Playlist
Show Playlist
Hide Playlist
Type 2 Diabetes: Diagnosis and Management
-
Slides Diabetes ChronicCare.pdf
-
Download Lecture Overview
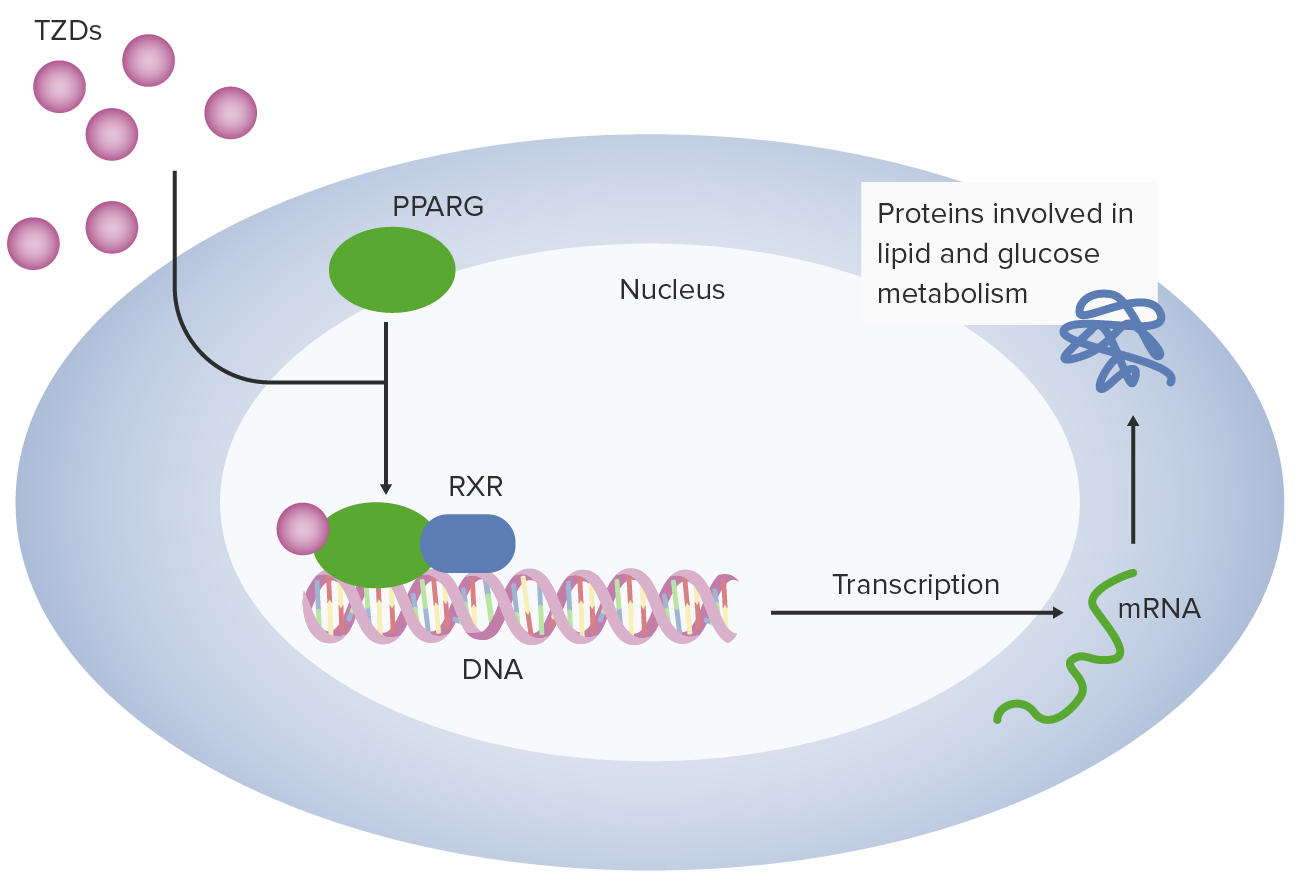
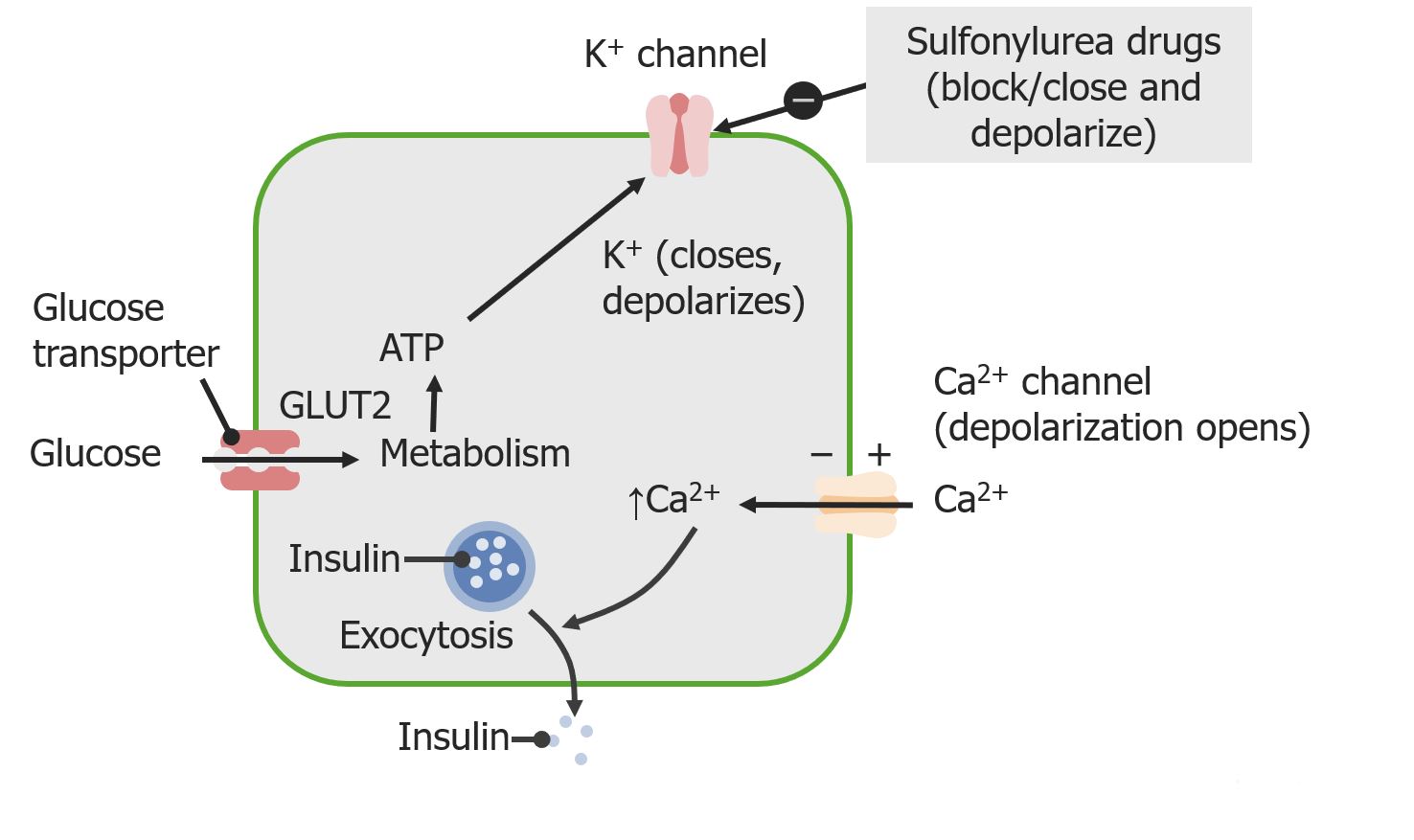
00:01 So, how do we diagnose diabetes? So, it’s a serum glucose level of 126 mg/dL or 7 mmol per liter on two separate occasions. 00:12 Or it could be an HbA1c of 6.5% or more on two separate occasions. 00:16 But if a patient comes in with fatigue and polyuria and polydipsia and you check their glucose in the clinic and it's over 200 mg/dL, no further testing is necessary. 00:29 They have diabetes. 00:31 Of course, those patients will get a baseline HbA1c level right away as well. 00:35 So, I think this is good for patient care and also good for what may come up on your exam. 00:42 This is the routine evaluation for patients with diabetes with a schedule. 00:46 So, patients with Type II diabetes get their - an ophthalmologic exam right away when they're diagnosed with a dilated pupil for retinal exam. 00:56 And then, that's followed at least annually. 00:58 The HbA1c, if it’s well-controlled, can be every six months. 01:03 Poorly controlled, every three months. 01:05 A complete foot exam with monofilament testing, at least every year. 01:10 Lipids, at least every several years. 01:13 I probably draw them more often. 01:15 A urine, microalbumin, creatinine ratio at the time of diagnosis and then annually. 01:21 And then blood chemistries and renal function at least every six months. 01:24 All those things fairly straightforward and make sense. 01:26 Most of my patients are achieving those goals. 01:29 Now, we do an HbA1c level and it turns out it’s 8.2%. 01:34 So, besides lifestyle intervention, what's the best treatment to prescribe for this patient now? Is it, A, glipizide; B, Liraglutide; C, a basal insulin at night; or D, metformin? And in previous years, you can make an argument as to which one might be better. 01:53 Now, it's fairly clear and the American Diabetes Association recommends, along with the American Association of Clinical Endocrinologists, metformin as a foundational drug for diabetes. 02:05 So, we’ll talk about different interventions for diabetes with medicines in a second, but you always start with lifestyle first because, just think about it, a multidisciplinary team can promote weight loss of up to 9% among patients with diabetes, and that's going to reduce the need to use anti-diabetes drugs and anti-hypertensive drugs as well. 02:27 Physical activity is about as good as one of the weaker oral agents for reducing HbA1c. 02:34 And diet advice is similar. 02:37 It can reduce the HbA1c by another 0.5% to 1% for most people. 02:42 And it probably is better when it comes from somebody with experience in counseling patients, like a dietitian or a certified diabetes educator versus a physician who is trying to manage 20 things at once. 02:54 A little pearl regarding home glucose testing, we recommend this broadly and probably a little too broadly. 03:02 Just in terms of stewardship of resources, because it can get expensive to get new machines, to get the lancets, to get the test strips, it’s most helpful for patients with severe diabetes who are taking insulin. 03:16 It hasn't really been shown to make much of a difference among patients who are fairly well controlled on oral medications, especially those early in their illness and it doesn't necessarily change quality-of-life. 03:28 Where I might use it in a patient who is on oral medications alone are patients with highly fluctuating glucose going very high and then at risk of hypoglycemia or for somebody who's chugging along and taking only Metformin and their HbA1c is 6.8% to 6.6% every time I check it. 03:48 There's not really much of a need to do any home glucose testing at all. 03:53 So, something to think about. 03:55 And I mentioned metformin is the first-line agent. 03:59 Why? There's a low risk of hypoglycemia. 04:02 Hypoglycemia and its danger has become a lot more apparent over the past few years and we’ll talk about some agents that promote low sugar. 04:10 It's usually associated with a very modest weight loss. 04:13 It doesn't create the cycle of more weight gain, therefore, more insulin resistance and then more need for drugs. 04:20 And the big complication with metformin that everybody worries about is lactic acidosis. 04:28 That’s right. 04:29 And it’s more common among patients with severe kidney disease. 04:33 But now, the new rules and warnings on the drug state that it can be used for certain patients all the way down to a glomerular filtration rate of 30 mm/m. 04:44 So, that’s kind of remarkable and a big change, getting metformin to more patients who need it. 04:49 Sulfonylureas have been around a long time. 04:52 Like metformin, they’re inexpensive. 04:54 And like Metformin, they promote about the same degree of HbA1c reduction. 05:00 If you ever get stopped and have to answer in like half a second, okay, how much does this drug reduce - this oral drug reduce HbA1c? 1% is always a good answer because they tend to be around that level. 05:12 But the problem with sulfonylureas is they can promote hypoglycemia and weight gain, and therefore, are maybe less favored. 05:19 There’s also an unknown effect whether they improve mortality or not. 05:23 Newer agents now. 05:26 Dipeptidyl peptidase-4 inhibitors. 05:29 These are - I think the benefit to these drugs is they’re really well-tolerated and they’re fairly easy to use. 05:34 Don’t promote a lot of hypoglycemia. Low rate of side effects overall. 05:38 They can even be used in moderate renal dysfunction as well. 05:42 The drawback, they're not that effective. 05:44 So, they're good for patients who are right next to gold maybe with metformin, but can't quite get there, but they also have intolerance to multiple drugs. 05:52 A DPP-4 inhibitor could be a good idea for them. 05:56 Thiazolidinediones, only rosiglitazone is available in the United States. 06:03 These drugs can promote weight gain, which is partly water weight. 06:07 They can promote edema. 06:08 Patients with a history of bladder cancer or osteoporosis should not be using these drugs. 06:13 And they reduce HbA1c by about 1%. 06:16 So, these still have some role, but it's probably a more limited secondary role in the management of most cases of Type II diabetes. 06:24 Thiazolidinediones should also be avoided in patients with severe heart failure. 06:29 What about the glucagon-like peptide-1 receptor agonists? So, these are different drugs. 06:33 These are again even a newer wave. 06:35 They've been out for several years now. 06:37 So, it's important for us to know them. 06:39 Different dosing schedules, but they are not - there is no oral product out there right now. 06:44 There are subcutaneous injections. 06:46 They rarely are associated with pancreatitis and you can’t use them on patients with the most severe chronic kidney disease, but they can be used in moderate kidney disease. 06:57 The beneficial effects of GLP-1 agonists, they can promote weight loss. 07:03 Sometimes, it exceeds 6 or 7 kg. 07:06 Routinely, it's going to be at least 4 kg. 07:09 So, weight loss is important. 07:11 It's something that patients can really hold on to. 07:13 It's not easy to lose 4 kg of body weight for many patients. 07:17 And their HbA1c action is a little bit stronger than other oral agents. 07:22 So, between the fact that it promotes weight loss and it reduces A1c fairly robustly, I like GLP-1 agonists. 