Playlist
Show Playlist
Hide Playlist
Sleep-Wake Disorders – Consciousness (PSY)
-
Slides State of Consciousness.pdf
-
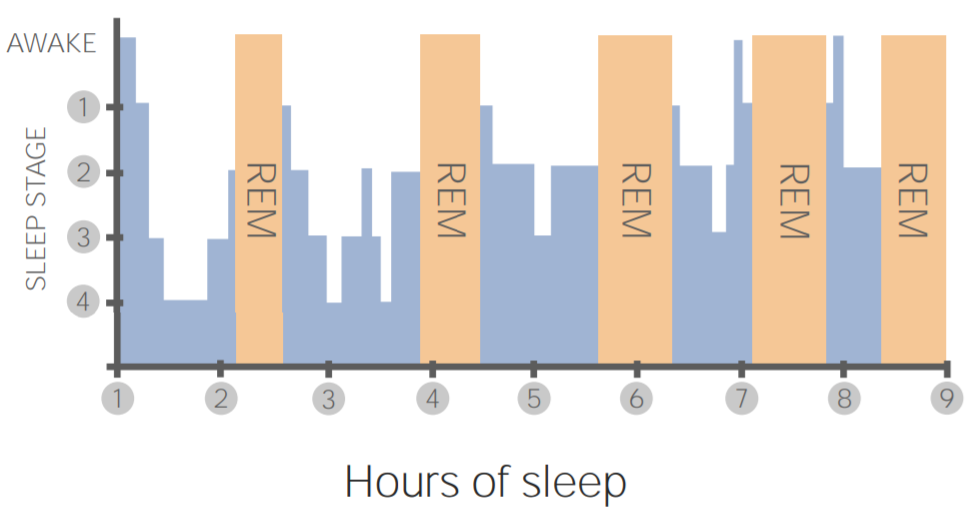
Download Lecture Overview
00:01 Let’s take a look at some sleep disorders. 00:04 Now, we can have two broad categories; we have dyssomnias and parasomnias. 00:08 So dyssomnias are abnormalities in the amount, quality, or timing of sleep. 00:14 So insomnia is a difficulty staying asleep. 00:18 So generally speaking, these are like basic attributes of sleep. 00:24 On the flipside are abnormal behaviors during sleep. 00:27 So, the two that I want to highlight here are the night terrors and REM behavior disorder. 00:32 So night terrors are when you’re having like really dramatic dreams. 00:36 And they’re not slightly scary. 00:37 These are terrors where you’re out of control, you’re screaming, and you’re acting out, behaviorally acting out and screaming at your dreams, and that’s tied into something called REM behavior disorder. 00:47 So remember I mentioned that REM is where you sleep -- is where you dream, sorry, and part of the self-preservation of REM is that it deactivates all muscle movements. 00:57 So, you’re basically paralyzed so that you don’t act out your dream. 01:01 Well, individuals with REM behavior disorder, they actually have an issue where this paralysis is lacking and they actually do act out their dreams. 01:11 So when they enter the REM state and if they’re dreaming of something, they’ll actually illustrate that movement and that behavior. 01:17 So one of the stories that I love to share when it comes to REM behavior disorder is with a patient that we had at our clinic, and I won’t actually say names because I’m not allowed. 01:26 But this patient was in for a sleep study but he was actually referred to us or mandated to come to us by the police. 01:36 So this happens time to time. 01:38 And the patient was completely unaware of why they were there. 01:41 So in our details in talking with them, we said, you know, “What’s going on and why are you here?” and he says, “I don’t know.” And he said that, “I’ve been told by my doctor and the police that I need to come for this test. I don’t know what this test is about.” And we said, “Okay.” So the backstory is with his wife. 01:57 His wife was going to the doctor and reporting a lot of bruising and pain and the doctor ran a whole bunch of tests and blood work and tried everything and nothing was solving the problem. 02:09 So then the doctor asked, “How are you sleeping?” And she said, “I sleep great.” And he asked her, “Do you dream? And do you remember all your dreams?” She goes, “Oh, I dream fantastic and, you know, like I’m getting my eight hours of sleep. No problems there.” And then the doctor said, “Well, how is your husband sleeping?” And she says, “My husband sleeps with me. We sleep fine. We don’t see any issues.” So after sort of exhausting all of his options with the patient, he moved onto -- onto him and said, “Well, bring in your husband and I’m just going to take a look at him.” And inspecting the husband, again, didn’t see anything obvious, so he sent them both to the sleep lab to come take a look. 02:45 So she slept. 02:46 She slept fine. 02:48 She went through all the stages of sleep and we didn’t see any issues. 02:51 He came in and he started going to sleep and he was all hooked up and we could see him cycling through the stages of sleep. 02:59 And when he entered REM, we realized that he was actually -- had REM behavior disorder because he was acting out his dreams. 03:06 Now, a little bit more backstories if you read his file, he happens to be 6’3” and a black belt in karate, and he mentioned this to me before he went to bed. 03:14 He said, “Listen, for any reason, if you need to come in, you might want to give me a heads up because I have a tendency to karate chop people because I’m a black belt.” So, kind of scary. 03:24 So when he went to sleep, we can monitor him on the screens and we could see that he was entering REM. 03:28 We can see that based on his brain activity, his EEG. 03:32 And what did we notice? We noticed kicking and wailing and he happened to karate chop the night lamp that was there and partially destroyed the room and he woke up in the morning and he said, “So, doc, how did everything go? How did I do?” And we said, “Oh, you did just fine.” And he said, “Well, there’s a lot of mess in here.” And we said, “Yeah, a little bit of mess.” And that was basically because he was karate chopping the room. 03:51 So what was happening was, back to our story, is our patient was experiencing REM behavior disorder and he was inadvertently, unconsciously hitting his wife, which explained the bruising, right? So the question you might ask is, well, how did she not know that she was getting karate chopped? And what happens a lot of times with couples if they’re going to bed together is they have synchronization of their sleep schedules. 04:13 So she was actually in REM when he was in REM, and she was unaware that she was taking a beating, which explained some of the bruising. 04:20 So I hope you kind of remember that story to highlight that REM behavior disorder. 04:25 Now, insomnia is difficulty falling or staying asleep and this is probably the most common sleep disorder that most people have. 04:33 It explains the multimillion dollar, billion dollar industry of sleep agents because they know that this is an issue. 04:41 So it’s different than occasional sleep issues related to, say, “I have a big test tomorrow like the MCAT and I can’t go to sleep.” You might have some short-lived acute insomnia. 04:51 We’re talking about something that’s a little bit longer, and this isn’t just happening, you know, a few days prior to your exam. 04:56 This is happening on a regular basis and it is a chronic issue and a lot of times this is linked to chronic stress or underlying chronic issues. 05:06 So if you’re in a really stressful position, like a lawyer or a doctor or a politician, you have a lot on your plate. 05:12 You don’t even have to be a professional, just as a -- as a, you know, as a parent. 05:16 You’re so concerned all the time about your children and how are we going to pay for bills and the mortgage and this and that. 05:21 That chronic stress actually can impact your ability to sleep and that’s expressed as an insomnia. 05:27 How do you deal with that? The obvious thing is good old medication. 05:31 And that’s a short fix because if the underlying issue is chronic stress, medication to help you fall asleep is not going to get you to where you need to be. 05:40 The other problem with medication is that it actually can influence the stages of sleep that you’re getting into. 05:44 So you’re getting the hours, but you’re not getting the appropriate stages. 05:47 So we say you’re getting quantity, but you’re not getting quality. 05:50 Because in order for you to feel rested and for sleeping to do what it needs to do, you need to hit stages one through three, plus REM. 05:57 And a lot of the medication prevents you from achieving REM, and so you’re getting stages one, two, three, one, two, three, and you’re not getting REM. 06:04 Another really important -- another very sort of useful tool is relaxation. 06:08 And this is when simple things like breathing and doing things like that really, really help. 06:14 We have a term called sleep hygiene. 06:18 And what that is, is we prompt individuals who have trouble sleeping to employ relaxation and to cleanse their sleeping area. 06:26 So that includes things like, you know, removing a whole bunch of stimulus, like all the lights. 06:30 Remove the lights. 06:31 You shouldn’t have your iPad with you. 06:33 You shouldn’t have an alarm clock blaring in your face with the time. 06:37 You should not be doing anything in your bed other than sleeping. 06:42 Obviously, a lot of us like this, some extracurricular activities, but that’s not what I’m talking about. 06:45 I mean you shouldn’t lie in your bed eating a, you know, a sandwich, watching TV, and reading a book an hour before you’re about to go to sleep. 06:52 So you should do that in the appropriate place, the kitchen or on a sofa or a lounge chair. 06:56 But when it’s time to go to bed, you go to bed in your bed. 07:01 You go to sleep in your bed. 07:02 So the idea is to create a relaxing atmosphere to be relaxed when you go to bed and not be thinking about the MCAT that’s happening tomorrow. 