Playlist
Show Playlist
Hide Playlist
Vascular Changes during Acute Inflammation
-
Slides Acute and Chronic Inflammation Vascular changes.pdf
-
Download Lecture Overview
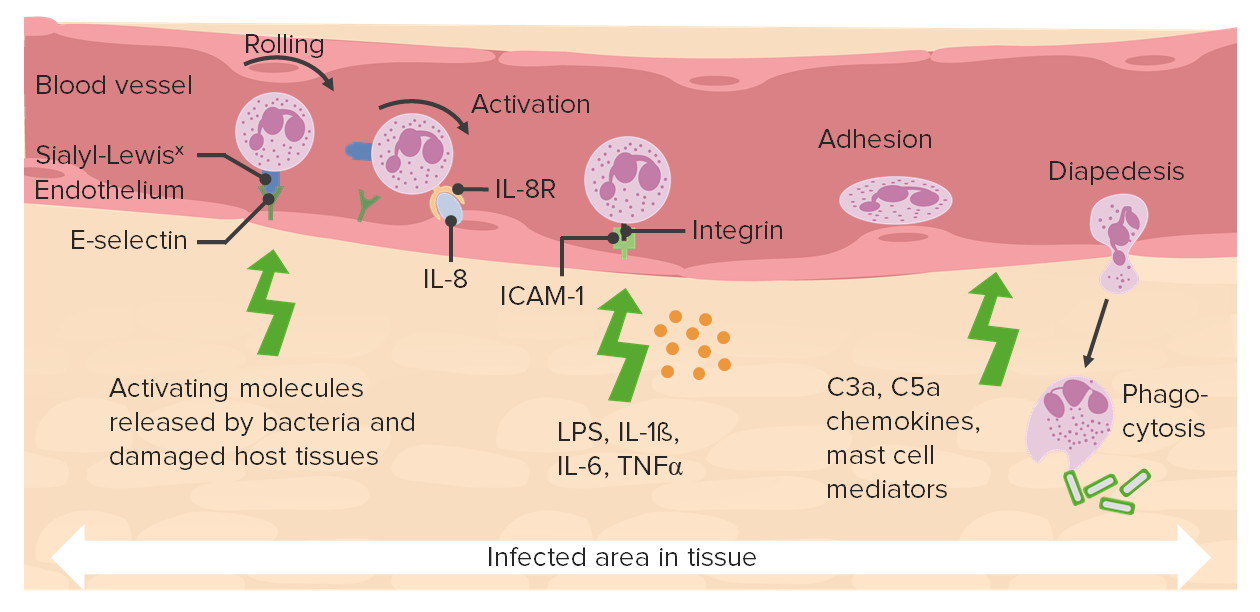
00:01 Increase Vascular Permeability. 00:03 So that's just increased flow and we're getting increased movement of water across the cells just because of hydrostatic pressure. 00:10 But we're also changing how the endothelial cells are behaving. 00:15 And very quickly, after an initial inflammatory injury, or injury that's going to activate an inflammatory pathway, we have a transient and reversible contraction of endothelial cells. 00:28 The cytoskeleton pulls them apart. 00:32 That's driven by histamine released by the mast cells, bradykinin, and we'll talk more about that that's inflammatory mediator made by a variety of cells. 00:40 And leukotrienes, one of those eicosanoids. 00:42 So endothelial cell contraction happens very quickly. 00:47 Endothelial cell retraction because of breakdown of the tight junctions between the endothelial cells also happens. 00:53 It's more of a passive process, it takes many hours, and it's very reversible. 00:57 In fact, you've all experienced this, if you've ever had a sunburn, that late in the day after you've had that wonderful glorious day on the beach, and you've got that nice rosy red sunburn in your skin. 01:09 And at night, you feel like your skin's a little tight, and you feel a little warm. 01:13 Well, in fact, that is being driven by cytokines. 01:18 Interleukin-1, tumor necrosis factor other inflammatory cytokines that are causing the endothelial cells to pull ever so slightly apart. 01:27 And now you're getting a transudation of fluid water, making the skin feel a little bit tight. 01:33 You're also get increased vascular flow, and that's why you feel red and warm. 01:37 So just another little pathologic take home nugget. 01:40 You can also get increased permeability by injury to the endothelium. 01:45 And it can be early direct necrosis due to a toxin, or due to trauma, or due to ischemia. 01:52 It can also be late due to apoptosis driven by a variety of inflammatory pathways. 01:57 So you can get leakage increased vascular permeability, because the endothelial cells are hurt. 02:02 That makes sense. 02:03 You can also get it because leukocytes mediate damage. 02:07 So there are multiple, multiple ways that you can get increased vascular permeability in inflammatory area. 02:15 So we talked about increased flow, that's going to get rubor and calor. 02:19 And that increased flow will also have a degree of the tumor, the edema, but now with increased permeability, due to all these mechanisms that we just talked about, you have increased much more increased edema fluid, water, electrolytes, and mediators they are able to get into the extravascular space. 02:37 Okay, now it's important and this becomes clinically relevant. 02:41 Not all vascular leakiness increased permeability is created equal. 02:47 So at the top, we see here, hydrostatic pressure, oncotic pressure being balanced, in terms of moving fluid into or out of a vessel. 02:58 We can change the hydrostatic pressure be by causing dilation of an arteriole. 03:05 We can also have it because we block the outflow in a venous circulation. 03:11 If we block the venous outflow, all that pressure backs up through the capillary and into the other end, and we will have increased efflux of water. 03:20 Congestive heart failure will also do this by giving us kind of retrograde pressure increases. 03:25 So we can increase hydrostatic pressure. 03:27 In fact, the swollen ankles associated with heart failure is because of increased hydrostatic pressure due to kind of retrograde increases. 03:39 You can also get this loss of fluid into the extravascular space by changing the oncotic pressure. 03:46 So if we decreased protein synthesis, the liver is damaged. 03:50 So we're not making enough albumin, or we have increased protein loss such as glomerulonephritis, where we have a lot of protein in the urine. 03:59 Then our oncotic pressure goes down and we get that same increased amount of fluid, electrolyte water into the extravascular space. 04:09 So that's one way to do it. 04:11 The other way is with inflammation. 04:13 Inflammation is kind of getting the same effects, but now on steroids. 04:19 It is much more robust. 04:22 And you get increased endothelial permeability from all the things that we talked about in previous slides. 04:27 You see endothelial damage, and you see massive vasodilation and stasis because we're losing fluid. 04:34 And so inflammation gives us a much greater degree of fluid that gets out of the tissue or out of the bloodstream into the tissue. 04:45 This has ramifications in terms of fluid accumulations. 04:48 So when we have increased hydrostatic pressure, or diminished oncotic pressure, the fluid tends to come out is protein poor. 04:57 It's basically an ultra filtrate and it is mostly water, and a little bit of electrolyte, a little tiny bit of protein, but it's really protein poor. 05:06 It's called a transudate. 05:07 And when we see it grossly, it looks yellow. 05:10 It looks yellow and clear, it's serous. 05:13 That's what the serous means. 05:15 On the other hand, the inflammatory fluid that gets out is called an exudate. 05:21 And transudate and exudate is a very important distinguishing feature in the clinical setting, because if it's a transudate, that's one thing, if it's an exudate, it usually means there's an infection. 05:30 So in exudates are protein rich. 05:32 So there's some much increased vascular permeability, that we're getting all kinds of protein that's out there. 05:38 And we've even got cells. 05:39 We've got neutrophils, we got macrophages, we got all kinds of other stuff there. 05:42 It tends to look bloody because we've even had leakage of red blood cells. 05:46 And that's what's going on in the little diagram. 05:48 The red blood cells are even getting across. 05:50 So it looks bloody, hence sanguineous. 05:53 And it can look also pussy or purulent. 05:56 So exudates have a very different significance clinically than transudates. 06:01 And they're just about different levels of vascular leakiness. 06:06 So, we've covered the very first stage of acute inflammation. 06:11 We've talked about the vascular changes that are going to give us calor (heat), rubor (redness), and a tumor or edema. 06:19 And then we're going to move on to the cell recruitment and eventually the mediators.
About the Lecture
The lecture Vascular Changes during Acute Inflammation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Which of the following is true about endothelial cell retraction?
- It is caused by breaking down the intercellular tight junctions.
- It is one of the earliest vascular changes occurring in acute inflammation.
- It is driven by the release of histamine, bradykinin, and leukotrienes.
- It is an active process caused by the rearrangement of the cytoskeleton.
- It is an irreversible change.
How does inflammation force the fluids out of the vessels?
- Endothelial damage
- Venous outflow obstruction
- Decreased protein synthesis
- Vasoconstriction and stasis
- Increased oncotic pressure
Which of the following best describes a transudate?
- A protein-poor fluid
- A protein-rich fluid
- A cell-rich fluid
- Pus-like appearance
- Bloody appearance
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |