Playlist
Show Playlist
Hide Playlist
Bronchi and Bronchiole
-
Slides 03 Human Organ Systems Meyer.pdf
-
Download Lecture Overview
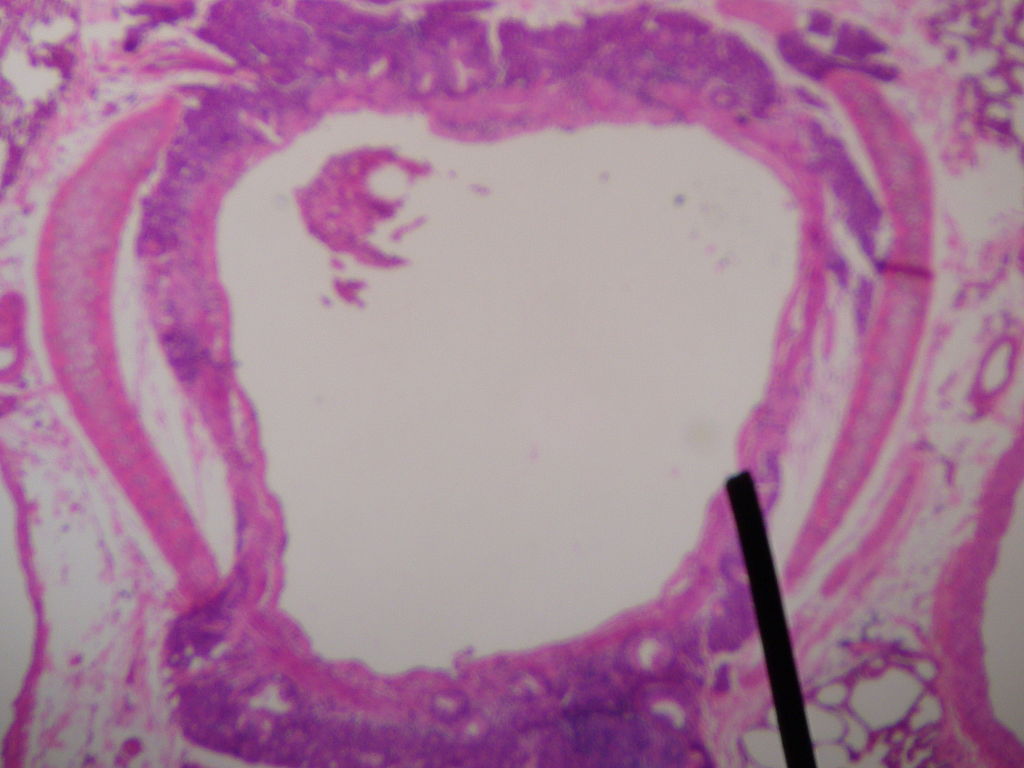
00:01 propria and the underlying submucosa. When you go down from the trachea towards the lung, the trachea is going to branch prior to going to the left and right lung inter bronchi and those bronchi divide further into a number of bronchopulmonary segments. They go to different lobes of the lung. And then within those bronchopulmonary segments, there are further divisions and these divisions are defined anatomically. And those of you do the anatomy of the lung will know these divisions. Here I just want you to appreciate that as we move down from the trachea into the lungs, these bronchi are still supported by cartilage. And they pass down to the deep levels of the lung getting smaller and smaller, but they are still highly supported by the cartilage. The cartilage in these structures, as well as the trachea, stops these conduits from actually closing, from collapsing during the breathing process. So they are very important to be supporting the open conduit. And again if you look very carefully in these sections, you can make out some very tiny pieces of cartilage or some more prominent pieces of cartilage. And that is because as you move from the trachea down into these bronchi, then you no longer have the horseshoe-shaped ring of cartilage. 01:31 The cartilage just becomes isolated plates as you move further and further down the bronchi tree. Smooth muscle is also prominent. It starts to appear in these bronchi and it becomes increasingly dominant as the bronchi move down to become smaller and smaller and smaller until they finally become bronchioles where the only main components supporting the wall of these bronchioles is smooth muscle. All the cartilage is absent. So the difference between a bronchus or bronchi and a number of these conduits and a bronchiole is the fact that the bronchiole does no longer have cartilage supporting it, it just has smooth muscle. 02:21 And this can be a problem, that smooth muscle can contract under various stimuli. Smooth muscle does not need necessarily just an innervation to contract. Various chemicals can make smooth muscle contract and this is sometimes deleterious. The asthmatic suffers because sometimes these smooth muscle contracts and therefore, closes the airway or the passage of air down these little airways, the bronchioles. Let us look at one of these bronchioles in more detail. 02:59 Bronchioles actually, originating from the bronchi form firstly terminal bronchioles. A terminal bronchiole then proceeds to branch into further bronchioles called respiratory bronchioles. And when one terminal bronchiole divides into a number of respiratory bronchioles that defines what we call the pulmonary lobule. It is because the lung originated from an outgrowth of the gut and develops like a gland. That is why we refer to the term lobule and in a moment acinus. And sometimes it is not surprising in the epithelium all the way through the respiratory tract they find enteroendocrine cells. We are not sure what they do, but they're present probably because of this fact that the lung developed as an outgrowth from the gut and developed as now a gland. One thing you notice on the slide is that the smooth muscle is arranged in certain orientations, in a circular manner and also in a spiral type of manner. And this helps to open and close effectively the airway so that air can then pass down into the alveoli below for exchange. There is also elastic fibers all the way through down to the very fine components of the alveoli. They help, when the lung expands during inhalation of air, and then breathe out expiration. Those elastic fibers help to recoil the structure, recoil these bronchioles and the alveolar and therefore, help to force the air out during expiration. They are absent or at least minimal in people who suffer from emphysema and therefore, that makes breathing and the exchange of gases very difficult in those individuals. The respiratory bronchioles branch into alveolar ducts and finally alveoli, that we will see in a moment. But one thing happens to the epithelium. Up until the terminal bronchiole, the epithelium has remained pseudostratified ciliated columnar, typical respiratory tract epithelium. Now the epithelium is going to change. It is going to lose the cilia, become more cuboidal and then finally it is going to become more squamous. Because now they are changing from being a conducting conduit, warmer, moisten and clean the air to being a conduit purely designed for the exchange of gases across the air sacs into the blood stream. 