07:09 You also want to avoid stimulants before you go to sleep, so drinking a cup of coffee, having chocolate, having pop, going for a nice run. 07:18 These things are actually going to increase arousal and stimulation and that’s the opposite of what we’re trying to achieve. 07:24 Another disorder is something called narcolepsy, and this a periodic overwhelming sleepiness during waking periods and is usually in response to a stimulus. 07:34 So what we’re referring to here is the sudden loss of muscle control. 07:39 So we call that cataplexy or sudden transient muscle weakness and it’s linked to a dysfunction of a region within the hypothalamus which produces a compound called orexin. 07:49 We don’t need to go into all the specifics. 07:51 Just kind of be aware that narcolepsy is linked to cataplexy which is driven by orexin. 07:56 And it’s a fairly alarming and odd scenario that you’re speaking to somebody. 08:01 You might tell them a joke or they might get startled by somebody walking in. 08:05 And that sudden activation actually knocks them right into REM sleep and that they’re completely in cataplexy. 08:11 So they’re completely out. 08:13 Now, this is a potentially dangerous situation if you can imagine somebody with narcolepsy driving a car. 08:20 And they’re driving a car and unexpectedly somebody honks a horn, they’re startled, and they fall asleep at the wheel. 08:26 Kind of an obviously a dangerous situation and this happens quite often. 08:31 Now, the interesting point is they don’t just kind of slightly doze off. 08:33 They dramatically fall into sleep and enter REM very, very quickly. 08:37 Okay. So that’s not typical. 08:39 Typically, you want to cycle through the stages of sleep and get to REM. 08:42 In this scenario, they’re getting to REM quite, quite quickly. 08:46 Now, another extremely prevalent disorder that’s surfacing lately over the last, I would say, 15 years is sleep apnea. 08:54 And this is when you intermittently, periodically stop breathing during sleep. 08:59 Now, you might say, “Well, what’s the big deal if I kind of stop breathing a little bit here and there?” Well, we’re not talking about the occasional, you know, you stop breathing. 09:07 This is very, very dramatic and this is happening throughout the night. 09:10 So episodes can last from seconds to just over a minute. 09:13 So we had this kind of, I don’t want to say a contest, but a running tally of the longest apnea event that we’ve ever had at our -- at our sleep institute and it was a minute and thirty two seconds. 09:25 Again, you might say, “What’s the big deal? A minute and a half almost.” Well, right now at your desk, I want you to hold your breath and hold it just for five seconds. 09:33 Okay? So let’s do that. 09:38 Okay. That was five seconds. 09:40 How do you feel right now? I’m not saying you’re completely winded, but you can feel the effects of just holding your breath for five seconds. 09:45 Now try that for 20 seconds. 09:47 And after the 20 seconds, what do you do? You’re like -- okay, I’m good, I’m good. 09:51 Now, a minute and a half is a long period of time, and this isn’t just happening once. 09:57 This happens repeatedly over and over throughout the night. 10:00 Sometimes 80, 100, 140 times. 10:05 So what this actually does is two things. 10:07 One, it’s physically draining, you’re quite tired, and you’re not getting the oxygen that your body needs. 10:13 So normally when you’re breathing, you’re bringing in oxygen, you’re expelling carbon dioxide. 10:16 So you’re bringing in oxygen, which your body needs very badly, and you’re expelling the waste product of carbon dioxide. 10:22 So you’re not allowed to do that. So that’s not a good thing. 10:24 The second thing that it does is it actually causes an awakening. 10:27 So you might be in a deeper stage of sleep, stage three for example, which is that restful, restorative stage of sleep, and all of a sudden, you have this apnea event where you stop breathing. 10:37 And then, the way you get out of apnea is there’s a deep part of your brain that handles autonomic functions, so the basic things like breathing and blood pressure. 10:47 It detects that you’ve stopped breathing and it kicks you back in. 10:50 And so what you typically do is you’re -- and then you start breathing again. 10:53 Now that action is enough to kick you out of the deeper stage of sleep into a lighter stage of sleep. 10:59 The majority of people who have apnea are unaware that they have apnea, and so, they come and say, “I don’t know what’s wrong with me, but I’m bushed. 11:05 I’m just exhausted. I’m getting eight, nine hours of sleep, but I wake up and I’m done. I have zero energy.” And it’s because, again, they’re getting quantity, eight hours, but they’re not getting quality because they keep getting bumped out of that lighter stage of sleep, not enough to wake them up, but enough to get them out of that deep stage of sleep. 11:23 The events are repeated throughout the night, and this is accompanied a lot of times by heavy, heavy snoring. 11:28 Now, apnea is linked to snoring, and snoring and apnea is linked to obesity. 11:35 And generally speaking, in North America, that is a huge epidemic right now, is increasing and increasing amounts of obesity. 11:41 As obesity goes up, health outcomes go down, snoring and apnea events are going up. 11:47 So it’s extremely, extremely prevalent now these days. 11:50 You know, 15 years ago, we would see, you know, a certain amount of apnea patients. 11:54 We’ve seen probably in the last 10 years a doubling of that. 11:58 So what is the treatment? The obvious treatment is just straight up weight loss, so lifestyle changes. 12:02 Lose a little bit of weight and become a little bit more active, eat a little bit a better, you’ll lose weight. 12:06 And the weight that we’re talking about, there are two places, is right around your neck and the weight around your chest and abdomen. 12:13 So, all that weight, when you lie down, falls on you. 12:15 And actually, what it does is, it prevents your airway from working well and it collapses it. 12:21 So another option is something called CPAP. 12:24 It’s where you wear a mask and it’s attached to a machine, and the machine delivers positive air. 12:29 So that’s where you get the abbreviation of CPAP, it’s continuous positive airway pressure. 12:35 And CPAP is delivering this air and is preventing your airway from collapsing and it’s keeping it open. 12:40 So the analogy I always use when I try to explain this to people is imagine sticking your head out of a moving car going down the road, going down a highway, so you’re going fast enough and when you try to breathe. 12:49 The air is being forced up your nose and mouth. 12:51 So it’s like trying to breathe in, which is easy when it’s blowing at you, and trying to breathe out against the air that’s coming at you when you’re driving down a highway. 13:00 Okay? So again, what it does is it prevents the airway from collapsing.
About the Lecture
The lecture Sleep-Wake Disorders – Consciousness (PSY) by Tarry Ahuja, PhD is from the course Making Sense of the Environment.
Included Quiz Questions
Which of the following is considered a dyssomnia?
- Insomnia
- Somnambulism
- Night terrors
- REM behavioral disorder
Peter, an overweight, middle-aged man, complains that he is always tired in the morning despite sleeping for 8 hours. Which characteristic is unrelated to the likely cause of his sleep difficulties?
- It is classified as a parasomnia.
- It is associated with loud snoring.
- It is caused by brief periods of apnea.
- This condition is managed with continuous positive airway pressure (CPAP).
- The body's response to apnea kicks the patient out of deeper stages of sleep.
Amy comes to the clinic saying that she is having difficulty staying asleep and is tired during the day. What is the most effective long-term treatment for her dyssomnia?
- Improving sleep hygiene
- Drinking a glass of wine before sleeping
- Using stimulant medications
- Watching TV in bed
- Taking sedative medications
Jane says that she suddenly feels extremely tired and falls asleep during the day despite having 8 hours of sleep at night. Which of the following statements is false?
- REM behavior disorder is a similar sleep disorder.
- It can be triggered by sudden movement or sounds.
- It can occur in potentially dangerous situations, such as driving a car.
- It is linked to dysfunction of a region within the hypothalamus that produces orexin.
- Episodes can be associated with a sudden loss of muscle strength.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text