Playlist
Show Playlist
Hide Playlist
Acute Hypercapnic
-
Slides RespiratoryFailure RespiratoryPathology.pdf
-
Download Lecture Overview
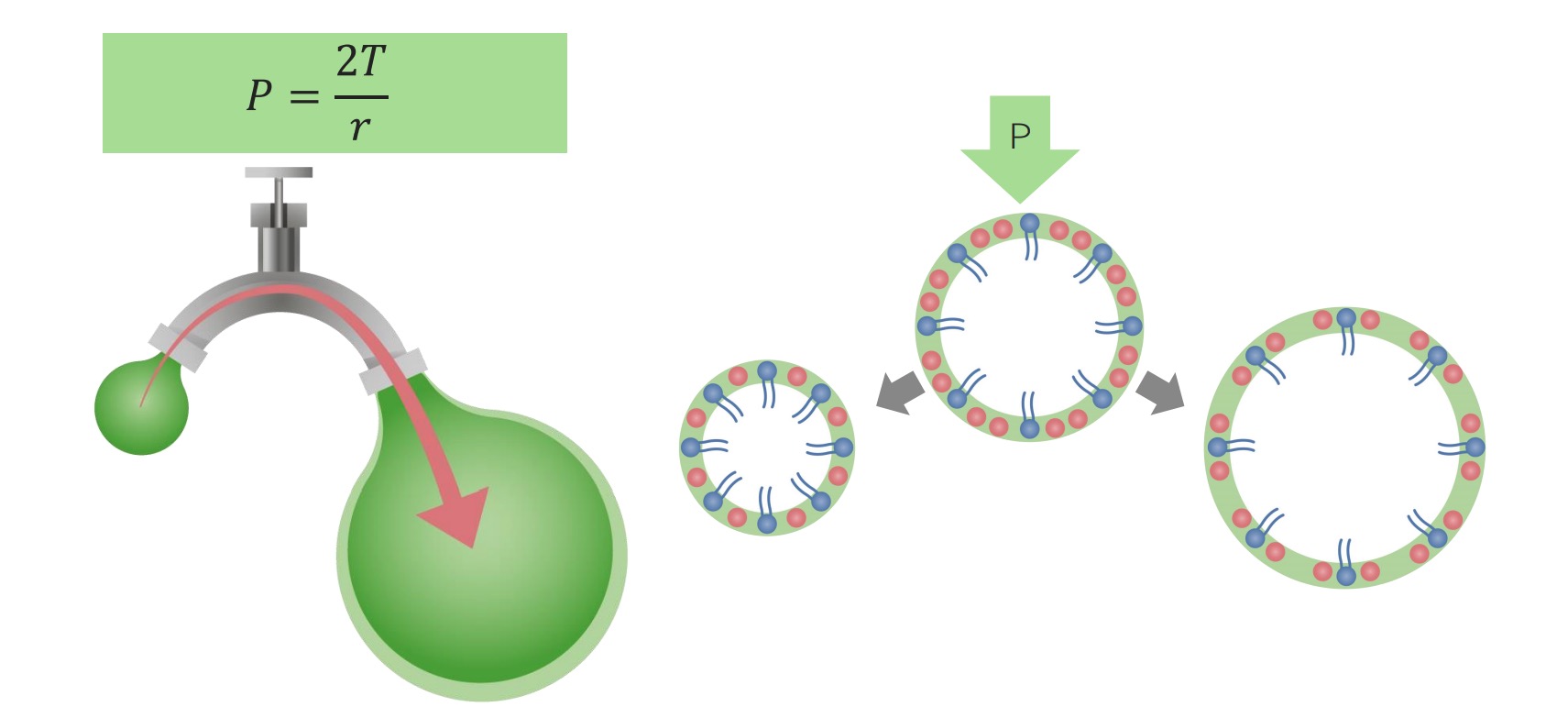
00:00 Continue forward. We have differentials now, for acute type of hypercapnea. Ventilatory. 00:07 So this would mean that something is causing your absolute shutdown of the respiratory drive to blow off carbon dioxide. What is this? Maybe a demyelinating disorder. So from the CNS maybe stroke, maybe herniation, multiple sclerosis type of issue or perhaps even drugs. 00:25 So this is then, for example, think about opioids that we talked about, knocking out the respiratory centre. What happens? From the CNS you can’t properly do what? Blow off your carbon dioxide. Herniation. Think of something like your subfalcine type of herniation, or something like a uncal herniation, right? Some of those herniations in the brain may then bring about, well, damage to the respiratory centre. What’s my topic? Acute hypercapnea, failure to blow off carbon dioxide. 00:57 Continuing further with demyelinating disorders. Guillain-Barre, right, we’ve talked about, where diaphragm can’t properly work. Myasthenia gravis is a big one. So, therefore, here you’re looking at possibly, a female, autoimmune disease, and she wakes up in the morning and she feels great, right? And then she tells you “Hey, doc, in the middle of the day I’m having a hard time looking at my computer and stuff. And as the day progresses and I get into 3 or 4 o’clock in the afternoon, oh, I can’t even move. And then I go to sleep at night, I can barely even crawl into my bed. I have to drag.” Not that bad, but I’m just being dramatic here. Wake up in the morning and that cycle continues. 01:37 This is myasthenia gravis. Botulism, what’s going on here? It’s the fact that, well, those patients that you might get, right, and of course, cosmetic surgery is a big deal. And you do what you want, but those patients that are coming in and they want to get rid of their wrinkles. What do you do? You are injecting, what’s that called? Botox, right? And so, therefore, now, how are they walking around? Oh, my face is groggy. 02:03 So, I mean to say that they have that type of face in which their wrinkles are gone, but at what expense? But, anyhow, I’m just having fun there. It’s the fact that you’re inhibiting the release of acetylcholine from the neuromuscular junction. There you go. 02:18 Neuromuscular diseases. 02:19 Myopathies, these include things like muscular dystrophy. 02:22 Airways. You can have even issues like bronchoconstriction, such as from asthma, in which it may result in difficulty with blowing off carbon dioxide, obstructive patterns. 02:33 Often seen in acute respiratory failure as patient tires. That’s a big one. So, for example, say that you have a child who just had a asthma attack, and at this point comes in and huffs and puffs, breathing really fast. 02:49 My goodness gracious, intercostal muscle. All the accessory muscles of respiration are going at full steam. This is a child. And then, what happens? Well, patient comes to you and intern perhaps gives treatment, whatever that may be, some type of bronchodilator, and the child starts quieting down. Intern feels as though that he or she has just saved the life of the child. Well, come back with the [Inaudible 00:12:21] the child is dead. What just happened? This is what happened. Often seen in acute respiratory failure as patient tires. So, the reason that the child was tiring, was why? Because the