Playlist
Show Playlist
Hide Playlist
Aortic Dissection: Surgery & Medication
-
Emergency Medicine Aortic Dissection.pdf
-
Download Lecture Overview
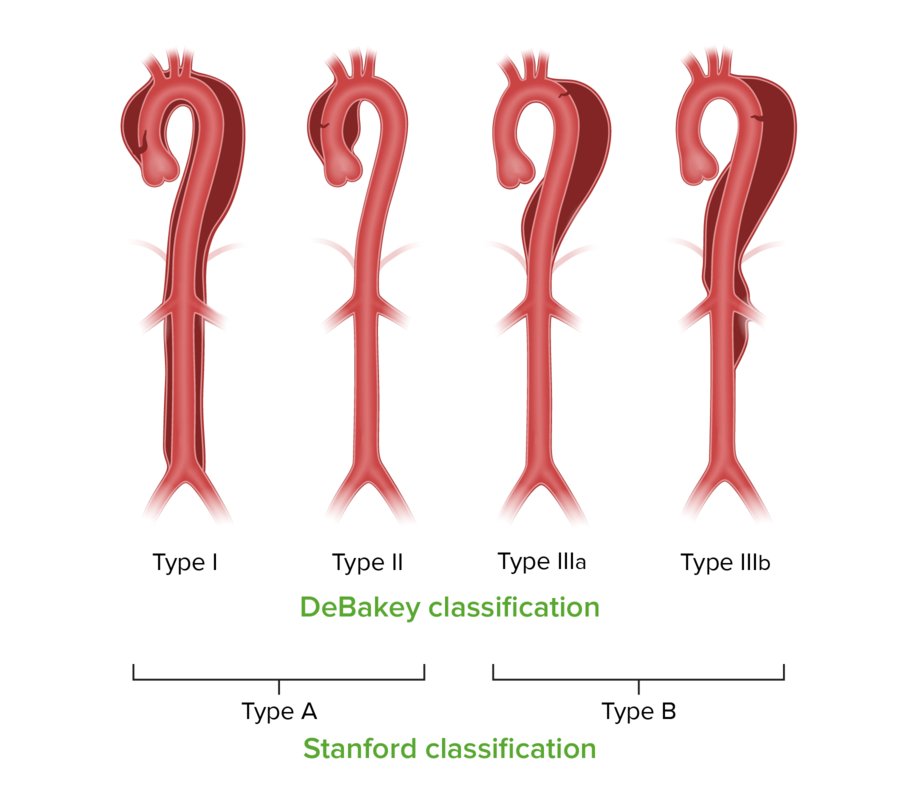
00:01 So what do we do about dissections? Well, like I said, it's based on classification, so all Type A’s require emergent surgical intervention. 00:09 If your ascending aorta is involved with the dissection, it needs to be managed operatively. 00:15 Type B’s, are typically managed medically except in the case of complications and we'll talk about that in a second. 00:22 For ED purposes we're gonna manage all dissections the same way with the one important exception of consulting cardiothoracic surgery for patients who do require surgical management. 00:35 We should also remember that aortic dissection is always an emergency, so just because your patient presents stable right now, it doesn’t mean they're gonna be stable 30 minutes from now, and it's really, really, important that you expedite treatment for this patient and take this disease process very seriously. 00:52 So as far as what we're gonna do for these patients in the ED we're gonna of course give them oxygen to ensure adequate saturation and optimize oxygen delivery to the organs. 01:04 We're gonna have them on cardiac monitors and we're gonna really keep a hawk’s eye on their vital signs. 01:10 Patients with aortic dissection can decompensate very quickly, and we wanna make sure that we are completely on top of their physiologic status at all times. 01:19 We wanna make sure we have adequate vascular access. 01:21 We talked about what that means before, but just to remind you that is two large bore IVs at minimum or central access. 01:29 So we really wanna make sure we have stable, reliable, large bore access so that if we need to we can rapidly resuscitate the patient with fluids or blood. 01:38 Speaking of blood, we wanna make sure we have typing cross matched. 01:42 And we wanna cross match the patient for a significant number of units of blood, typically four to six. 01:47 Remember one of the risks of aortic dissection is rapture of the aorta, and as you can imagine that's gonna lead to significant blood loss and we wanna be prepared to deal with that if it happens. 01:59 If the patient is hypotensive we definitely wanna give them IV fluids and or blood if we're concerned about the possibility of rupture, and we wanna keep a very close eye on their hemodynamic status. 02:11 We're always gonna monitor urine output because the aortic dissection can involve the renal vessels and we wanna make sure that we're not missing any early evidence of renal ischemia. 02:21 And we wanna place an arterial line so that we can really keep minute to minute tabs on our patient's blood pressure. 02:28 It's not good enough to be checking blood pressures every few minutes in these patients. 02:31 We really wanna know from one minute to the next what's gonna with their blood pressure because as you'll see in a moment medical management involves blood pressure optimization. 02:42 So when do we consult our surgical friends? Like I said before, for any type A we're gonna contact immediately. 02:49 If it involves the ascending aorta we need to make sure we get surgery on board. 02:54 And that's because these patients are at very high risk of developing cardiac complications. 02:59 Cardiac tamponade, myocardial ischemia, or acute aortic valvular insufficiency. 03:05 All of these can be deadly complications and we wanna make sure that we have a surgeon on board to help us deal with them. 03:12 For Type B’s, the management is gonna be primarily medical. 03:16 So we're really gonna involve surgery if we have a complication or we suspect an impending complication. 03:23 So patients who are ruptured or we suspect may have impending rapture, we're gonna get surgery involved. 03:29 If the dissection is rapidly propagating so their clinical status is changing, there is evidence of new vessels getting involved, we're gonna want surgery to help us out there. 03:39 If they have an enlarging wall hematoma that's the sign of active bleeding and again may merit surgical consultation. 03:46 If they're developing aneurysmal dilation of the aorta that could place us at risk for rupture and we wanna get surgery involved for that. 03:54 And if there's any compromise of major aortic branches, so if they're infarcting their mesenteric vasculature, if they're infarcting their kidneys, if they're showing stroke symptoms, we wanna consider whether surgery might be warranted in those patients to limit the extent of propagation of the dissection. 04:15 So for Type B's, any rupture, any bleeding, any significant complications, get surgery on board. 04:25 And when in doubt, it's always a good idea to involve a surgeon. 04:29 The worst thing they're gonna say is, "No, we don’t need to do surgery for this," but you definitely wanna make sure that you have them on board for any case where you suspect you might. 04:38 As far as our medical management goes, our biggest goal is to stop further propagation of the dissection and to prevent rupture. 04:46 So we can't do anything about the blood that's already dissected into the aortic wall, but we wanna keep that dissection from getting bigger and involving more of the aortic branch vessels. 04:56 And we wanna prevent aneurysmal dilation and rupture. 05:00 The way we do that is by decreasing blood pressure so we wanna lower the hydrostatic pressure inside of the aorta and we wanna decrease the shear force on the aortic wall from cardiac contraction. 05:11 So basically lower the pressure so less blood is pushed out and decrease the continual shear stress on the wall by causing the heart to beat a little bit less forcefully. 05:22 The best way to accomplish both of those goals with a single drug is beta-blockers. 05:26 So we wanna beta-block these patients quite aggressively. 05:29 This is one of the few situations in medicine where you wanna lower the blood pressure down to normal regardless of where your patient started. 05:38 Typically, when patients come in with really elevated blood pressures, they have systolics of 180 or 200 or 220, we only lower them modestly. 05:46 We only lower them to maybe 20% of their original mean arterial pressure. 05:51 However, with aortic dissection, we wanna normalize that pressure as quickly as we can with the goal of preventing complications of the dissection. 06:01 So this is gonna take down our heart rate, it's gonna decrease myocardial contractility and ultimately lower aortic pressure and shear stress. 06:10 So whenever we treat dissections, or really any other life-threatening pathology, it's always a good idea to use an agent that can be given as a continuous infusion. 06:22 That way you can turn it up, turn it down, turn it off if you need to. 06:25 You can continually adjust how you're manipulating the patient’s physiology in order to achieve your treatment goals. 06:34 So typically we use Esmolol, which is a very short acting beta-blocker that's given as a continuous infusion. 06:40 Labetalol can also be used in some settings as well. 06:43 All right. 06:44 So once we've maxed out our beta blockade, if we're still not getting a good handle on the blood pressure, we wanna add an additional agent. 06:52 Nitroprusside used to really be the agent of choice, but now we often use ACE inhibitors or calcium channel-blockers. 06:59 There's no one agent that’s been shown to yield better outcomes than any others. 07:04 A lot of people will use an Enalaprilat or nicardipine as alternatives to nitroprusside to get the blood pressure under control if beta blockade alone isn't doing it. 07:14 Again, we wanna give these drugs as continuous IV infusions, we don’t wanna be giving boluses that we can't control the effect of in an hour. 07:23 We wanna make sure that we can really carefully adjust the patient’s parameters as needed. 07:28 If our patients become hypotensive, of course we're gonna turn off any infusions that we're giving that would be lowering the blood pressure but we're gonna also replete volume. 07:37 So we wanna make sure they have adequate circulating volume by giving them fluid first, and we're only gonna use vasopressors if we're certain that our patient is euvolemic and we've addressed any hypovolemia or bleeding.
About the Lecture
The lecture Aortic Dissection: Surgery & Medication by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock.
Included Quiz Questions
Which statement regarding the management of aortic dissection is INCORRECT?
- Aortic dissection is not always an emergency.
- Definitive treatment is based on its classification.
- Type A requires emergent surgical intervention.
- Type B is usually managed medically.
- Initial medical management is identical for both Type A and Type B aortic dissections.
Which of the following findings is NOT an indication for immediate surgery in Type B aortic dissections?
- Stable intramural hematoma
- Rupture or impending rupture
- Propagation of dissection
- Rapid expansion of aneurysm
- Renal ischemia
Which of the following is the agent of choice for the medical management of aortic dissection?
- Beta-blockers
- Calcium channel blockers
- Angiotensin-converting-enzyme inhibitors
- Angiotensin receptor blockers
- Nitroprusside
If the patient with aortic dissection is noted to have hypotension, which of the following actions should be done first?
- Ensure adequate intravascular volume with fluid/blood.
- Initiate vasopressors immediately.
- Initiate CPR.
- Continue IV infusion of beta-blockers.
- Refer for surgery immediately.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |