Playlist
Show Playlist
Hide Playlist
Infections of the Upper Pediatric Airway: Croup
-
Slides Headandneckinfections Pediatrics.pdf
-
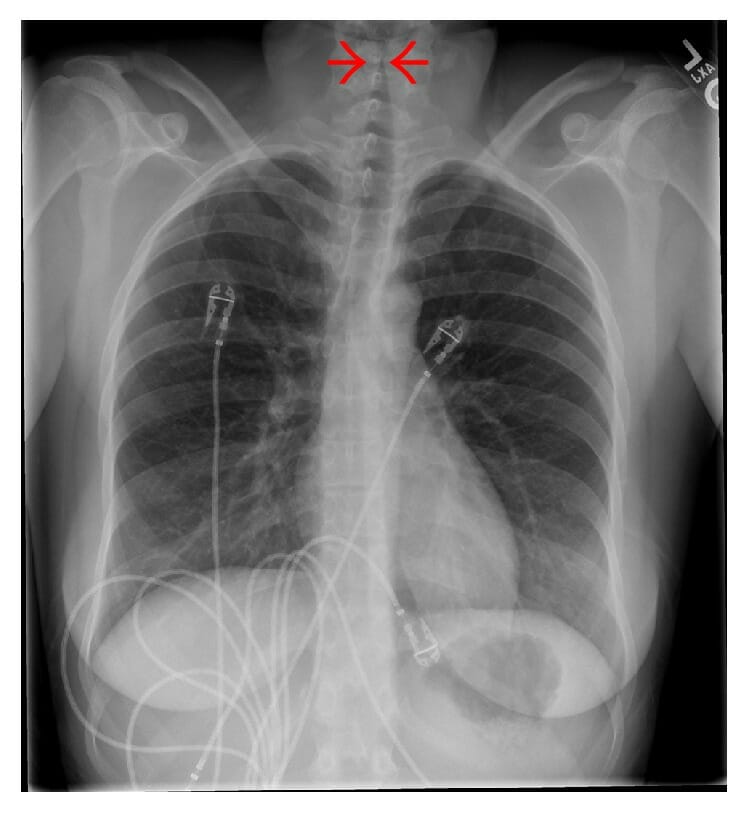
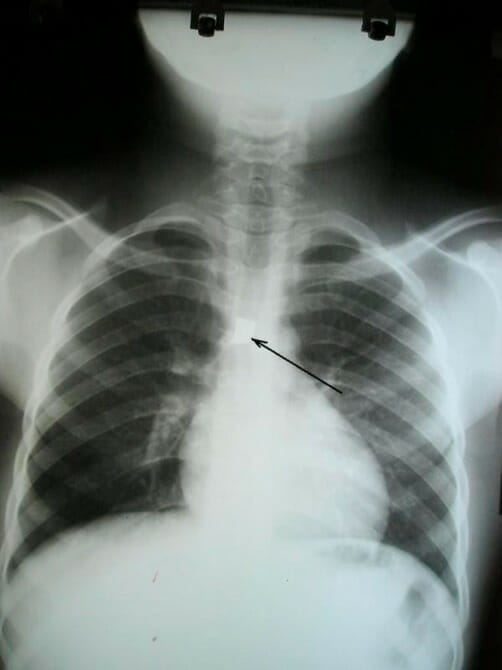
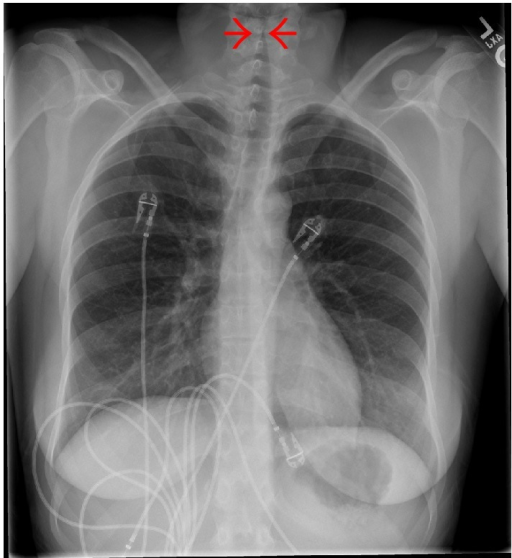
Download Lecture Overview
00:00 Let's switch now to perhaps slightly deeper infection which is Croup. This is a viral infection of the larynx. It happens in kids. In adults, this is laryngitis. In kids, this is croup. It typically affects kids between 3 months and 3 years of age and usually they have upper respiratory infections, runny nose, congestion, cough. So, classically we're taught that this is caused by parainfluenza virus. That's the answer on your test. But realistically this can be any virus at all. It can be paraflu, it can be flu, it can be RSV, it can be adeno, it might be enterovirus, rarely human metapneumovirus, usually that's bronchiolitis but it could be and it certainly could even be coronavirus. It doesn't really matter what the virus is. What's more important is that they're sick and they need our help. So, typically these patients will present with fever with a barking cough, people describe it as a seal if you ever heard a seal bark, that's sort of what it sounds like. They almost always will have a hoarse voice. This is the kind of question that's a good clinical pearl. You should ask that mom "Does your child sound like they're crying as like it normally is or does it sound hoarse?" and frequently they'll _____ "Oh yeah it sounds much different and that's a clue it's probably croup. They may have difficulty swallowing, they may have drooling because they don't want to swallow their saliva and they may complain of throat pain if they're old enough to tell you about that. So there is this score called the Westley croup score which is out there and sometimes it shows up on tests. Realistically, we almost never used this score so I'm not going to go through the details of the score, it's there if you want to look at it. What's key is that these patients present with stridor and stridor is the thing that worries us most. Oftentimes they'll present with stridor waking up at night. 02:06 Classically parents say "had a cold, put him to bed and then in the middle of the night he started crying and when I went he was making this horrible noise while he was breathing in." Remember, stridor is from a narrowing of the upper airway. In patients who have stridor at rest, we're really worried about these children and we generally would like to have them in the inpatient setting. In patients who have stridor only with severe agitation like crying, that might be okay as long as their airway is otherwise fine. So we worry about kids with stridor at rest. When we see a patient with croup, we want to make sure it's not another thing. For instance, "How do I know this child doesn't have a cold and recently just got a foreign body lodged in the throat?" There can be some clues about foreign body that are important. Examples would be "Mom says the child was completely fine and then all of a sudden there was remarkable