Playlist
Show Playlist
Hide Playlist
Aortic Dissection: History & Classic Findings
-
Emergency Medicine Aortic Dissection.pdf
-
Download Lecture Overview
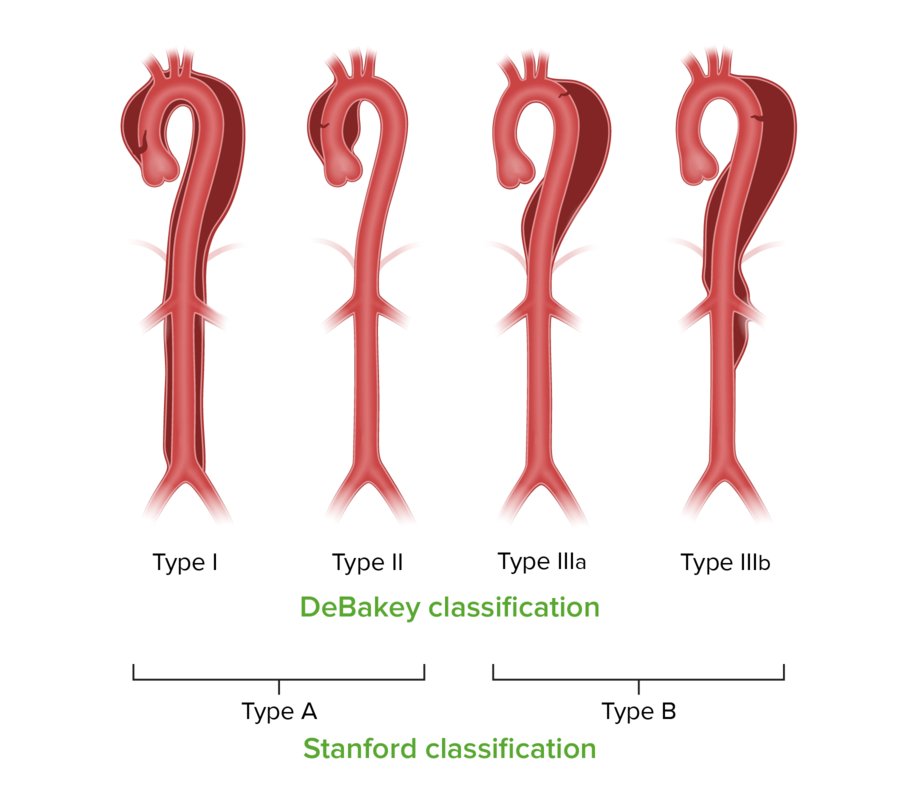
00:01 When we take a history of a patient with aortic dissection we wanna look for features that are gonna allow us to either include or exclude the disease in our differential diagnosis and probably the single most important question to ask is, how bad is the pain? Dissections are very, very painful, and a handful of cases I've seen throughout my career the patients have been in significant distress, often very agitated, clutching their chest, moaning, raving, it's not subtle pain. 00:31 So you wanna get a sense of how severe the pain is and how much distress the patient is in. 00:37 And when their distress level is really high, think about dissection. 00:40 Dissection is also a sudden catastrophic event. 00:44 You're going about your business doing everything normally and then suddenly you're intimal tears and you develop this accumulation of blood in the aortic wall. 00:53 This isn't something that gradually runs up, getting worse over time. 00:57 This is a sudden event and patients will report that they experienced pain very abruptly and that the pain was maximal at onset, it didn't sort of ramp up gradually over time, it really just hit them like a ton of bricks all at once. 01:12 The location of the pain is variable. 01:14 Now classically we all learned that it starts in the anterior chest and radiates into the back. 01:19 About two-thirds of patients will report the anterior chest pain, another third of patients will report back pain. 01:26 Meaning that two-thirds will not report that classic radiation into the back, so we don't wanna exclude the diagnosis just because they don't have that finding. 01:35 Another thing to think about is that almost a quarter of patients will present with isolated abdominal pain. 01:40 Remember the aortic goes all the way through the chest and abdomen, so you can have aortic dissection with pain only in the abdomen. 01:49 That classic ripping or tearing pain that we all learned about in medical school, you definitely see it. 01:56 It's present in nearly half of patients, but that means that another half of patients or even 60% would not have it. 02:03 So it's not a very sensitive finding but it is quite specific. 02:06 When patients tell you spontaneously, I feel like something is being ripped apart on the inside of my body, that's highly suggestive of an aortic dissection and should definitely get your attention. 02:18 We all learn about the classic physical exam findings in aortic dissection and unfortunately, these classic findings, while they make a lot of sense physiologically, and they're really cool when you see them, they are actually not the norm. 02:31 So pulse deficits where you feel a pulse more strongly on one side than another, or you kinda get a higher blood pressure in one arm compared to another, only present in about a third of the patients, meaning two-thirds of patients are not gonna have that finding. 02:46 Again, it's quite specific when they do have it, so if you find a patient who has diminish pulse or blood pressure differential across their arms, definitely think about dissection, but don't rule it out just because that finding is missing. 02:59 Neurologic deficits are only gonna be present when the dissection involves the carotid or brachiocephalic vessels, so we only see that in about 17% of cases. 03:10 Again, very specific when it's there but shouldn't cause you to exclude the diagnosis when it's not. 03:16 Diastolic murmurs are a classic. 03:20 We only see that in about a quarter of patients. 03:22 Syncope we see in only 13% of patients. 03:26 And hypertension which is a very important predisposing factor we see in about 50% of patients. 03:33 Meaning the other 50% can be normo or even hypotensive. 03:37 So you really should consider the diagnosis regardless of the patient's blood pressure. 03:41 We all learn about chest x-ray in the diagnosis of aortic dissection, right? And we all know about the classic finding of the wide mediastinum. 03:49 So rather than seeing a nice, crisp, narrow aortic silhouette, we see the upper mediastinum as sort of ballooned out taking up more space in the chest than it should. 03:59 That's great, unfortunately, it's not present universally. 04:03 You can also see obliteration of the aortic knob which is seen in this image, instead of a nice, crisp, clear circle delineating the aortic knob, you can see that the whole thing is kind of hazy and fuzzy and doesn't really give you clear definition of the anatomy. 04:19 Double aortic contour is also something that you can see on the chest x-ray that's where in addition to the aortic knob, you see a second bulge in the aorta representing the aneurysmal dilation. 04:32 And you can also in some cases, if the patient has a calcified aorta from atherosclerotic disease you can see those calcific plaques sort of floating in the middle of the aorta rather than adherent to the aortic walls like they should be. 04:46 So these are all classic findings. 04:48 However, chest x-rays are only about 70 to 80% sensitive for aortic dissection, meaning that a full quarter of your patients are gonna have normal or nondiagnostic chest x-rays, so you should never exclude the diagnosis based on x-ray findings. 05:04 All right. So if we can't rule it out based on our history and physical and our x-rays, what tests do we need to do? CTA or Computed Tomography Angiography is the most common test that's used in the emergency setting. 05:18 The sensitivity and specificity and some series have been reported as high as a 100%. 05:22 It's a very good way to image the aorta. 05:25 It's quick, it's available in almost every emergency department, at least in the US. And it's non-invasive. 05:31 However, it does require IV contrast which is problematic for patients who have contrast allergies, or for patients who have renal disease and can't receive contrast for those reasons. 05:44 It's also problematic for pregnant patients because it involves exposure to radiation. 05:48 So we do have alternatives. Transesophageal echo or MRI can be used. 05:54 They both have pretty good sensitivity and specificity and they both avoid the issue of contrast and radiation, however, the availability is limited. 06:03 They take a long time and they're really not considered first line test. 06:08 So when it all possible, get a CTA to image the aorta if you suspect this pathology. 06:14 Here's an example of a CTA, and you can see up at the top of the image the aorta in transverse section. 06:22 And there is both a true lumen which is filled with bright, white contrast-enhanced blood, as well as a false lumen which is a little bit grayer and darker because that represents hematoma in a region where contrast isn't reaching the blood. 06:38 When we think about aortic dissection it's really important that we classify the location of the dissection because that's gonna affect our management. 06:49 So there are two different classification schemes for dissection, the Stanford and the De Bakey. 06:54 In the Stanford classification, dissections are broken down into A and B. 06:58 Basically, A is any involvement of the ascending aorta, whereas B, involves the descending aorta. 07:05 So pretty straight forward. A for ascending. Easy to remember. 07:08 The De Bakey classification is a little bit more extensive. 07:12 A Type I De Bakey, is gonna involve the entire aorta both ascending and descending. 07:17 A Type II De Bakey is gonna involve only the ascending. 07:21 And a Type III is gonna involve only the descending. 07:24 De Bakey Type III is further sub-classified into thoracic versus abdominal. 07:29 So thoracic is a III-A and abdominal is a III-B. 07:33 It's not so much important that you memorize these specific classification schemes as it is that you recognize that the anatomic location of aortic dissection is really, really important because that's gonna determine your management and it's also gonna help you predict what complications the patient might experience based on what vessels are gonna be involved.
About the Lecture
The lecture Aortic Dissection: History & Classic Findings by Julianna Jung, MD, FACEP is from the course Cardiovascular Emergencies and Shock. It contains the following chapters:
- History
- History
- Additional Test
Included Quiz Questions
Which of the following statements about the physical findings in aortic dissection is NOT correct?
- It is caused by a tear in the tunica externa.
- Syncope is present in a minority of patients.
- Peripheral pulses may be symmetric in some patients.
- Diastolic murmurs can be found in almost one-third of patients.
- Hypertension is present in 50% of patients.
Which of the following findings on chest X-ray is least associated with aortic dissection?
- Pleural thickening
- Inward displacement of calcification
- Double aortic contour
- Obliteration of the aortic knob
- Widened mediastinum
When looking for aortic dissection, which highly specific and sensitive modality is recommended for hemodynamically stable patients who require RAPID imaging and do not have any contraindications to contrast?
- Computed tomography angiography
- Chest radiograph
- Trans-esophageal echocardiography
- Magnetic resonance angiography
- 2D-echocardiography
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |