
Show Playlist
Hide Playlist
Acute Pancreatitis: Ranson's Criteria, Treatment, and Complications
-
Slides Pancreas and Biliary Tract.pdf
-
Download Lecture Overview
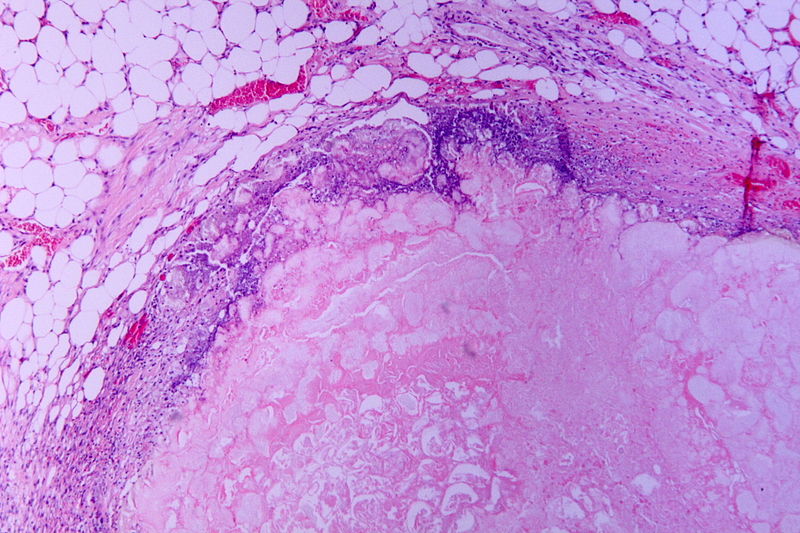
00:01 We have something called Ranson's criteria for acute pancreatitis. 00:04 I've given you a bunch of criteria in medicine, especially with the GI system, but what's most important about the criteria is that you understand the concepts and at least know the name and what type of disease and what organ system that you're in, and that will help you out tremendously. 00:23 For example, if you talk about MELD and that will be the model for end-stage liver disease. 00:28 If you're thinking about Gleason, the prostate system. 00:31 You're thinking Ann Arbor classification, Hodgkin. Remember all these, right? Now, some of these you have to know a little bit more detail than others, but nonetheless, know what organ system. The other one that comes to mind is Jones criteria for rheumatic fever. 00:48 On admission, older patient, acute pancreatitis, -itis means inflammation. 00:57 It should be of no surprise that you found leukocytosis. 01:02 -itis of whom? The pancreas. There's every possibility that the insulin might be affected. Then what happens to glucose? Hyperglycemia. Don't just memorize it, analyze everything that I'm saying here. 01:17 Because you have the understanding now, okay? That's the power that you have now. 01:21 It's the fact that you have all these information in your head and everything that's being presented here, you're actually understanding what's going on. 01:29 It's beautiful, it really is. 01:31 You have lactate dehydrogenase and AST that might be elevated, meaning to say that now, you start involving your liver and company, especially AST. 01:38 On admission, within two days, 48 hours, now at this point hematocrit drops greater than 10% and now, you're thinking about anemia kicking in, kidneys might be affected with BUN rising. Calcium is going to diminish. 01:54 Diminish. The more this calcium starts dropping or it starts depositing on your damaged tissue, what kind of calcification is this? Good. Dystrophic calcification. 02:05 Also with these enzymes causing damage to the lung, two days later, you find that your PO2 - What's your normal PO2 in the artery? Approximately 100, right? About 95 to 100. It dropped down to 60. 02:20 This is not good. You have damage to the lung and base deficit, and you have fluid deficit of greater than 6 liters, that's important, something they call third spacing. 02:32 Fluid deficit of greater than 6 liters. You've heard of third spacing? Give me some examples oft hird spacing. How about third degree burns? Severe burns in which now the fluid is escaping into your tissue. 02:47 Pancreatitis, there's every possibility that third spacing might be a possibility. 02:51 So your patient is actually hypovolemic and is therefore presenting with hypotension. 02:58 So therefore, why are we looking at this? Greater than three risk factors, mortality rate 15%. You double this and you have six of these risk factors, mortality rate-- it doesn't get any worse than this -- 100%. 03:18 Acute pancreatitis. What is your management? Supportive care. Step by step. 03:24 Bowel rest. IV fluid, your patient is hypovolemic. Your patient's in pain, so much so that your patient might actually become addicted on narcotics. 03:38 When's the last time you've heard of that? Let's see this patient. 03:42 Young African American boy, playing quite a bit, and complains of pain in the chest, pain in the hands, sickle cell disease, dactylitis. Pain, pain, pain, pain. 04:00 Analgesia there as well. 04:02 Antiobiotics are reserved for cases of necrotizing pancreatitis but are only given if there is a suspicion for an infection. 04:10 Continue here with the pancreas, it's the organ for proper digestion. 04:17 My goodness. Every food group that we consume, pancreas plays a role. 04:23 Trypsin and company, protein. Lipase, lipid. Insulin, glucagon, all that's carbohydrates granted some as endocrine and some as exocrine, but it plays a huge role. So therefore acute pancreatitis, you're definitely worried about proper nutrition. Parenteral nutrition. ERCP for duct disruption, meaning to say there might be a need to remove a stone, but be careful with that, you might cause damage. 04:52 And if there is going to be abscesses and pseudocysts that we'll talk about in a little bit, then drainage of infected pancreatic collection is definitely something that you want to think of in doing. 05:05 At some point, perhaps surgery is required and you start thinking about necrosectomy. In other words, you need to get in there and make sure that you prevent any further damage and surgery might be the last resort. 05:19 Complications of acute pancreatitis locally? Something called phlegmon. 05:22 Illl-defined fluid collection, usually sterile locally, acute pancreatitis. 05:28 So think about where you are in the pancreas and pancreatic region and all the different things that could occur locally as complications. 05:36 The pseudocyst we talked about. I mean this is pseudocyst, meaning to say that it's not a true cyst. And the reason for that is because it's a non-epithelial wall. By definition, a cyst has a pure or true epithelial wall. That's not whatever is a pseudocyst. If infection sets in, your worried about pancreatic abscess and you might have pseudoaneurysm of splenic artery. 06:04 This is known as hemosuccus pancreaticus and meaning to say that you have hemorrhage taking place into it. These are local complications that you want to keep in mind for acute pancreatitis. 06:15 Systemically, we've talked about a few of these already. 06:18 If these enzymes and such then start getting into the respiratory system or pulmonary circulation, there's every possibility that ARDS might kick in. 06:28 Next, kidney damage, renal failure and with such severe volume deficit may actually result in shock and you're absolutely worried about DIC. 06:40 Remember, keep this in mind from henceforth, I can only give you so many different angles for DIC, okay? And by that I mean DIC is an interesting beast. It really is. 06:54 For example, we've talked about M3, acute myelogenous leukemia type 3, that being DIC, amniotic fluid emboli, venom, sepsis being a common. What I'm saying is anything in which to the body, there has been pretty massive alterations or even during pregnancy. Remember with pregnancy, especially if we start getting into the point of what's known as pre-eclampsia or eclampsia and such, you might be worried about DIC as well. 07:20 What you're paying attention to truly is what is that major stress the patient might be then suffering or experiencing that all of a sudden triggers DIC and it's dangerous.
About the Lecture
The lecture Acute Pancreatitis: Ranson's Criteria, Treatment, and Complications by Carlo Raj, MD is from the course Pancreatic and Biliary Tract Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following criteria is associated with acute pancreatitis?
- Ranson's criteria
- Jones criteria
- Dukes criteria
- Light's criteria
- Stanford criteria
Which of the following is NOT a part of Ranson's criteria for admission?
- Calcium < 8 g/day
- Age > 55 years
- LDH > 350 IU/L
- AST > 250 IU/L
- Glucose > 200 IU/L
When should Ranson's criteria for acute pancreatitis be assessed?
- After 2 days
- After 3 days
- After 1 day
- After 4 days
- After 7 days
Which of the following is NOT a treatment option for acute pancreatitis?
- Steroids
- Being NPO
- IV fluids
- Bowel rest
- Analgesics
Which of the following is NOT a complication of acute pancreatitis?
- Calcification
- Phlegmon
- Pseudocyst
- Abscess
- Hemorrhage
Which of the following is the cause of hemosuccus pancreaticus?
- Pseudoaneurysm of the splenic artery
- Aneurysm of the splenic vein
- Aneurysm of the splenic artery
- Pseudoaneurysm of the splenic vein
- Aneurysm of the hepatic artery
Which of the following is NOT a systemic complication of acute pancreatitis?
- Phlegmon
- Pleural effusion
- Kidney failure
- DIC
- Shock
Customer reviews
4,3 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
2 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Best explanation,Dr.Raj makes any difficult topic very easy. thank you very much Sir
Great lecture and Dr. Raj is wonderful. My only comment would be to add a bit of information about the pathogenesis tied to the different etiologies
his lecture is short & more useful good for practice study easily