Playlist
Show Playlist
Hide Playlist
Cardiac Arrhythmia: Dysrhythmias and CSD
-
Slides CardiacArrythmia CardiovascularPathology.pdf
-
Download Lecture Overview
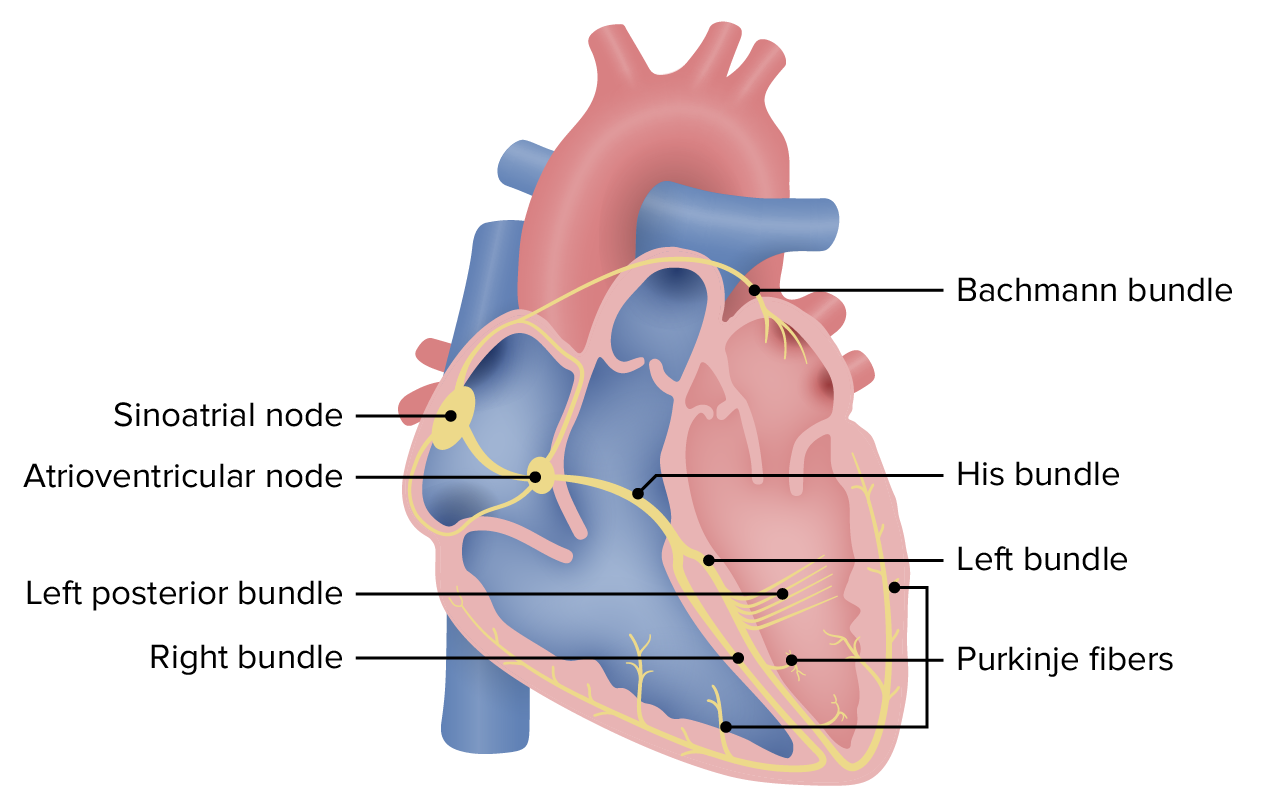
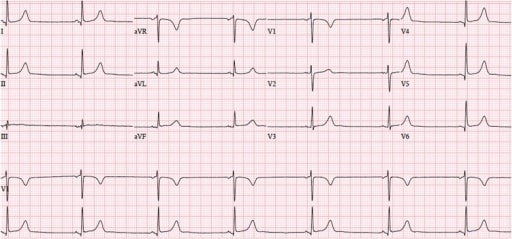
00:01 Now with Dysrhythmia and Conduction System. 00:03 What are the two ends of the spectrum? Either too slow or too fast. 00:10 With the bradyarrhythmia our topic will bring us to heart blocks. 00:15 With this most common type of blocks that we will take a look at AV nodal block, first-degree, second-degree. 00:21 With second degree will then divide that into mobitz. 00:24 But want to take a look at type one and type two. 00:27 and then we'll walk into our third-degree AV block. 00:30 On the other end of the spectrum to quick. 00:34 I'll quickly walk you through now press it reinforcement so that you feel comfortable with arrhythmia. 00:39 As soon as your atria -- well, what exactly are you going to be looking at, or interpreting so that you can figure out that your patient has an arrhythmia? How about an EKG? Would that come in handy? Sure it would. 00:50 So if you have an atrial type of arrhythmia, what kind of wave are you automatically looking at please? The P wave, right? Now, let's say that you add a fib. 01:01 Okay, not a fib where you're lying to yourself about anything but a fib in the sense of a fibrillation. 01:09 A fibrillation is one in which that wave has disappeared. 01:13 Is that clear? Or has become wavy. 01:16 Difficult to identify obscure. 01:18 Can we agree upon that? I hope so. 01:21 So if you have atrial fibrillation, what wave is this? The P wave is now become very obscure to identify. 01:27 Let's continue. 01:28 Atrial flutter. 01:29 You pay attention the two T's in the middle of flutter, okay. 01:33 And the reason for that is because you want to think of a saw tooth type of appearance of your P wave. 01:41 Why P wave? Atria. 01:43 Multifocal Atrial Tachycardia (MAT) This once again would be an issue with your atrium. 01:50 So what does the P waves look? They look abnormal. They look bizarre. 01:53 The P waves do. It doesn't touch the QRS complex. 01:56 Is that clear? And then we have WPW, Wolff-Parkinson-White Syndrome. 02:02 What is this? It's an accessory pathway. 02:04 What does that even mean Dr. Raj? It means that, remember, the proper conduction of an impulse is going to be from the SA node, you have to go to a delay. 02:13 Why do you need that delay at the AV node? Well, you need that delay so that you have just enough time as I squeezed the blood from the atria to the ventricle, right? You need just enough time and a delay in which you have enough time to properly fill up the ventricle. 02:28 Correct? Who is going to provide that delay? I believe it's called the atrioventricular node, the AV node. 02:35 Okay, that's perfectly normal, physiologic conduction. 02:39 What if you accidentally, inherently, ended up having an accessory pathway anywhere along the interatrial or should I say between the atrial and the ventricle? Alright, so if you had some type of accessory pathway on the septum or the wall, between the atrial and the ventricle, well, this will not provide a delay. 03:00 This is that accessory pathway that you're referring to. 03:02 And so therefore, we'll talk about this what's called as an AV nodal re entry type of arrhythmia. 03:08 Not good, not good. 03:09 And the particular characteristics that are very important for you to clinch WPW as diagnosis. 03:16 Okay, so that's the atria. 03:17 But in general, what's going on? Tachy. 03:21 To fast. 03:22 what's normal beats per minute? 60-100. 03:26 Okay, 60 to 100 is normal beats per minute. 03:30 So if it's tachy, greater than 100, by definition, automatically tachy. 03:35 Less than 60 automatically brady. Is that clear? So this is all greater than 100. 03:40 Ventricular. 03:41 What are you going to affect? What wave are you going to affect here with ventricular issues? Hopefully you're telling me, QRS. 03:50 Correct. 03:50 The QRS complex represents the activity of the ventricle. 03:55 So therefore, let's say that you have twisting around your point. 04:00 How do you say that in French? "To saw the point." You know, probably saying more Italian when I said it. 04:05 But it's French. 04:06 It is to saw the point, you're twisting around the point. 04:10 Who is? The QRS complex. 04:12 Wow, that's dangerous, isn't it? What predisposed to this? Most likely, maybe some kind of Long QT issue. 04:22 Alright. 04:23 So when the QT becomes more and more prolonged, Why? Oh, maybe drugs, such as antibiotics, such as antipsychotics, such as quinidine. 04:32 You have a bunch of drugs that may result in a Secondary Long QT. 04:38 Inherently, you can have genetic diseases. 04:41 You've heard of Romano-Ward, right, in which there's no deafness. 04:46 You've heard of things such as Lange-Nielsen So these are the inherent type of Long QT syndrome. 04:52 What does that even mean? The more that you prolong your QT, the QRS complex doesn't know how to behave. 04:59 So therefore, it starts twisting around the point. 05:01 Is that clear? So understand the most common predisposing factors, and once you do things become a heck of a lot easier. 05:08 Ventricular fibrillation. 05:09 Ah, you should feel very comfortable with the term fib. 05:13 Fibrillation. 05:14 What does that mean? An disappearance or obscure type of wave can talk to identify. 05:21 But in this case, if ventricular so it's difficult to identify the QRS complex. 05:25 Oh, my goodness. Picture this. 05:28 That QRS complex is difficult to identify. It's wavy. 05:32 That's almost like a flat line. What flat line mean to you? You're sleeping forever. You're dead. 05:38 So ventricle fibrillation, you worried about death, aren't you? You don't ever want to get to that point. 05:43 In fact, whenever you have any type of arrhythmia, and if it's originating in atria known as supraventricular arrhythmias, right. 05:52 Whenever you have supraventricular tachycardia is, what is your number one mission? What is your objective? You do everything in your power to prevent that arrhythmia from going into the ventricle? Because if it does, oh, my goodness, take a look at this ventricular fibrillation, you're going crazy. 06:09 Who is? The ventricles are. What does that mean? You can't properly fill up your ventricles with blood How on the world are you supposed to have cardiac output you don't. 06:17 Is your patient going to die? Yes. 06:19 Are you putting things together? I hope so. 06:22 Ventriclar tachy. 06:24 Well, just all this means that the QRS complex, the span between of them is getting very, very short. 06:29 The R wave to R wave, think about R wave, major positive deflection, the R wave to R wave is it going to shorten. 06:36 You might have heard of mnemonics or paramedics or whatnot there and they talk about 300 and 150, 100 and 75, 60, and 50. 06:44 Alright? It's like a phone number. 06:46 And what that means is the fact that the more number -- the lines, as I should show you an EKG, the lines when they're closer together, is that tachy, or is that brady? Please. 06:56 Tachy. Okay. And with that, I'll show you that coming up. 06:59 If you've missed it, that's okay. Don't worry. 07:01 I'm just introducing, what I like to do, as you know, is to bring information from before and then introduce information to be head, but ultimately, reinforcement. Let's begin. 07:12 So now, with vascular disease, the only other category here with arrhythmia, where let's say that you had a myocardial infarction, okay? Once again, let's say left anterior descending, you find an ST elevation. 07:22 And which leads would you find ST elevation, if your left anterior descending was undergoing infarction, A major, major embolic obstruction. 07:34 Got it. Good. What isi it? V1 through a V4. Are you picturing this? Good, so left anterior descending, and there's a myocardial infarction upon ST elevation in V1 to V4. 07:45 Okay, so that's your interventricular area, and maybe anterior apical. 07:49 And at some point, wow, this used to be called the widow-maker. Why? Because if the patient had an LAD top MI, chances are they're not coming back. 07:57 And it ends up where the spouse is lost. 08:01 Right? That's unfortunate. 08:02 My point is this though, if there is myocardial infarction and the wall is not working properly, could it result in arrhythmias, sure it can. 08:10 Other cardiac disorders that can cause arrhythmias include cardiomyopathy and the conduction system abnormalities that we just discussed. 08:17 Noncardiac disorders can also cause arrhythmias COPD is associated with multifocal atrial tachycardia or METI hyperthyroidism can cause atrial fibrillation channel properties and stimulants can cause taki arrhythmias. 08:30 And as strange as it sounds, antiarrhythmic medications can cause arrhythmias and even be pro arrhythmic in some cases. 08:37 Aortic Dissection. 08:39 This itself, let's say that you have an issue such as Marfan disease what's that called, when you have a little bit of tear and there's accumulation of fluid from the into the media, cystic medial necrosis may result in eventually, aortic dissection with vascular diseases, once again, if there is a proper blood supply to the heart, and you have origination of your arrhythmia. 09:08 Interesting, isn't it? Interesting. 09:10 So you can have these inherent causes that we just walked through, or vascular diseases, but you have to take a look at the body and totality for you to truly make sense of this
About the Lecture
The lecture Cardiac Arrhythmia: Dysrhythmias and CSD by Carlo Raj, MD is from the course Arrhythmias: Basic Principles with Carlo Raj.
Included Quiz Questions
What is the normal heart rate at rest?
- 60 to 100 beats per minute
- 30 to 60 beats per minute
- 100 to 120 beats per minute
- 150 to 200 beats per minute
- 120 to 150 beats per minute
Which of the following statements is true regarding atrial fibrillation?
- The pulse is irregular and rapid.
- The p wave is easily identified.
- Bradycardia is more frequent than tachycardia.
- It is a type of first-degree heart block.
- The heart rate is never within the normal range.
What structure slows down normal conduction?
- Atrioventricular node
- Sinoatrial node
- The Purkinje fibers.
- Bundle of His.
- Left atrium
Which of the following statements regarding Wolff-Parkinson-White syndrome is correct?
- Conduction occurs through an accessory tract.
- Conduction occurs through the AV node.
- PR interval is prolonged.
- The rate and rhythm are always regular.
- Q waves are seen.
Which of the following statements is correct regarding Torsades de Pointes?
- The QT interval is prolonged.
- The PR interval is prolonged.
- P waves are absent.
- The heart rate and rhythm are regular.
- It is an autoimmune condition.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
very well outline and simplified presentation. Good wits combined with serious discussion