05:54 Sometimes those ciliated epithelial cells will be looking at in the respiratory tract at epithelium, they can change. They can go through a transformation. They can often become cuboidal or even stratified squamous in areas where there happens to be abrasion. The vocal cords, for instance, are lined by stratified squamous epithelium because that resists the abrasion of the air passing very quickly pass them. Other places around the larynx, the epithelium is pseudostratified epithelium. But in certain places there can be this change or transformation of the epithelium, for instance, a smoker. The smoke can change this epithelium. 06:40 Epithelial cells can lose their cilia and mucous secretion can seize and therefore the smoker has the typical smoker's cough because they do not have the mucous or the cilia to beat the debris back into the parts of the body where we can swallow or get rid of it. 07:00 Luckily the epithelium is rather versatile, it can renew those lost epithelial cells when they are given a chance to actually heal. One thing I want to point out on this slide before we move on is that the alveoli actually have little tiny pores, pores of Kohn. 07:19 They allow air to pass from one alveolus to another if there happens to be an obstruction in the alveolar ducts, those very small airways that deliver air to individual alveoli. Here is a diagram on the left hand side showing you the very top part, a bronchiole moving into a terminal bronchiole, then into respiratory bronchiole and then to the alveolar ducts and finally the alveolar sacs. And on the right hand side is the description of the epithelial changes. 07:58 The epithelium changes from the pseudostratified ciliar epithelium down to these cuboidal type epithelial cells and finally they are going to form very very thin squamous cells. Sometimes if you look at the respiratory bronchioles, and can just make out a very small slip of smooth muscle as that smooth muscle finally disappears. Now there are clara cells. Cells we call clara cells sitting in the epithelium and these are present also higher up in the pathways of the air. These clara cells secrete the surface active agent that stops the surface of these bronchioles collapsing, coming together, sticking together because there they moisten surfaces and that would not get any good. We would not want our airways to stick together and therefore, prevent air from passing down there. So these Clara cells secrete that agent that reduces the surface tension between the two surfaces. Well, now we go from the bronchiole into the alveolar sacs and the alveolar ducts all the passage ways where the exchange occurs. 09:14 And the bottom image you see there labels basically these terminal bronchioles and a few clara cells which are hard to see, opening into respiratory bronchioles, into passage ways and sometimes as I've mentioned before, very small slips of smooth muscle can be seen. 09:36 Those respiratory bronchioles then pass into the alveolar ducts. There are long corridors of very thin epithelial surfaces. The air passes along those corridors into all the alveolar sacs that branch out from them, or out pocketings of these alveolar sacs and this is where all the exchange occurs. In the alveolar ducts, the alveolar sacs and the individual alveolus or alveoli. Let us have a look at the surface of these alveoli.
About the Lecture
The lecture Bronchi and Bronchiole by Geoffrey Meyer, PhD is from the course Respiratory Histology.
Included Quiz Questions
Which of the following MOST ACCURATELY describes a pulmonary lobule?
- A cluster of up to 30 acini supplied by a common distal pulmonary artery and bronchiole
- A cluster of up to 30 acini supplied by a common distal pulmonary artery and bronchus
- One respiratory bronchiole and all the terminal bronchioles branching from it
- The lung unit distal to the respiratory bronchiole
- It is significantly smaller than an acinus, and is composed of alveolar ducts, alveolar sacs and alveoli.
Which of the following options provides the correct order of lung structures from proximal to distal?
- Terminal bronchioles, respiratory bronchioles, alveolar ducts, alveolar sacs
- Terminal bronchioles, respiratory bronchioles, alveolar sacs, alveolar ducts
- Respiratory bronchioles, terminal bronchioles, alveolar ducts, alveolar sacs
- Respiratory bronchioles, terminal bronchioles, alveolar sacs, alveolar ducts
- Terminal bronchioles, alveolar ducts, respiratory bronchioles, alveolar sacs
Which of the following best describes the shape of the cartilage in smaller bronchi?
- Irregular
- C-shaped
- Z-shaped
- Rings
- Longitudinal
Which of the following lines the inner layer of smaller bronchioles?
- Simple ciliated cuboidal epithelium
- Pseudostratified columnar epithelium
- Stratified columnar epithelium
- Stratified squamous epithelium
- Pseudostratified squamous epithelium
How are bronchioles histologically different from bronchi?
- Bronchiole walls do not have hyaline cartilage.
- Bronchiole walls have hyaline cartilage.
- Bronchiole walls do not have smooth muscle.
- Bronchiole walls have smooth muscle.
- Bronchioles are differentiated from bronchi based on size alone.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great lecture, for I learnt somethings from the lecture. Thank you Professor.