Playlist
Show Playlist
Hide Playlist
Type 1 Diabetes Management with Case
-
Slides 02-03 Diabetes Mellitus part 1.pdf
-
Download Lecture Overview
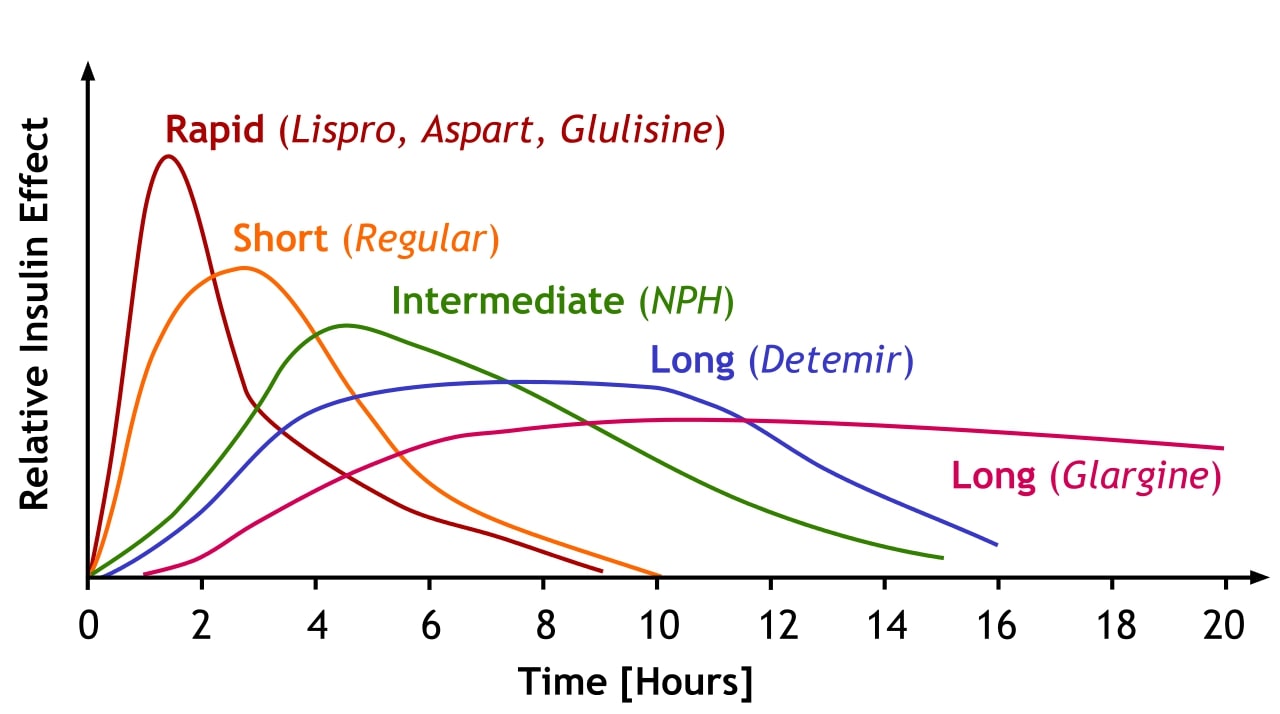
00:00 Therapy for type 1 diabetes. Usually these patients are looking at life-long insulin therapy as the first line treatment. Physiologic insulin therapy also known as intensive insulin therapy is the ideal insulin regimen as it attempts to mimic the body's actions of normal pancreatic beta cells. Let's go on to another case. Here we have a 14-year-old boy who is rushed to the emergency room after became disoriented at home. His parents say that the boy was doing well until 2 days ago when he got sick and vomited several times. They thought he was recovering but today he appeared to be disoriented since the morning. His vital signs are normal except for shallow rapid breathing at a rate of 33 breadths/minute. His blood sugar level is 654 mg/dL and his urine is positive for ketones. He is diagnosed with diabetic ketoacidosis and is managed with intravenous fluids and insulin. He responds well to therapy. His parents are told that their son has type 1 diabetes and insulin therapy options are being discussed. Which types of insulin can be used in this patient for the rapid action required during meal times as well as for his basal needs. This is a teenage boy, type 1 diabetes is more likely and we have confirmed the diagnosis. He has also presented with classic features of diabetic ketoacidosis initially with vomiting associated with dehydration. 01:35 He may have had a preceding infection that was subclinical, and he has presented with respiratory alkalosis in the form of tachypnea in response to developing a metabolic acidosis from diabetic ketoacidosis. Very high blood glucose and urine positive for ketones help steer you towards this diagnosis. This patient's presentation with type 2 diabetes with DKA is not an uncommon initial presentation and it is usually at this point during the phases prior to discharge from the hospital that discussion of long term regimens to control the diabetes are discussed. A preprandial insulin lispro and a basal insulin glargine would be ideal. This provides the combination of a long-acting basal insulin that can be taken in the morning and evening with shorter-acting rapid onset insulin at pre-meal time. Let's talk a little bit about the various types of insulin preparations. Rapid acting insulin examples include glycine, insulin lispro, and insulin aspart begin to work within 15 minutes of injection and continues to work for 2-4 hours. Regular or short-acting insulin usually begins to work within 30 minutes. The peak effect is at 2-3 hours and it continues to work after injection for a range of 3-6 hours. Intermediate acting insulin otherwise known as NPH or neutral protamine hagedorn begins to work after injection within 2-4 hours. Its peak effect is reached at 4-12 and continues to work after injection in the range of 12-18 hours. And then finally long acting insulin such as insulin detemir or insulin glargine used in this case usually begins to work within several hours of injection and then continues to be present over a 24-hour period before disappearing from the body. This slide demonstrates the peak effect and duration of action of the various insulin preparations that are color coated ranging from rapid or lispro insulin with the earliest peak and the shortest duration all the way through to glargine insulin which has the latest peak and the longest duration. Intensive insulin therapy consists of multiple daily injections usually more than 3 per day with intermediate or long acting insulin for basal coverage and multiple preprandial injections throughout the day with analog or regular insulin. It can also include continuous subcutaneous infusions and mealtime dosing with an insulin pump. They just support targeting normal glycemic levels and a goal hemoglobin A1c of less than 7% to reduce the long-term complications of diabetes. Long-term reductions in early microvascular disease of 34-76% can be expected and also reductions in cardiovascular events in the range of 42-57%. 04:52 Risks, however, of very very tight intensive insulin therapy are more frequent episodes of hypoglycemia and with the use of insulin unfortunately weight gain. Initial total daily doses of insulin typically range from 0.3 to 1 unit/kg/day. The basal dose is usually half of the daily calculative dose of insulin. This is provided by 1 or 2 daily injections of longer duration insulin lasting from 10-24 hours either with detemir, glargine, or NPH. Insulin pumps can also provide basal coverage with analog insulin. The bolus dose provides the remaining doses of insulin required during the day and are there to cover the number of meals consumed during the day. Analog or regular insulin injected pre meal is usually the way to manage this and it's usually based on counting the number of carbohydrates in a particular meal. Analog insulin bolused with a pump prior to meal times is a slightly simpler way of performing the same action. Insulin dosing immediately after meal is appropriate in certain situations particularly when food intake is unpredictable. 06:07 Postprandial insulin dosing allows for a reduction in the insulin dose that is commensurate with the amount of food ingested to avoid hypoglycemia that could have resulted from the insulin dose. 06:19 Postprandial insulin dose is reduced by half if only half of the meal is consumed.
About the Lecture
The lecture Type 1 Diabetes Management with Case by Michael Lazarus, MD is from the course Diabetes Mellitus. It contains the following chapters:
- Type 1 DM Treatment
- Case: 14-year-old Boy with Disorientation
- Various Types of Insulin
- Intensive Insulin Therapy
- Principles of Insulin Therapy
Included Quiz Questions
What is the underlying mechanism of the following patient's presenting illness? A 14-year-old boy is rushed to the emergency department after becoming disoriented at home. His parents say that 2 days ago he got sick and vomited several times. He was recovering but today appeared to be disoriented since the morning. Physical examination: Normal vital signs except for shallow rapid breathing (33 beats/min) Laboratory test results: blood sugar level is 654 mg/dL, and urine is positive for ketones. Diabetic ketoacidosis is diagnosed, and he is treated with fluids and insulin. He responds well to the therapy. Type 1 DM is diagnosed, and insulin therapy options are being discussed.
- Loss of endogenous insulin production by the pancreas
- Excessive endogenous insulin production by the pancreas
- Relative insulin resistance from chronically elevated insulin levels
- Excessive ketone production from an inborn error of metabolism
- Excessive exogenous insulin administration
Which of the following types of insulin is most appropriate to give before each meal?
- Lispro
- NPH
- Glargine
- Detemir
- Regular insulin
You are initiating insulin therapy for a 25-kg patient with newly diagnosed type 1 diabetes. Which of the following is the best starting regimen?
- 10 units glargine once daily and 3 units lispro 3 times daily before meals
- 15 units glargine once daily and 15 unit lispro 3 times daily before meals
- 15 units lispro once daily and 3 units glargine 3 times daily before meals
- 8 units NPH 3 times daily before meals and 8 units glargine once daily
- 15 units lispro 3 times daily before meals
Which types of insulin can be used for the patient described below? A 14-year-old boy is rushed to the emergency department after becoming disoriented at home. His parents say that 2 days ago he got sick and vomited several times. He was recovering but today appeared to be disoriented since the morning. Physical examination: Normal vital signs except for shallow rapid breathing (33 breaths/min). Laboratory test results: Blood sugar level is 654 mg/dL, and urine is positive for ketones. Diabetic ketoacidosis is diagnosed, and he is treated with fluids and insulin. He responds well to the therapy. Type 1 DM is diagnosed, and insulin therapy options are being discussed.
- Preprandial insulin (e.g. lispro, aspart, and glulisine) and basal insulin (e.g. glargine or detemir)
- Only a preprandial bolus cover with short-acting insulin is required.
- Preprandial insulin (e.g., glargine and glulisine) and basal insulin (e.g., regular insulin)
- Only a basal cover with long-lasting insulin is required.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |