Playlist
Show Playlist
Hide Playlist
Ischemic Heart Disease: Development
-
Slides IschemicHeartDisease CardiovascularPathology.pdf
-
Download Lecture Overview
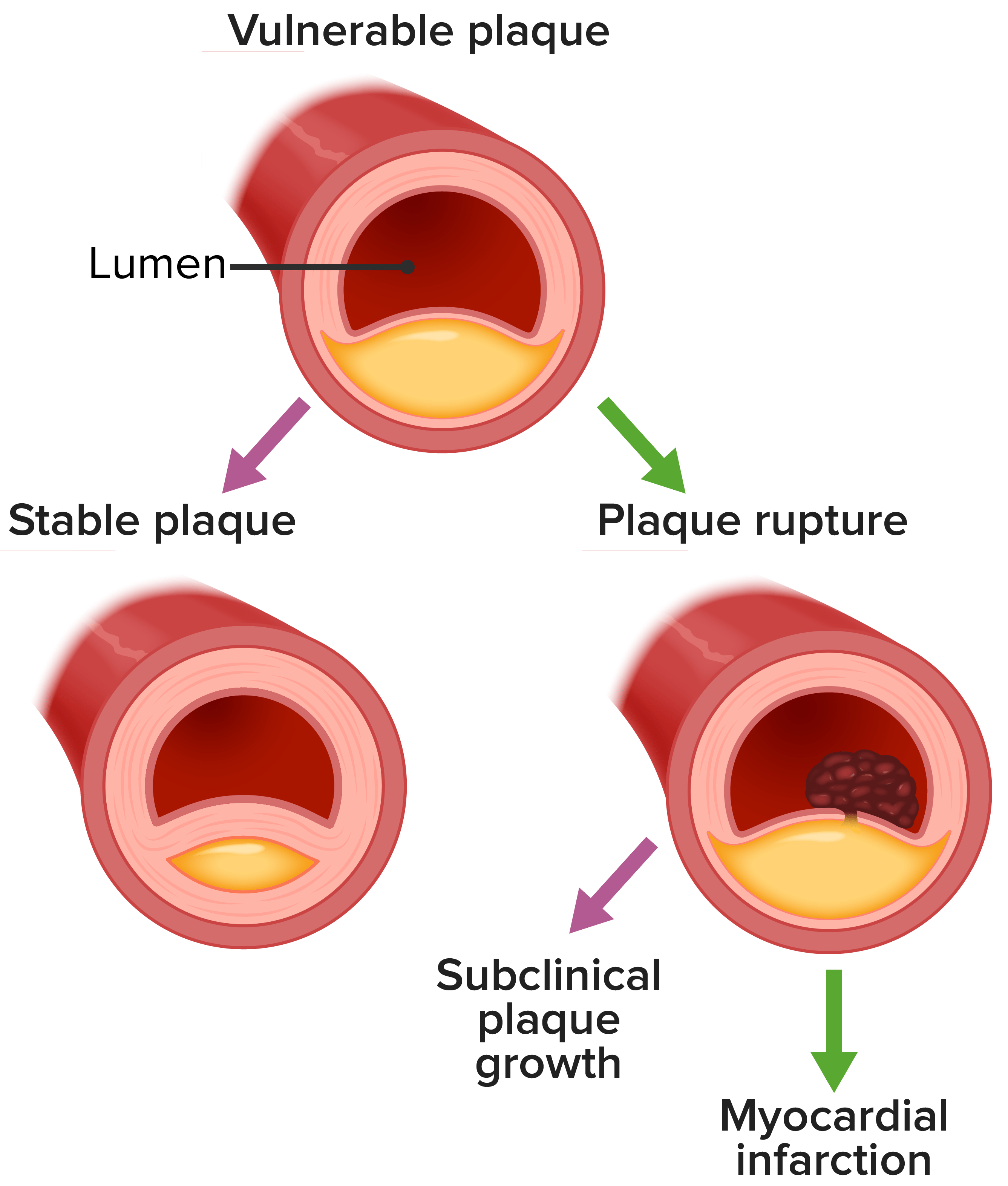
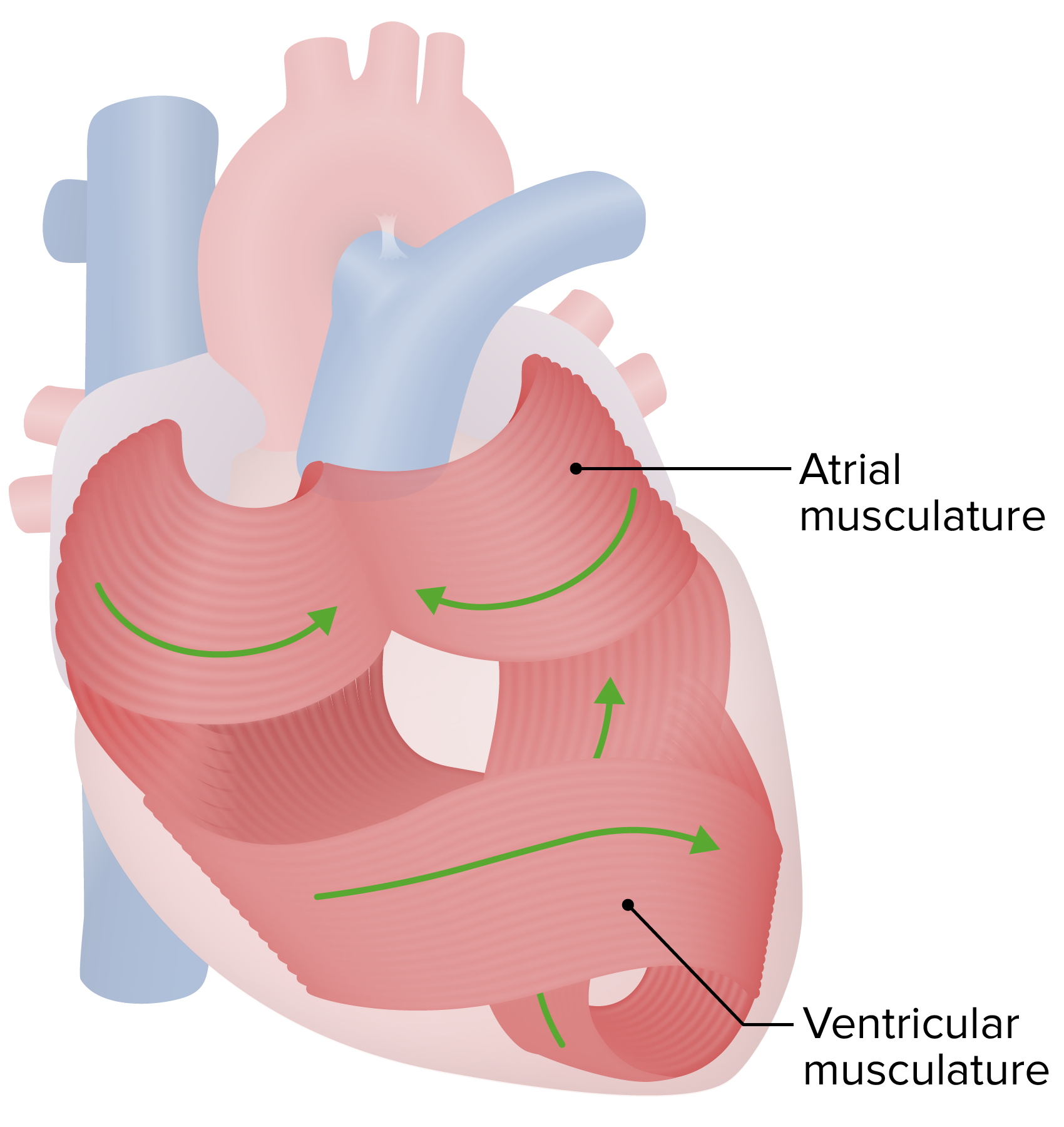
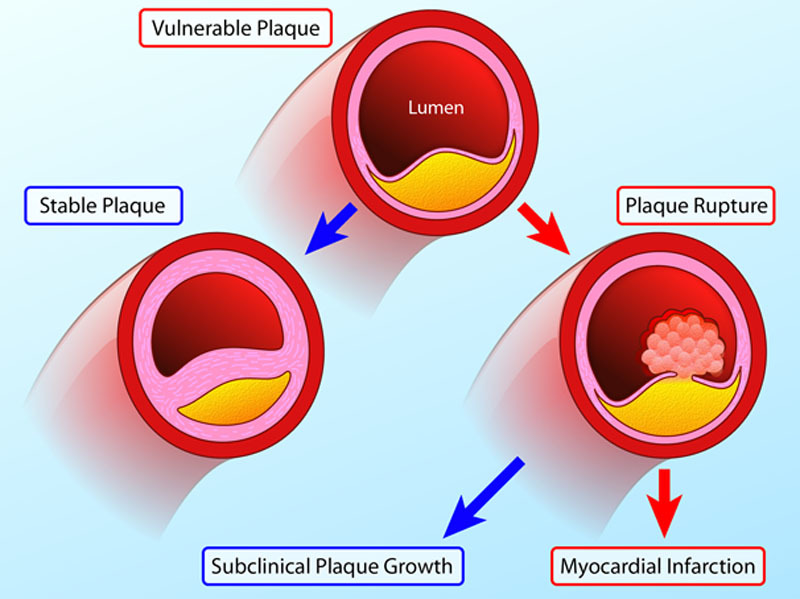
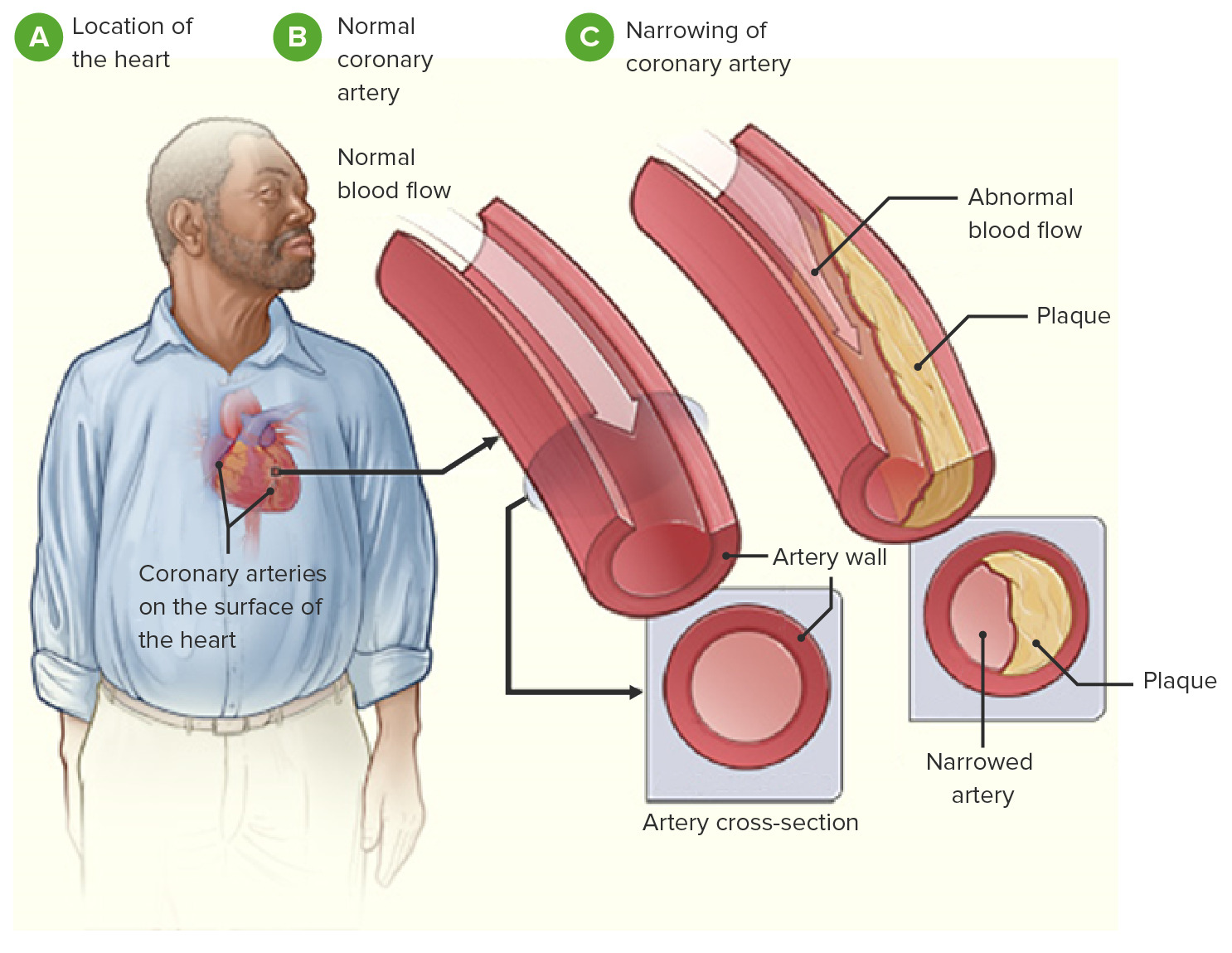
00:01 Ischemic heart disease. Important for us to take a look at the following table, quite. So the patient has now moved on from unstable angina. Unfortunately has now experience the myocardial infarction, an MI. How do you know that? Patient says I have chest pain, has tachycardia, diaphoresis. This chest pain is radiating where? Up into the left shoulder as maybe moving up into the jaw. Substernal chest pain, is it not right? Take a look at the cardiac enzymes, you find troponin I to be elevated. Why is that your gold standard because within 24 hours, it is elevated and how long does it last, troponin I? About one week. Keep it simple, okay. So therefore, it is quite difficult for you to miss your patient having a myocardial infarction with troponin I and you shall see that in a second. So now what are you doing here? The important points of changes in myocardial infarction. It is 0 to 24 hours gross changes like microscopy and then complications. 0 to 24 hours. Have occlusion of an artery, infarct. You have dark mottling, that's what you are looking at and pale with the area because it just underwent what? Necrosis. What kind please? From basic pathology, it is a coagulant necrosis. 01:18 What kind of infarct is this? A pale or hemorrhagic infarct. It is a pale infarct. Things that we have already referred to. So let us begin at the top. Coagulant necrosis, what then happened? There was reversible injury at first, wasn't there? There was ischemia taking place, lack of oxygen. If there is no oxygen, then what kind of glycolysis do you have? Lack of oxygen, anaerobic glycolysis or are you going