Playlist
Show Playlist
Hide Playlist
Large Vessel Vasculitides: Takayasu's and Giant Cell Arteritis
-
Slides Vasculitis.pdf
-
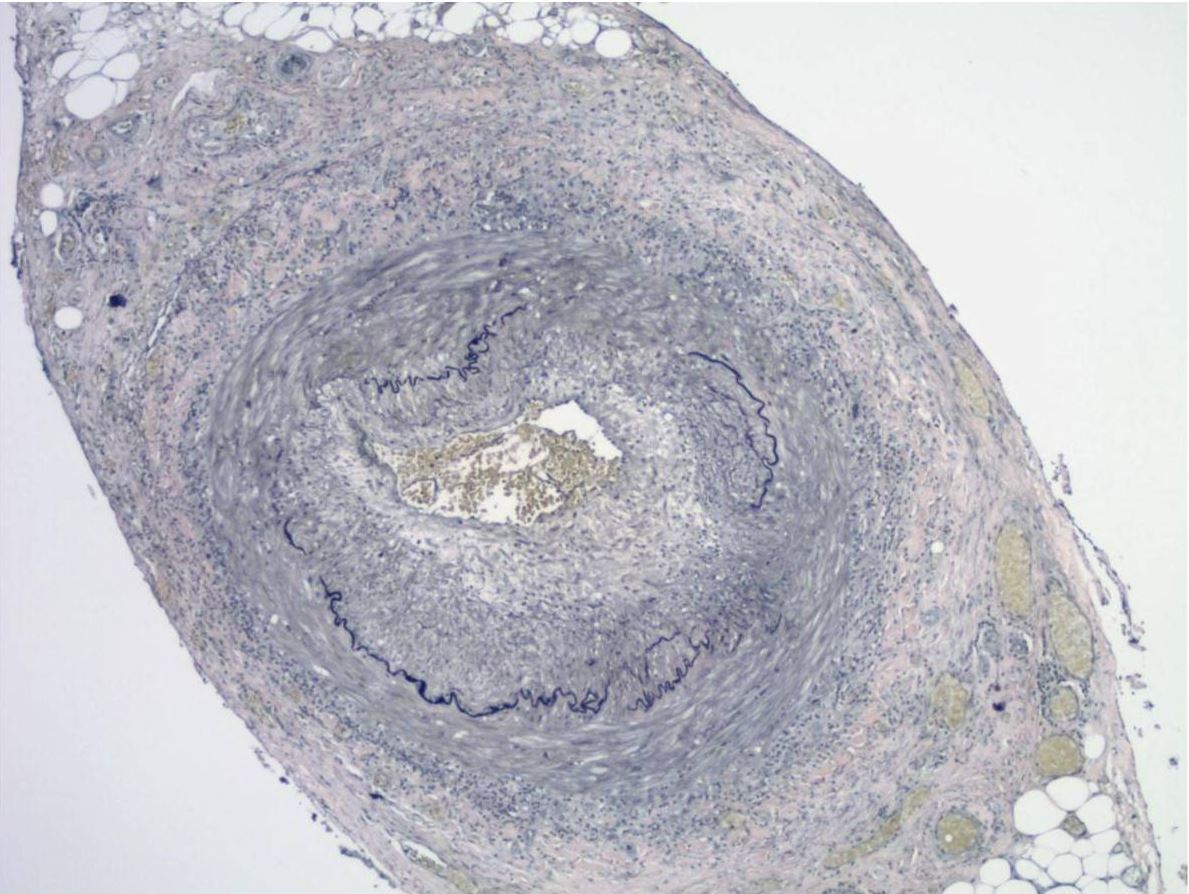
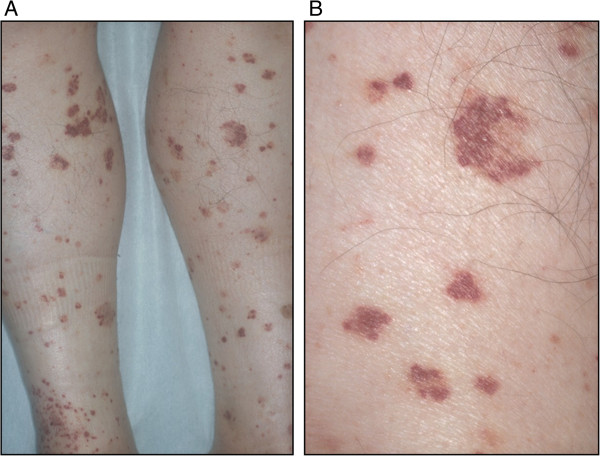
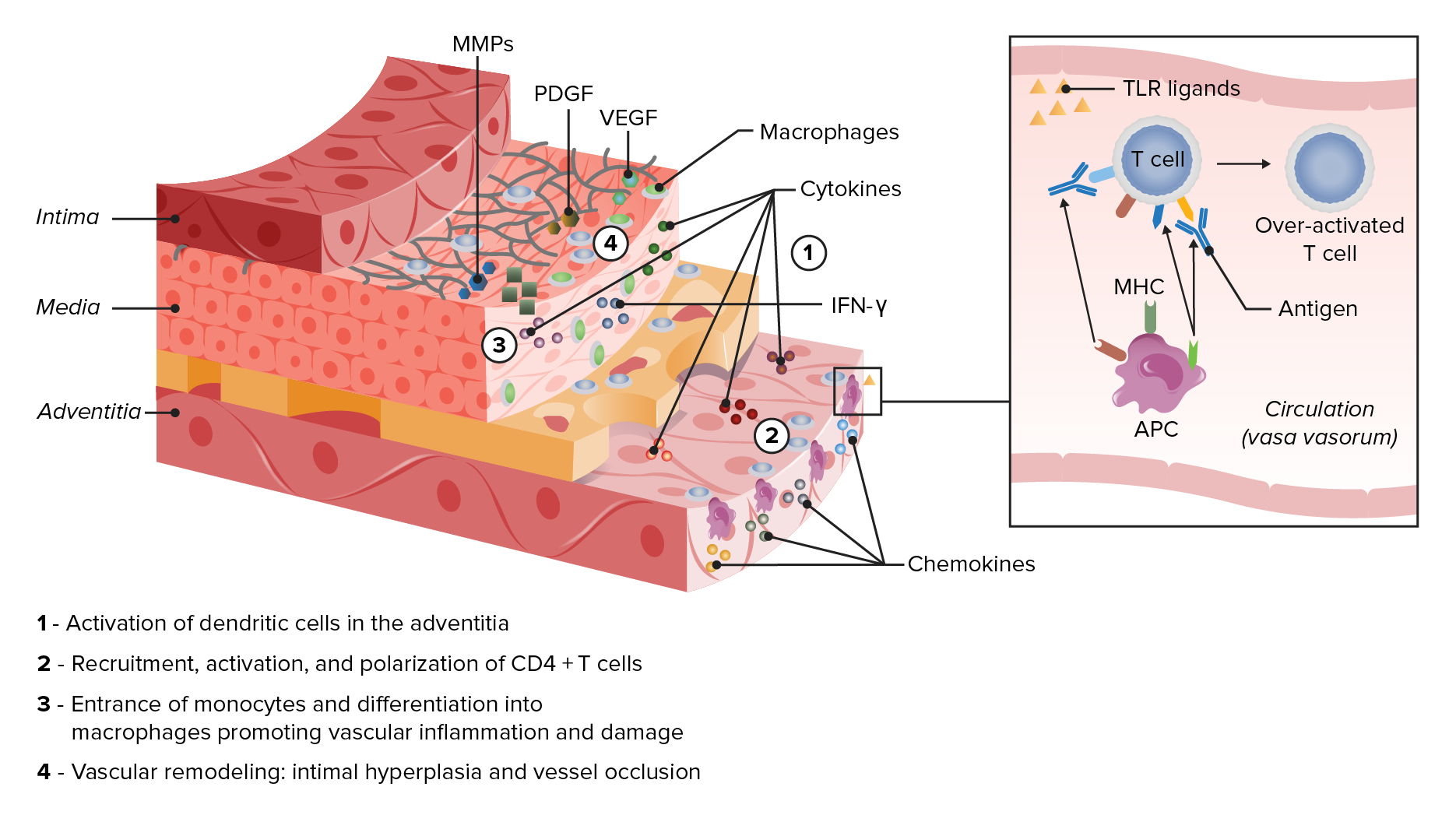
Download Lecture Overview
00:00 Alright, Takayasu's first. So, Takayasu's, as we've discussed, is a large vessel vasculitis and by being a large vessel vasculitis that means it's affecting things like the aorta and other major vessels like the brachiocephalic, the carotids, et cetera. 80%-90% of patients with Takayasu's are women typically between the ages of 10 and 40. Classically, it's associated with folks of Asian ancestry. On the one hand, our patient does meet the demographics, she is a woman, she is between the right age, and we aren't explicitly told where she's from so certainly this is a likely scenario for her. Takayasu's, unlike something like polyarteritis nodosa, can have a really indolent course over months even years before you start to make a diagnosis. It's going to present with constitutional symptoms which again can be fairly indolent. You may have limb claudication or cyanosis which, as you might imagine, would be problems with disease of the right and left subclavian or lightheadedness due to disease of the carotids. Abdominal pain, nausea, vomiting, that will be in particular if the abdominal aorta is involved where the mesenteric vessels are coming off. Hypertension if there is renal artery involvement or arthralgias which it's hard to make sense of why those occur but they do occur in about 50% of patients. 01:25 On physical exam, you're going to be looking for weak pulses particularly discrepantly weak pulses, one side worse than the other, likewise having discrepant blood pressures. It's reassuring that our patient has the same blood pressure on both sides. You might also be looking for an aortic insufficiency murmur which would suggest involvement of the aortic root and you should also palpate and auscultate for bruits over the carotids, perhaps over the aorta, the renal arteries, et cetera. This diagnosis is going to be made by magnetic resonance arteriography of the arterial tree. I mean you can imagine, biopsy of the aorta very impractical. That being said, for post-mortem specimens they found that there is infiltration with cytotoxic lymphocyte into those large vessels; the subclavian, the aorta, the carotid, brachiocephalic. And on imaging, you're going to see narrowing or occlusion and aneurismal dilatation of these vessels. What we can see in our image here on the right is significant narrowing with beaded aneurismal dilatation of the left subclavian. This diagnosis, just like some of the other vasculitides, will be treated with corticosteroids. Of course if you got a significant large vessel involved that's otherwise progressing rapidly, you may need to consult your cardiothoracic surgeon and have angioplasty or bypass. Alright, now let's move on to giant cell arteritis. While a large vessel vasculitis, giant cell arteritis, that can affect the very same vessels as Takayasu's, most of the symptoms of giant cell arteritis come from involvement of smaller cranial branches of the internal and external carotid arteries. Otherwise, it's histopathologically indistinguishable from Takayasu's. It is in fact the most common systemic vasculitis so when you're thinking about epidemiology this is the one you're most likely to see over the course of your career. It has a rising incidence after age 50. So that should already raise some flags for the case that we're talking about now though there is a 3:1 female predominance. Patients with giant cell arteritis tend to have a fairly subacute course over weeks to perhaps months and they're going to present with constitutional symptoms, weakness, malaise, perhaps low grade fevers, headache, jaw claudication, and vision loss. 03:48 Of course the vision loss can be from ischemic optic neuropathy typically due to occlusion of the posterior ciliary artery. This is a branch of the ophthalmic artery. The posterior ciliary artery is feeding the optic nerve. So that's the thing that we're most concerned about would be acute vision loss. It's also important to mention here that many patients with giant cell arteritis, about 50% in fact, will have associated or concomitant symptoms of polymyalgia rheumatica and those are folks who have inflammation and pain with