07:31 Another new kid on the block, the sodium-glucose cotransporter-2, or SGLT2 inhibitors, these inhibit glucose reuptake. 07:39 They work in the kidneys. 07:40 They have been associated with a higher risk for UTI as well as genital fungal infections. 07:46 These also promote weight loss though, as well as they lower blood pressure in and of themselves too. 07:52 Again, a little bit weaker though for their HbA1c reduction. 07:57 So, not something - not that strong reduction you might experience with a GLP-1 agonist.
About the Lecture
The lecture Type 2 Diabetes: Diagnosis and Management by Charles Vega, MD is from the course Chronic Care. It contains the following chapters:
- Type 2 Diabetes
- Taking Care of Diabetes
- Treatment of T2DM
Included Quiz Questions
All EXCEPT which of the following screening tests are generally indicated with a new diagnosis of type 2 diabetes?
- Echocardiography
- Lipid profile
- Ophthalmologic exam
- Urine albumin-to-creatinine ratio
- Serum creatinine
A 45-year-old man who was diagnosed with diabetes 3 months ago presents for follow-up after 3 months of diet and lifestyle modification plus pharmacotherapy. In addition to a HbA1c of 8.2% at the time of diagnosis, he had normal general tests including lipid profile, creatinine, urine albumin-to-creatinine ratio, and liver function tests. Which of the following tests is most appropriate at this time?
- HbA1c
- Lipid profile
- Creatinine
- Liver function tests
- Urine albumin-to-creatinine ratio
Which of the following diabetes drugs is/are associated with weight loss?
- Metformin, glucagon-like peptide-1 receptor agonists
- Metformin, thiazolidinedione
- Insulin, sodium-glucose co-transporter 2 inhibitors
- Thiazolidinedione, sulfonylureas
- Sulfonylureas, metformin
Which of the following antidiabetic medications is most likely to cause fluid retention, especially in heart failure?
- Thiazolidinediones
- Dipeptidyl peptidase-4 inhibitors
- Glucagon-like peptide-1 receptor agonists
- Sulfonylureas
- Sodium-glucose co-transporter 2 inhibitors
Which of the following is a contraindication to metformin use?
- Estimated glomerular filtration rate [eGFR] <30 mL/min/1.73 m2
- Morbid obesity
- Obesity
- History of hypoglycemia
- History of pancreatitis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
hello i was really good engoy makes me happy when i amsw. abd memorise
The lecture is clear and concise. Helpful before my rotation to family medicine.