actual muscles got tired and then what happened? Oh, my goodness, there is no energy left to blow off that carbon dioxide. Isn’t that my topic? Yes, it is. That is no joke. 03:46 You're better off breaking off a few teeth with intubation than knowing that you might have killed the patient, a child on your clock. Could I be any more dramatic? Hypercapneic respiratory failure ultimately leads to hypoxemia. Why? As we said earlier, carbon dioxide, wherever it may be, is going to then displace the oxygen, especially in the alveoli. Not a good thing. 04:10 Now, there is something from physiology that I wish to bring in to play with dealing with hypercapnea, okay? There is a difference between rapid shallow breathing, which students tend to confuse with rapid deep breathing. And students never seem to get this straight. 04:27 Well, let’s organise our patterns and get it straight, once and for all. Now, I’m not going to go through every single one, but I’m going to set up the table, where you understand as to how you are breathing from patient to patient to patient. 04:39 Let’s begin. So, on the ventilation side are your different patients. The Vt is your tidal volume of different types. The f is frequency, the number of breaths or respiratory rate that you have. Then, you stop here. Then you have two different types of ventilation. 04:58 We have total ventilation and we have alveolar ventilation. You keep them separate, please. 05:06 Why? Total ventilation is not taking your dead space into consideration. Is that clear? Is that space always pathology? Not at all. Remember, when you’re breathing in, and is it possible some of this air then may get trapped? Sure. Anatomically. 05:23 And how much is this dead space that we're referring to? This dead space, you should know from physio, is 150. So, you noticed, let’s do the following. 05:32 First, total ventilation for patient A, normal patient, normal. 500 times 10 gives you a total of 5000. Wow, that seems fantastic. Now, actual alveolar ventilation. Take a look at the equation, please. It’s VA, in other words alveolar ventilation equals tidal volume in our patient A, 500. VD stands for dead space, which for you clinically is fixed at 150. So, 500 minus 150, 350 times, what’s your frequency of this patient? 10. What does that give you? 3,500. That’s normal. Are we clear? Now, on your own time, you can take a look at patient B. That’s great. Patient C. Okay. 06:18 Now, I want you to pay attention to patient D and E for me. Patient D and E are both pathologies in which is compensation taking place and you’ll see as to who is who. Here, tidal volume for patient D as in delta is 300. Frequency is 18. What’s normal? About 12-16 breaths per minute. We are at 18, understand that this is now increased respiratory rate. So, increased frequency. So, now, it’s rapid breathing, that much we do know. Take a look at total ventilation. 5400. What was normal? 5,000. 18 times 300 gives you 5400. 06:58 Okay. But, take a look at alveolar ventilation here. You take the 300 and from this you subtract what? 150. Wow, that’s really low. Multiply that by 18, you get a measly 2,700. 07:13 What’s normal alveolar ventilation? 3,500. We have dropped by 800 in patient D. Who is this patient? Maybe rapid shallow breathing, secondary to a DVT, a PE. So, there’s every possibility in PE that you might have rapid shallow breathing. But guess what, you might not necessarily have hypercapnea. Okay? Be careful. So, now, or should I say you would necessarily have hypocapnea. So even though you are rapid shallow breathing, you might still be retaining to carbon dioxide, because that alveolar ventilation isn’t great. 07:52 That patient D, that’s a relevant patient for our topic, but, just to make sure we’re clear, let’s take a look at rapid deep breathing. Patient E, once again, look at frequency. 08:04 15, elevated. Tidal volume, 600. That’s deep tidal volume. Now, you take a look at the alveolar ventilation here, please. So, 600 minus 150, multiple that by your 15. You get a whopping 6,750. Is this effective for blowing off carbon dioxide? Of course it is. 08:23 Welcome to DKA, diabetic ketoacidosis, metabolic acidosis. How are you compensating? Rapid deep breathing and every breath that you then smell, oh, it smells so good. That’s your sweet odour, right? Welcome to Kussmaul’s breathing. Clear? You pay attention to patient D and patient E. However, make sure you begin with patient A and little titbit that you wanna know from physiology, very relevant for our cases. 08:49 Let’s go on to now, chronic. With chronic type of respiratory failure, due to chronic hypoventilation. So, what’s your A-a gradient here? Good. Normal. It’s depressed in the alveoli, therefore, depressed in your artery. 09:06 Next, well, if there’s chronic respiratory acidosis, you can be absolutely sure that your patient has increase in carbon dioxide. These tend to be type II respiratory failures. 09:21 Type I respiratory failure, not necessarily have an increased in carbon dioxide, but definitely have a depressed oxygen. In chronic respiratory failure, your carbon dioxide will be elevated, in fact, your body then becomes accustomed. It’s amazing, isn’t it? Remember, the central chemoreceptors are very very sensitive, to whom? Carbon dioxide. But, amazingly in a chronic setting, they then become dull. So, therefore, the central chemoreceptors are not going to respond. So, therefore, now, understand that your body becomes more responsive to depressed oxygen over long period of time. But, yet, the carbon dioxide levels are elevated. 10:03 So, therefore, what’s the kidney doing? Holding onto the bicarb. Please, look for serum bicarb to be elevated in chronic respiratory acidosis. Do not memorise any of this. You put stories, give yourself clinical situations and you build upon the information that we have looked at over and over and over again. I hope point two or that second bullet point makes perfect sense to you. 10:28 Now, diseases that can affect. Well, ventilatory control. CNS insult. But, we also saw they were acute? Sure. But, could you have chronic changes? Absolutely. Obesity-hypoventilation syndrome is a big problem in the United States. Obesity, what happens? Oh, boy. Well, obesity, understand that the patient is not able to properly ventilate. What is he or she retaining? Carbon dioxide. So, therefore, your patient is in a chronic state of hypercapnea. 10:58 Not good. Let’s continue. 11:01 We have chest wall type of issues. This is kyphoscoliosis where literally the lung doesn’t wish to expand. This is chronic. Neuromuscular diseases, here could also be chronic. Airways can be chronic and chronic diffuse lung disease. We’ll talk more about that lung disease later on, but all these may result in chronic type of, what’s on this? Hypoxemia. 11:22 And, hence, elevations of your carbon dioxide.
About the Lecture
The lecture Acute Hypercapnic by Carlo Raj, MD is from the course Respiratory Failures.
Included Quiz Questions
Which of the following CNS lesions can cause hypercapnia?
- All answers are true
- Drugs decreasing respiratory drive
- Herniation of the brain
- Stroke
- Multiple sclerosis
Which of the following is NOT an example of a neuromyopathic disorder that causes acute hypercapnia?
- Malignant acanthosis nigricans
- Myasthenia gravis
- Muscular dystrophy
- Polymyositis
- Botulism
Which of the following is NOT a cause for chronic respiratory failure due to chronic hypoventilation?
- Hyaline membrane disease
- Obesity hypoventilation syndrome
- Kyphoscoliosis
- Amyotrophic lateral sclerosis
A patient is on treatment for chronic obstructive pulmonary disease for many years. His HCO3 levels are elevated in the urine. Which of the following better explains the underlying pathophysiology?
- Chronic hypoventilation causes the chemoreceptors to become unresponsive over many years, leading to the consumption of carbon dioxide for the formation of HCO3.
- Chronic hypoventilation causes the chemoreceptors to become stimulated over many years, leading to the consumption of carbon dioxide for the formation of HCO3.
- Chronic hypoventilation causes baroreceptors to become unresponsive over long periods leading to the consumption of carbon dioxide for the formation of HCO3.
- Chronic hypoventilation causes baroreceptors to become stimulated over long periods leading to the consumption of carbon dioxide for the formation of HCO3.
- Chronic hypoventilation causes no change in the carbon dioxide levels but the secretion of HCO3 occurs.
The pathophysiology of myasthenia gravis predisposes to death via which respiratory mechanism?
- Hypercapnic respiratory failure
- Hypoxemic respiratory failure
- Loss of hypoxic drive
- Respiratory center depression
- Inability of the muscle to relax
A patient has a normal tidal volume and an increased respiratory rate. What is the expected alveolar ventilation?
- Increased
- Decreased
- Remains the same
- Initially increased and then decreased
- Initially decreased and then increased
Which of the following can cause an increased dead space?
- Emphysema
- Asthma
- Sarcoidosis
- Interstitial lung disease
- Lung cancer
A 60-year-old patient has a decreased tidal volume and an increased respiratory rate. The total alveolar ventilation is decreased. The V/Q is 0. Which of the following is the most likely cause?
- Asthma
- Emphysema
- Hypoxia
- Lung cancer
- Tuberculosis
If the formula to find alveolar ventilation is (tidal volume - dead space) × frequency of respiration, which of the following values remains constant?
- Dead space
- Tidal volume
- Frequency of respiration
- Alveolar ventilation
- Tidal volume - dead space
Which of the following is the correct formula to assess the alveolar ventilation?
- Alveolar ventilation= ( tidal volume - dead space) × frequency of respiration
- Alveolar ventilation= (tidal volume + dead space) × frequency of respiration
- Alveolar ventilation= (dead space - tidal volume) × frequency of respiration
- Alveolar ventilation= (frequency of respiration- dead space) × tidal volume
- Alveolar ventilation=( tidal volume -frequency of respiration) × dead space
If a patient has alveolar ventilation of more than 7200 ml/min with a respiratory rate of 21/min along with a tidal volume of 600ml/min. What kind of breathing does one expect?
- Rapid deep breathing
- Rapid shallow breathing
- Slow shallow breathing
- Slow deep breathing
- Normal breathing
A patient has alveolar ventilation of 9000 ml/min, a respiratory rate of 20/min, and a tidal volume of 600ml/min. This is likely a respiratory compensation for which of the following?
- Metabolic acidosis
- Respiratory acidosis
- Metabolic alkalosis
- Initially, respiratory acidosis further converting to respiratory alkalosis
- Respiratory alkalosis
A patient has alveolar ventilation of 3000 mL/min with a respiratory rate of 20 and a tidal volume of 300 mL. What kind of breathing is expected to occur?
- Rapid shallow breathing
- Rapid deep breathing
- Slow shallow breathing
- Slow deep breathing
- Normal breathing
A patient has alveolar ventilation of 3000 ml/min with a respiratory rate of 20 and a tidal volume of 300ml/ min. What will happen to the patient's carbon dioxide level?
- Increase as there is less alveolar ventilation for exchange.
- Decrease as there is less alveolar ventilation for exchange.
- Remains unchanged
- Increase initially and eventually decreases
- Decreases initially and eventually increases
How is bicarbonate concentration affected in patients with chronic hypoventilation?
- Increases
- Decreases
- Remains the same
- Nullifies
- Changes proportional to the change in SaO2
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |