Playlist
Show Playlist
Hide Playlist
Acute vs. Chronic Inflammation
-
Slides Acute and Chronic Inflammation Overview.pdf
-
Download Lecture Overview
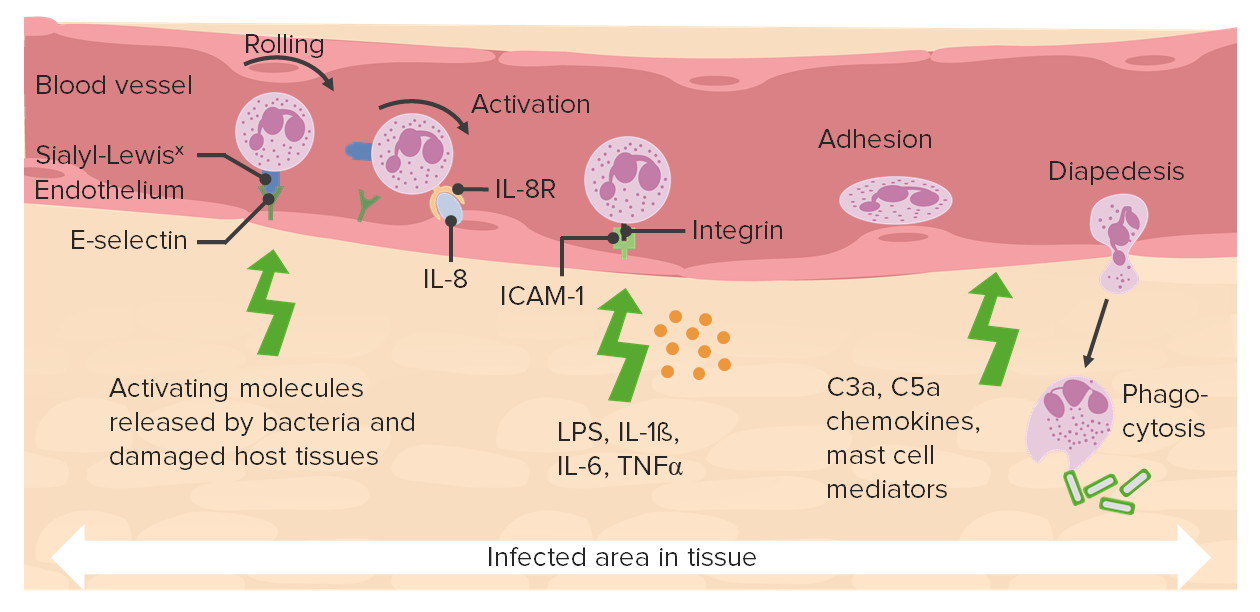
00:00 Welcome. 00:02 The topic for today is to begin looking at the inflammatory response that occurs in the setting of injury, and specifically necrosis. 00:13 Acute inflammation is going to be the first step. 00:16 And so for this topic, we're going to do kind of an overview to understand where acute inflammation fits into the total scheme of things. 00:27 Inflammation is actually divided into two components: Innate immunity, and adaptive immunity. 00:35 Adaptive immunity are T and B cells. 00:37 And we'll come back to those in a subsequent set of discussions. 00:42 Today, we're going to be talking mostly almost exclusively about innate immunity. 00:48 And the components of innate immunity are acute and chronic. 00:52 Okay, easy enough. 00:54 And that really has to do with when they appear? And how long they last? And are they early or are they late? So there are various components in the acute and chronic inflammatory response. 01:08 That's where we're headed today. 01:11 Inflammation: Innate immunity is happens because it anticipates that if we have necrosis, if we have injury that has caused cell death, that was one, either caused by an infection, and there are nasty infectious pathogens roaming around, or that zone of necrosis can be very soon infected. 01:36 Necrotic tissue is a beautiful culture medium. 01:39 And if we don't get rid of that, bacteria that are in the environment can set up shop in there and then we're in a world of trouble. 01:49 So we have this innate immunity to deal with necrosis. 01:55 Again, assuming that it's either caused by infection or will soon be infected. 02:00 So the goals of innate immunity. 02:02 The goals of this inflammatory response is to subdue any infection that might be there. That's one. 02:09 Number two, it's to remove necrotic debris because we don't want to leave dead stuff lying around, because that could be a source for subsequent infection. 02:18 So we want to clean up the mess. 02:20 And then if at all possible, number three, restore normal function. 02:25 So that's the goal of inflammation. 02:27 And it works pretty well for about 90% of infections, and works pretty well for a lot of necrotic injury. 02:37 Too cool. That's where we are. 02:39 Okay, so acute inflammation. Big picture things. 02:43 It's the first responder. 02:45 It occurs within hours to days after an injury. 02:52 The major cell that's going to be involved is shown on the right hand side. It's the neutrophil. 02:57 It's called a neutrophil because the granules within it in this white blood cell, don't stain well with our typical stains, so they are neutral. 03:08 The neutrophil is also called a polymorphonuclear leukocyte. 03:12 that's because the nuclear component, as you see there can be in multiple forms and shapes. 03:18 So it's a polymorphonuclear cell. 03:21 And it can also be called a PMN polymorphonuclear, or a poly. 03:26 So there are lots of different names that we will use. 03:28 And I'll try to stick with neutrophil as we're going through this, but just so you're aware. 03:33 So the neutrophil is the major cell that's involved in the acute inflammatory response. 03:37 It's the major player. 03:40 Here, it's shown in the bloodstream. 03:41 It's shown amongst a bunch of red blood cells, but it actually can crawl out and do its job in the tissue. 03:48 So it has the ability to have mobility. 03:52 The acute inflammatory response getting back over to our bulleted points, there's an initial vascular change. 03:59 The vessels in an area where there is inflammation where there's been necrosis become dilated, and they have increased permeability. 04:06 This is to improve blood flow into that area. 04:09 To deliver more neutrophils and more of the mediators that neutrophils will provide. 04:16 The cells that are there, the neutrophils are very short-lived. 04:19 In fact, they die within a day after they're synthesize on the bone marrow. 04:23 They die within 10 hours after they crawl out of the bloodstream and start doing their job. 04:28 So they're very short lived cells. 04:30 And that's part of the beauty of the acute inflammatory response, it goes away pretty quickly because the length of the cells that get the length and duration of survivability of the cells that crawl out, is pretty short. 04:43 They do their job in part by eating but in part by making very potent short-lived mediators. 04:51 Important point about this is that those short-lived mediators don't care what they're acting on. 04:56 They will do damage not only to bugs, pathogens, but they can also potentially do damage to host tissues. 05:05 So they work really well for sterilizing the wound, but they can cause a lot of bystander injury. 05:12 They sterilize the site, that's why they're there. 05:16 And they also begin the process of degrading the debris. 05:19 They release a lot of proteases. 05:21 Again, proteases don't care what protein they're acting on, they're just going to be degrading them. 05:26 So you can have specific destruction of things that are necrotic. 05:31 But you may also get destruction of normal tissues that are in the vicinity. 05:34 So there may be bystander injury. 05:37 The neutrophils are going to set the stage for the subsequent chronic inflammation that's on the next slide. 05:42 So they are first on the scene and they kind of set the stage. 05:47 Next players in the sequence. 05:50 And these form the major cells of chronic inflammation are the monocyte-macrophage lineage. 05:57 So it's the second response, chronic inflammation comes later. 06:00 That's why it's chronic, and it persists. 06:02 It can last for days, or weeks, or months or even years, depending on the circumstance. 06:07 It is driven largely by the monocyte. 06:10 Here we see the monocyte, which is the precursor to the macrophage. 06:15 In the bloodstream, it circulates as this kind of bilobed larger cell, that once it crawls out of the bloodstream and into the tissue can become a very long-lived macrophage. 06:28 And the macrophage in the tissues can live for the lifespan of the host. 06:31 So these as opposed to neutrophils, which only live a very short period of time, these can live potentially forever. 06:38 This is a macrophage. 06:39 After it's crawled out into the tissue, and it's out there with a variety of other cell types, it's a very granular cell. 06:45 We will spend a whole bunch of time talking about the macrophage. 06:48 So never fear, we will revisit this cell, and he will become your good friend. 06:55 Macrophages do part of their job by making potent, short-lived mediators. 06:58 So much like the neutrophil, they secrete proteases and a variety of other mediators that can be extremely potent in doing their job. 07:09 And are usually short-lived, but they have the potential for bystander injury. 07:13 They are the definitive clean-up crew. 07:15 So the first ones on the scene, the neutrophils do a lot of it, but not all of it. 07:19 And then the macrophages will be the final ultimate cleaner. 07:25 They also will orchestrate subsequent stages. 07:28 So we've now cleaned up all the necrotic mess. 07:30 Now what? Well, we either have to heal and regenerate that tissue if we can, or we need to make scar. 07:38 We can't just leave a vacuum. 07:40 And the people who are going to coordinate this... 07:42 the cell that's going to coordinate this, orchestrate this be the field marshal is going to be the macrophage. 07:50 Okay, so we will spend as they say, a lot more time talking about macrophages when we talk about the inflammatory process.
About the Lecture
The lecture Acute vs. Chronic Inflammation by Richard Mitchell, MD, PhD is from the course Acute and Chronic Inflammation.
Included Quiz Questions
Which of the following is an important function of inflammation?
- Defense against infections
- Removal of apoptotic cell bodies
- Degradation of senescent cells
- Formation of immunological memory
- Deactivation of reactive oxygen species
Which of the following is true about neutrophils?
- They are recruited to the site of injury quickly and are short-lived cells
- They stay alive for a long period of time after they leave the circulation.
- They play an important role in healing and fibrosis.
- They typically have rounded or kidney-shaped nuclei and little cytoplasm.
- They release potent proteases that have high specificity for damaged cells or pathogens.
What is the predominant cell type in chronic inflammation?
- Macrophages
- Helmet cells
- Neutrophils
- Eosinophils
- Basophils
Which of the following is a hallmark of acute inflammation?
- Increased vascular permeability
- Vasoconstriction
- The formation of scar tissue
- Infiltration of the lymphocytes and plasma cells into the tissue site
- The onset of days-weeks after the injury
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
An excellent overview, brief and concise. Just the right amount of detail for an introduction is presented.
his way to explain is amazing. i love the silds so much
Really informative and to the point lectures that clearified my concepts