stridor." That would be unusual. Very rarely this could be a mass or an airway hemangioma. It's interesting, children with airway hemangiomas often show up with croup because they're more susceptible to it because there's less space in that airway in the first place. In a child with recurrent croup infections, you might worry about some airway mass or problem. Patients may have epiglottitis although as we already discussed in the epiglottitis section of this talk that's fairly rare now. This might be an allergic reaction. We want to listen for wheezing too and look for areas of edema like on the lips or the tongue. If you're concerned about this being something else, the test of choice is an anterior x-ray. What you'll see on anterior x-ray is called the Steeple sign. This is commonly on test. The ID is from the front, that airway which you can see on this x-ray, looks a little bit like a church steeple. Here's the church fitting right in there with the steeple pointing up. 04:04 That's your sign that that what's the problem is. So let's talk about the management of croup. 04:09 First off, we have classically taught people that if it's at home and it's relatively mild, humidity or cold air might work. We tell the families you can go in the bathroom and steam it up and put the child in there or you can take the child outside where it's cold because this usually happens in the winter and the cold will help shrink the swelling in their throats. Maybe this works, probably it doesn't. There was 1 study from Canada where they showed the humidity was not beneficial. So why do this seem to work? Well they seem to work, remember a child that's crying has a long exhilational phase and a very quick inhalation. So what happens is as that child is breathing in quickly, the stridor is worse. Once they stop crying, the stridor gets better. So if you can imagine, child wakes up in the middle of the night, starts crying, parents hear the weird stridors, noises, run in, take the child, bring the child to the bathroom, wait for the bathroom to steam up. By now the child has stopped crying. The humidity maybe that helped the crying, that's a stridor but maybe it was just that the crying stopped. In the emergent setting though, we have a few things we can do. The first is we will give a dose of dexamethasone. Some people like to use prednisone but most of us preferred dexamethasone. Why do we care? Because dexamethasone has a much longer half life, tends to last about 3 days. So you can give 1 dose of dexamethasone rather than 3 doses of prednisone and a prescription that the mom has to take home and try and wrestle to get their child to take what is the somewhat nasty tasting drug once or twice a day. Dexamethasone, you give it once you're done, you can give it through orally or you can give it through an injection. Also, because the dexamethasone takes a few hours to kick in, in an emergent setting we can give racemic epinephrine. We give that nebulized. The child is to breathe in this treatment. That racemic epinephrine causes alpha constriction and a constriction of the blood vessels that are providing the edema in the throat. In other words, it acutely reduces the edema. One thing you have to watch for though is that the racemic epinephrine is relatively short acting. It wears off within an hour or 2. So you have to watch that child to make sure they don't get worse again. It would be crime to give a child racemic epinephrine and then say "Yup, okay you're good to go" and then have them be at home when the child gets worse again. So what we'll typically do is give a dose of racemic epi and give a dose of dexamethasone and watch for a period of time. If the child needs another treatment, often they're admitted to the hospital but what usually happens is the dexamethasone has kicked in by the time the racemic epinephrine has worn off and the child should be good to go. Some people like to give another dose of dex the next day. There's no evidence to say that's a good or a bad thing to do. Generally, we will discharge those patients who are admitted once they're without stridor for a 3 to 4-hour period. So, once they're no longer requiring epi to keep going they should be okay to go home. What's key is we never send these children home who have worked up breathing or who have stridor at rest. So that's my summary of the major common infections of the upper airway. Thanks for your time.
About the Lecture
The lecture Infections of the Upper Pediatric Airway: Croup by Brian Alverson, MD is from the course Pediatric Infectious Diseases. It contains the following chapters:
- Pathology and Diagnosis of Croup
- Management of Croup
Included Quiz Questions
What should be given as soon as possible after a diagnosis of severe croup has been made?
- Dexamethasone + nebulized racemic epinephrine
- Dexamethasone
- Nebulized racemic epinephrine
- Humidified air
- Nebulized albuterol
Which of the following organisms is classically implicated in the infant with croup?
- Parainfluenza
- Haemophilus influenzae
- Influenza
- Corona virus
- Enterovirus
What is the most common age group of patients who present with croup?
- 3 months to 3 years
- 1 month to 3 months
- 6 months to 6 years
- 5 months to 5 years
- 4 months to 4 years
Which of the following is NOT a typical symptom of croup?
- Hiccups
- Barking cough
- Hoarseness of voice
- Dysphagia
- Drooling
Which of the following is the typical radiological finding for croup?
- Steeple sign
- Thumbprint sign
- Rat tail sign
- Bird beak sign
- Corkscrew sign
Which of the following is the test of choice for diagnosing croup?
- Anterior neck X-ray
- Lateral neck X-ray
- Base of skull X-ray
- Ultrasound of the neck
- Laryngoscopy
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture. I particularly liked the emphasis on the differential diagnostic, the remarks regarding the humidity and cold and the modality of the treatment. Also the signs that the child is sufficiently treated.
I really liked this summary, the information is precise and really easy to get thanks to the way the doctor explains it. Today at school we reviewed this topic, so when I got home I went over CRUP again with this video and it was really, really useful.