shoulder girdle and the hip girdle, one of the rheumatologic diseases that we associated with this condition. About 10% of folks with just polymyalgia rheumatica will manifest with giant cell arteritis as well. On physical exam, you're really going to look for tenderness over the temporal arteries. You're not going to be able to appreciate tenderness over the ophthalmic artery so that's why you really have to do the things that are available to us. Along the same lines, the temporal artery biopsy is performed because that's the only affected artery that's actually accessible. If you were to perform imaging, you could use an ultrasound which would potentially show luminal narrowing, some intimal thickening on the ultrasound. Depicted here on the right, you can see significant luminal narrowing. 05:07 You can barely make up the lumen of this temporal artery at all. There is a lot of infiltration of the inside of that vessel. Here, you can actually see the multinucleated giant cells that earn the disease its name, shown at the green arrow. And finally, treatment, again you're going to use corticosteroids just like we would for Takayasu's arteritis. Alright, well, the age issue clearly takes out giant cell arteritis and our patient doesn't really seem to fit with any of this large vessel involvement either. So, we can take Takayasu's and giant cell arteritis off of our list. Alright, let's take a look at cryoglobulinemic vasculitis.
About the Lecture
The lecture Large Vessel Vasculitides: Takayasu's and Giant Cell Arteritis by Stephen Holt, MD, MS is from the course Vasculitides.
Included Quiz Questions
Which of the following is the most common systemic vasculitis?
- Temporal (giant cell) arteritis
- Takayasu arteritis
- Kawasaki disease
- Buerger disease
- Granulomatosis with polyangiitis
Which of the following is most commonly associated with giant cell arteritis?
- Polymyalgia rheumatica
- Dermatomyositis
- Polymyositis
- Mixed connective tissue disease
- Sjögren syndrome
Which of the following is used for the treatment of giant cell arteritis?
- High-dose steroids
- Aspirin
- Intravenous immunoglobulin
- Cyclophosphamide
- Acetaminophen
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |