Playlist
Show Playlist
Hide Playlist
Pelvic Inflammatory Disease (PID): Management and Etiology
-
Slides PelvicInflammatoryDisease InfectiousDiseases.pdf
-
Download Lecture Overview
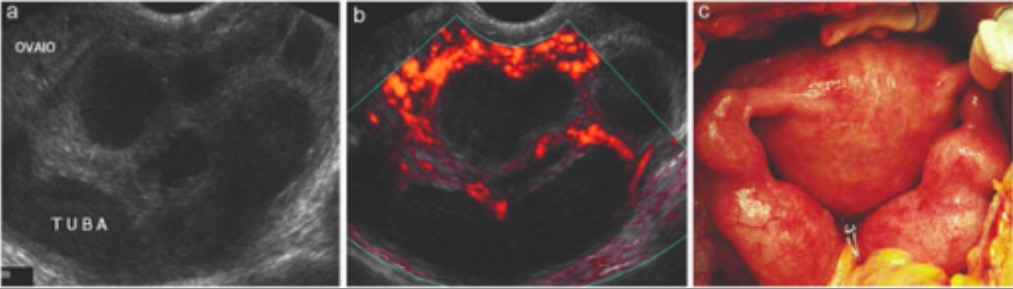
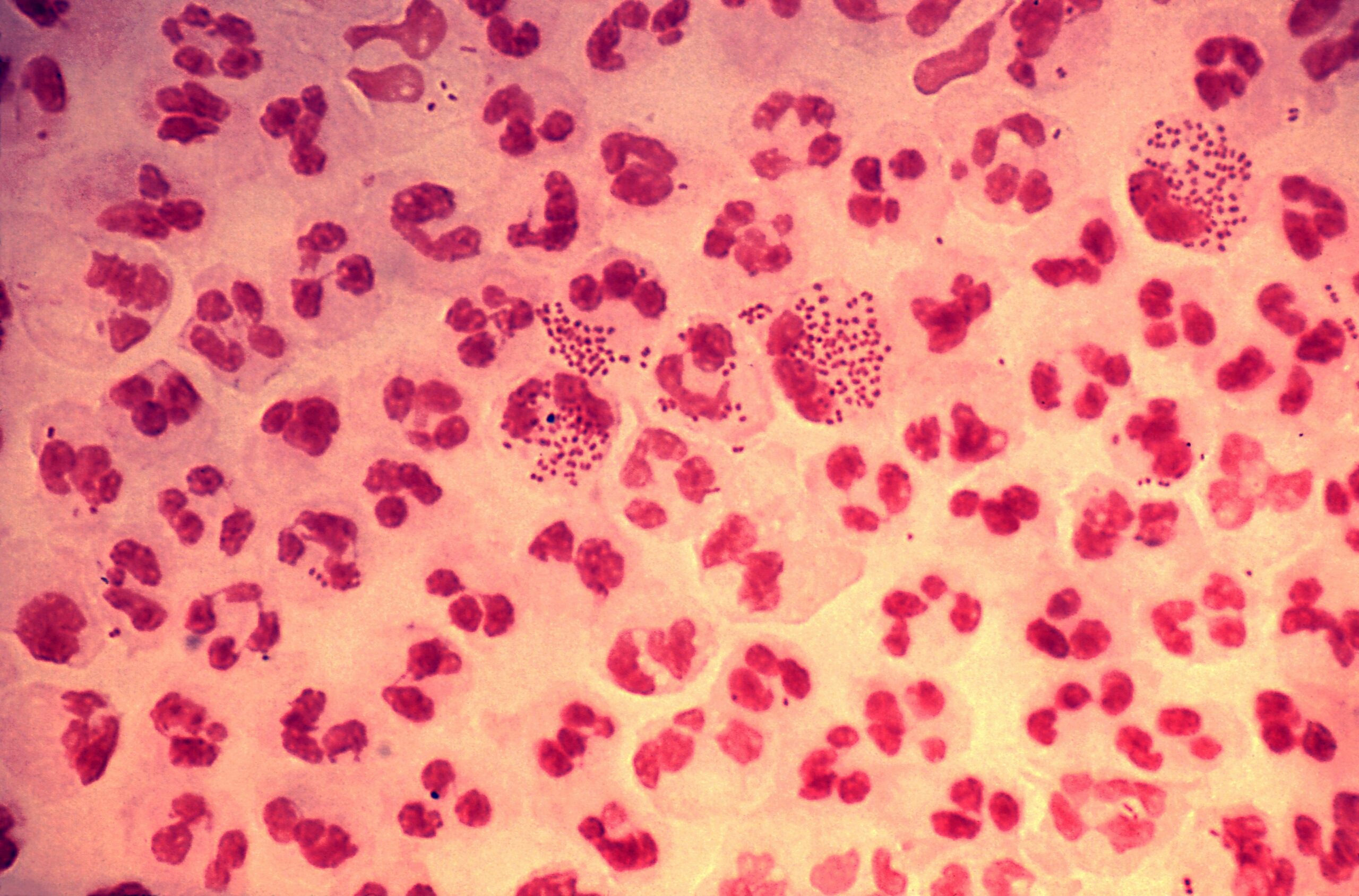
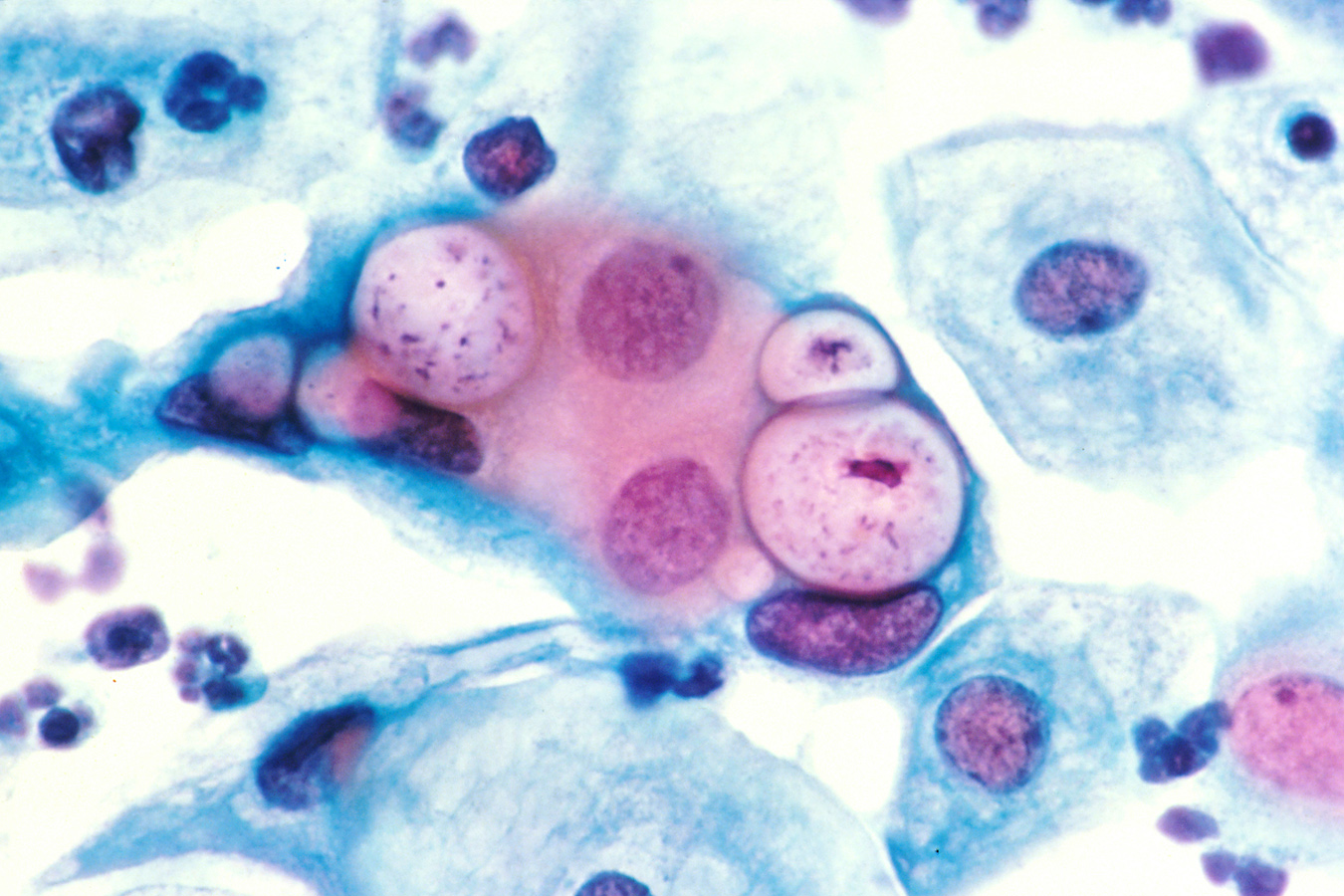
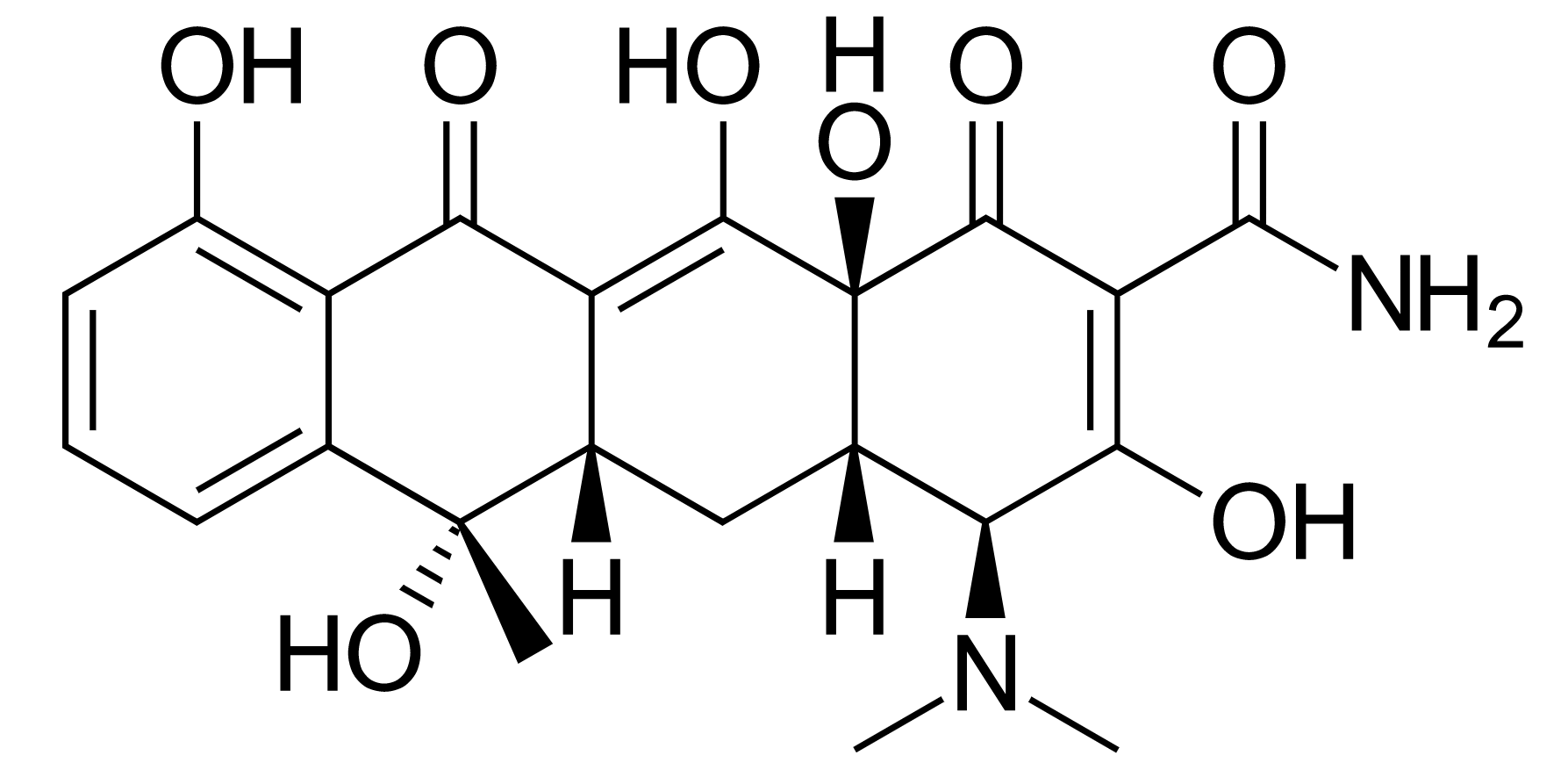
00:01 So then, how do we treat PID? Well, fortunately we have regimens to treat most patients as an outpatient. 00:12 We would hospitalize patients only for clinically severe disease (high fever, nausea, vomiting) or patients unable to tolerate or follow an outpatient oral regimen. 00:26 That includes a sizeable minority of individuals. 00:30 We would certainly, for the safety of mother and baby, hospitalize all pregnant women with PID. 00:39 One of the major concerns is, "Is there pus that needs to be drained - a tubo-ovarian abscess?" So they would need to be admitted because antibiotics will fail to resolve a big abscess. 00:57 The antibiotics don't penetrate well, and the abscess needs, as we say in medicine, fresh air and sunshine -- it needs drainage. 01:07 And then sometimes acute appendicitis is in the differential diagnosis. 01:12 And when a physician can't exclude appendicitis, it would be prudent to admit the patient. 01:19 Pelvic rest is another form of therapy. 01:24 It's very, very important to resolve this process and so in terms of treating patients with antibiotics, for outpatients, we use a combination of intramuscular and oral regimens. 01:37 And the classic regimen is that of ceftriaxone. 01:42 And as you remember, this is a treatment for gonorrhea. 01:45 We also add doxycycline twice a day for 14 days and this will cover our chlamydia and mycoplasma organisms if they're present. 01:57 We also add metronidazole. 01:59 Now, metronidazole, well, is a wonderful agent to treat anaerobic organisms which may be involves in this infection as I've mentioned. 02:09 And, also, it is a treatment for bacterial vaginosis that might be present. 02:16 Now for inpatients, we're going to be using essentially IV cefotetan every 12 hours or every six hours plus doxycycline every 12 hours. 02:31 Or clindamycin plus gentamicin which will cover the aerobic gram negative rods and the anaerobes. 02:39 So we would expect patients to improve within three days. 02:47 If there's no improvement after our outpatient intramuscular or oral therapy, we would then hospitalize and reassess our antibiotic regimen and consider diagnostic laparoscopy. 03:02 We would also repeat the test for Neisseria gonorrhea and Chlamydia trachomatis, and then three months after treatment, we would retest again. 03:15 So we would expect clinical improvement within three days. 03:19 Another important thing would be to counsel our patients about the problems and complications of pelvic inflammatory disease, and we would have to honestly tell the patients there is an increased incidents of ectopic pregnancy because of the scaring of the fallopian tubes and the adhesions that develops as parts of this process. 03:46 So in terms of preventing further episodes of PID we'd recommend that a person who's been exposed to a woman with PID during 60 days before the onset of symptoms should be tested for gonorrhea and Chlamydia. 04:04 Now for a woman whose last sexual intercourse was more than 60 days, we would recommend that we treat that most recent sex partner for both gonorrhea and Chlamydia empirically. 04:18 We would also recommend abstinence from sex until a therapy has been completed and the symptoms have resolved completely for both women and for her partner. 04:31 And this brings us to our conclusion of the discussion of pelvic inflammatory disease.
About the Lecture
The lecture Pelvic Inflammatory Disease (PID): Management and Etiology by John Fisher, MD is from the course Genital and Sexually Transmitted Infections. It contains the following chapters:
- Pelvic Inflammatory Disease – Management
- Pelvic Inflammatory Disease – Etiology
Included Quiz Questions
Which of the following patients with a diagnosis of pelvic inflammatory disease is the most appropriate candidate for outpatient therapy?
- A 25-year-old college student with abdominal pain, cervical motion tenderness, and a positive smear for gonorrhea
- A 32-year-old homeless woman with abdominal pain, fever, cervical motion tenderness, and mucopurulent cervicitis
- A 21-year-old sexually active woman with right lower abdominal pain, nausea, vomiting, and mild cervical motion tenderness
- A 27-year-old pregnant woman with lower abdominal pain
- An 18-year-old woman who has not improved after 72 hours of oral therapy
Which of the following antibiotic regimens is most appropriate for outpatient treatment of mild pelvic inflammatory disease without a prior history of gynecological instrumentation?
- A single intramuscular dose of ceftriaxone (500 mg) PLUS oral doxycycline (100mg) twice a day for 14 days PLUS oral metronidazole (500 mg) twice a day for 14 days
- A single dose of intramuscular ceftriaxone (250mg) AND single oral dose of azithromycin (1 g)
- Oral clindamycin (900mg) thrice a day AND oral metronidazole 500mg orally twice a day for 7 days
- A single dose of intramuscular ceftriaxone (250mg) AND oral metronidazole (250mg) thrice a day for 7 days
- Oral clindamycin (900mg) thrice a day AND a single oral dose of azithromycin (1 g)
Which of the following options provides the most appropriate treatment for a non-pregnant woman with sepsis and a large tubo-ovarian abscess?
- Hospitalization, intravenous antibiotic therapy, and surgical drainage
- Hospitalization and intravenous antibiotic therapy
- Outpatient treatment with oral antibiotics and follow-up within 3 days
- Outpatient treatment with oral antibiotics and follow-up the next day
- Hospitalization and surgical drainage
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |