Playlist
Show Playlist
Hide Playlist
Dysfunctional Uterine Bleeding (DUB) in Adolescent Girls
-
Slides DUB Pediatrics.pdf
-
Download Lecture Overview
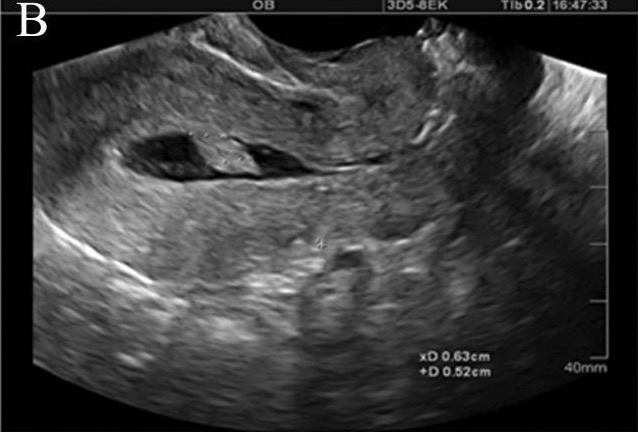
00:00 In this lecture, we will discuss dysfunctional uterine bleeding in adolescent girls. 00:07 There is the 7, 7, 21 rule to decide quickly whether this patient is having a normal or an abnormal menstrual cycle. 00:16 Generally, girls should have less than 7 pads per day for less than 7 days. 00:22 They should have 21 days or more between periods. 00:25 So the duration of the menstrual cycle should be at least 21 days. 00:30 The duration of the bleeding should be three to seven days. The average blood loss is 30-40 ml or less than 7 pads. 00:39 Dysfunctional uterine bleeding then is abnormal changes in the frequency, the duration of flow, or the amount of blood loss that’s occurring in periods. So, we have different terms to describe different problems. Menorrhagia is a prolonged or heavy uterine bleeding at regular intervals. Metrorrhagia is uterine bleeding that occurs at irregular intervals. 01:04 So, menometrorrhagia is prolonged or heavy bleeding that occurs at irregular intervals. 01:11 Oligomenorrhea is uterine bleeding that happens in intervals more than 35 days. In other words, it’s less common. Let’s discuss briefly the pathophysiology of dysfunctional uterine bleeding. 01:24 Girls may have an immaturity of their hypothalamic-pituitary-ovarian axis. This can result in anovulatory cycles. This is normal in the first two years after menarche. Girls tend to have very irregular periods after their first period. However, when we see dysfunctional uterine bleeding, this can be a result of many things. This can be a result of failure to ovulate, an absence of the corpus luteum, no progesterone secretion or unopposed estrogen, excessive proliferation of the endometrium, no cyclical hormone withdrawal, and then results in irregular, heavy bleeding. 02:05 So, when we see a patient with DUB, we want to take a good history. In particular, we will want to ask about the age of menarche, what sort of pattern of bleeding they’re having. Is it menorrhagia or menometrorrhagia, whether they have cramping or pain? We need to ask about a history of trauma and whether they’re having sex and whether they’re using contraception. We also have to ask these patients if they’re on any medications that might affect hemostasis of the HPO axis. 02:36 We need to ask about associated symptoms to get at severity of bleeding. Are they anemic? Do they have dizziness or fatigue? Finally, it’s useful to ask if there’s a family history of bleeding disorders or other gynecologic problems that might be participating in this patient’s condition. 02:53 Then, we need to do a good physical exam. This includes looking at vital signs for hemodynamic instability from anemia, checking for pallor or other signs of anemia, and doing a Tanner stage to make sure their sexual maturity rating is appropriate. Also, we should look for signs of androgen excess such as hirsutism or acne. Also, we should check for goiter because abnormal thyroid function can partake and result in dysfunctional uterine bleeding. We should do a breast exam for evidence of galactorrhea or tenderness which might tip us off that there’s a fundamental hormone problem. We should check for evidence of bleeding disorders such as easy bruising. 03:37 We should do a pelvic exam to really get a sense of what’s going on if there’s any internal pathology. 03:44 Lastly, we will often do diagnostic testing in these patients. Some key diagnostic tests: One is the pregnancy test. We might do a CBC to look for anemia and check of PT, PTT if we’re concerned that the patient is bleeding too much. Likewise, we can also check for sexually transmitted infections as they may result in dysfunctional uterine bleeding. 04:09 Lastly, if we suspect a hormonal problem, we will check hormone studies. We’ll check thyroid. 04:15 We'll check prolactin. Generally, we can check androgens and LH and FSH to get a sense of that axis and how it’s functioning. Next, we may undergo some radiologic imaging and in particular, we may do an ultrasound of the pelvis. This is certainly true if we suspect the patient has a high hCG level. 04:35 We might need to rule out an ectopic pregnancy. Likewise, if a patient has a structural abnormality of the uterus or the GU tract, an ultrasound is helpful in making that diagnosis and figuring out next steps. 04:49 So, how do we treat central causes of dysfunctional uterine bleeding? This is the most common problem. 04:56 Usually, what we’ll do is provide patients hormonal control. The best way to start is a low dose estrogen oral contraceptive pill. These have fewer side effects than the higher dose estrogens which can cause quite a bit of nausea. Also, it’s important that we always counsel patients who are getting oral contraceptive pills that oral contraceptives are not preventative of sexually transmitted diseases and patients should use condoms in addition to their oral contraceptive pill. 05:26 So, that’s my review of dysfunctional uterine bleeding in girls. Thanks for your time.
About the Lecture
The lecture Dysfunctional Uterine Bleeding (DUB) in Adolescent Girls by Brian Alverson, MD is from the course Adolescent Medicine. It contains the following chapters:
- Dysfunctional Uterine Bleeding
- Physical Exam Findings
Included Quiz Questions
Which of the following refers to prolonged, irregular, and more frequent menstrual bleeding?
- Menometrorrhagia
- Menorrhagia
- Metrorrhagia
- Oligomenorrhea
- Polymenorrhea
Which of the following is true regarding the normal menstrual cycle in girls?
- Bleeding for < 7 days per cycle
- Use of 3-10 pads per day
- Less than 21 days between periods
- Cycle length is 28 to 40 days
- Average blood loss per cycle is > 70 ml
What is the term used to describe prolonged or heavy bleeding that occurs at regular intervals?
- Menorrhagia
- Metrorrhagia
- Menometrorrhagia
- Polymenorrhea
- Oligomenorrhea
Which of the following is NOT considered a cause of irregular menstrual cycles during the initial years after menarche?
- Excessive progesterone secretion
- Failure to ovulate
- Absence of the corpus luteum
- Unopposed estrogen secretion
- Excessive proliferation of the endometrium
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent and clear overview of the terms and pathophysiology. Thank you!