to produce as much pyruvate? No. You're going to produce more lactic acid? Sure you will. Anaerobic glycolysis, lactic acid in that area. What happens to your pH? It decreases. Alright. So what happens to your enzymes? Enzymes in environment where is acidic, is it more active or less active? Do not memorize this. What kind of necrosis? Coagulative necrosis right. What does coagulative mean? Preservation of your architecture. How is it that your preservation of your architecture? The enzymes aren’t working, is that clear? Gross changes, pale. Why is it a pale type of necrosis or pale type of infarct? Because there is only one blood supply to that particular tissue or organ. Light microscopy, early coagulant necrosis you know preservation of your architecture. Wavy fibers. So what are you seeing here in this schematic is cardiomyocytes and they should be nice and parallel normally. Remember this from histology. You have seen this before and the cardiomyocytes should be nice and parallel, should be nice and straight and they should have intercalated discs. Remember? And those intercalated discs are your gap junctions. So that your heart can beat as one unit called syncytium. Okay. So what then happens here earlier on 0 to 24 hours, you might get wavy fibers. You see that. It is wavy. It shouldn't be like that. Early changes. Next this is an acute MI. So any type of acute inflammatory response, what are you going to bring in? Neutrophils, good. Next, now things we will talk about later is that remember, management. 03:19 What are you trying to do? You're trying to bust that clot. If you want to bust a clot, what might you introduce? Re-perfusion injury. We will talk about this later. And when there is re-perfusion injury, you might then introduce tons of calcium. You see that? Tons of calcium coming in, and therefore causing quite a bit of damage as we shall see, complications. We have ventricular arrhythmias, may be heart failure, worst case scenario when you have arrhythmia, what may then happen? The heart might just stop, cardiac arrest. Welcome to cardiogenic shock. 03:48 Let us continue. 1 to 3 days, if it is 1 to 3 days now what happens to this necrosis? It is rather extensive. Now you have lots of neutrophils coming in and now after three days, what kind of pericarditis might this be? This is three days, so therefore this is fibrinous pericarditis. 04:07 Versus what other type of pericarditis might you see please in pathology? Dressler's, right. 04:14 Dressler's pericarditis and as we go through cardiology, we will take a look at the difference in timeline between fibrinous pericarditis, which will be days, versus Dressler, which could be three weeks to a month or perhaps even a little bit more, but not within three days. It is that clear. That must be understood and if your patient does have pericarditis, then what happens? You lean forward, I feel so much better; you lean back, oh my goodness gracious you are creating friction, pericarditis. And you do inspiration, that makes it worse, doesn't it? Welcome to pericarditis in general. Things that you guys know, but just to make sure that we put things into context. Let us go to 3 to 14 days and now we are beyond three days. 04:56 We are getting into weeks. So now the neutrophils are going to be replaced by whom? Macrophages and take a look at the cartoon there. That is hyperemic. What does that mean? That means after three days, the heart and the tissue is trying to recover. Then necrosis is irreversible. 05:13 What about the surrounding tissue? Well you can have a rim of hyperemia, is that clear? That is within two weeks. Rim of hyperemia. That is the most important point there. Macrophages are coming in. Now let us go into complications now. With this, I am going to walk you through this as well. So now when you think about repair process. Close your eyes. Think about repair process okay. Now you think about repair process, then should you bringing in collagen? Sure. Who lays down that collagen? What is the name of that cell? Come on. Good. Fibroblast. And you are going to have a scar and is this scar always a good thing? Not in the heart. So that if you have a scar formation taking place in the heart, what happens to the conduction system? That could be affected. Welcome to arrhythmia. Next, what if we have fibrosis and that scar wasn't strong, what then happens? I want to you think about the ventricle and let us say that the ventricular wall with the scar is quite weak. Are you with me? So with all that pressure, what is going to happen? A ventricular aneurysm, right. With that aneurysm, what does that mean? Ballooning. At some point, what may then happen to the wall? It might give away. 06:21 What is that called? Rupture. Okay, now let me ask you something. When you have rupture taking place, how quickly is that fluid building up in the pericardium? Once again, you walk me through this, how quickly is that fluid accumulating in pericardial cavity? Like that. I don't care if it is even a measly 200 milliliters, a little amount of fluid rapidly accumulating in the pericardial cavity, by definition, is what? Good. Pericardial tamponade. Are you seeing this? Good. Let us continue. There might be papillary muscle rupture. At some point when your heart starts dying, then what happens to the mitral root or even the aortic root? It might then become expanded. Welcome to what please? Valvular heart disease. What kind? If you have root dilation, don’t memorize it. Root dilation what is that going to give you? Regurgitation type of valvular heart diseases, isn't it? Let us continue. Now next you have what is known as your pseudoaneurysm and you're worried about there once again ruptures, what we have talked about. 07:23 It is macrophage-mediated structural degradation. All of these things at some point in time may give you serious complications. Let us going to weeks now. Weeks we have scar formation. 07:34 We have lots of collagen as such and you're paying attention at Dressler syndrome. So what is the difference between fibrinous and Dressler? They are both pericarditis, fibrinous pericarditis would be the normal type of inflammatory process that you might see within three days. However, if you have an autoimmune response for whatever reason and you might then result in pericarditis, weeks to months later, then you are thinking about Dressler. It is that simple and it is that clear. These are some of the most important changes that you want to pay attention to when you are dealing with myocardial infarction in terms of hours, days, weeks and months. 08:13 You pay attention to these tables. You are in fantastic shape.
About the Lecture
The lecture Ischemic Heart Disease: Development by Carlo Raj, MD is from the course Ischemic Heart Disease: Basic Principles with Carlo Raj.
Included Quiz Questions
A patient has non-ischemic chest pain and a friction rub the day after myocardial infarction. What characteristics of pain are expected?
- Improved by sitting up and leaning forward
- Improved by lying supine
- Worse with sitting up and leaning forward
- Better with deep inspiration
- Tender to palpation
Which of the following pericardial complications can occur more than 2 weeks after a myocardial infarction (MI)?
- Dressler syndrome (post-cardiac injury syndrome)
- Pericardial effusion due to myocardial rupture
- Peri-infarction pericarditis
- Pericardial tamponade
- Fibrinous pericarditis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture on the pathological timeline of MI and IHD.
i like it so much . thank you i like it so much . thank you i like it so much . thank you
Very good lecture about the MI chronology. The Professor explains very well what we can read in "First Aid".