Playlist
Show Playlist
Hide Playlist
Endocrine Pancreas and Control of Insulin – Endocrine Pancreatic Hormones
-
Slides EndocrinePancreaticHormones EndocrinePathology.pdf
-
Download Lecture Overview
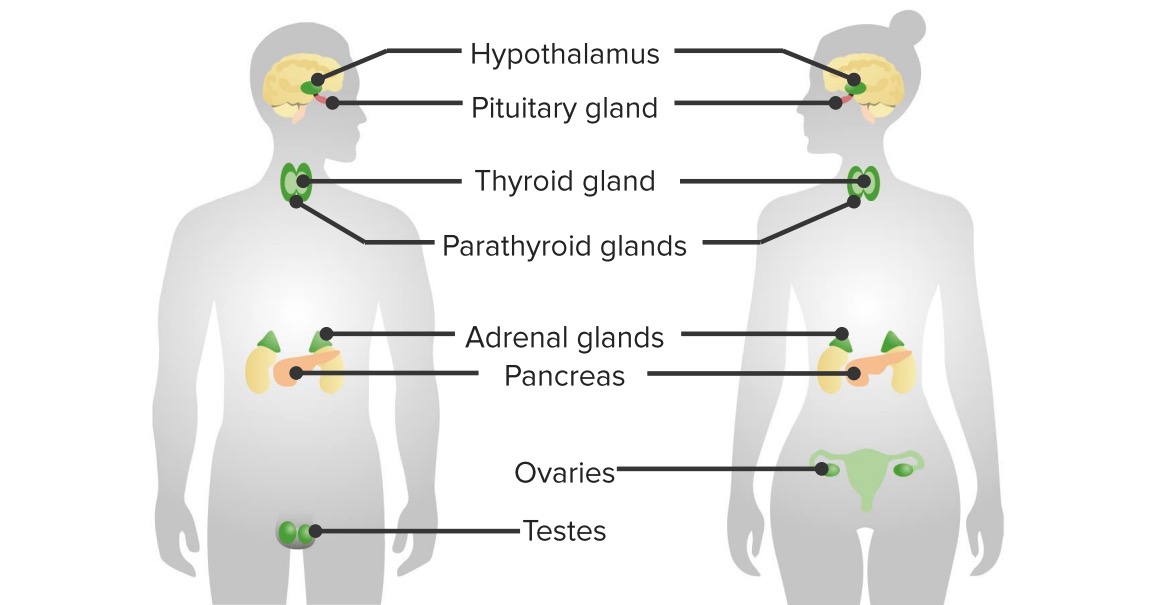
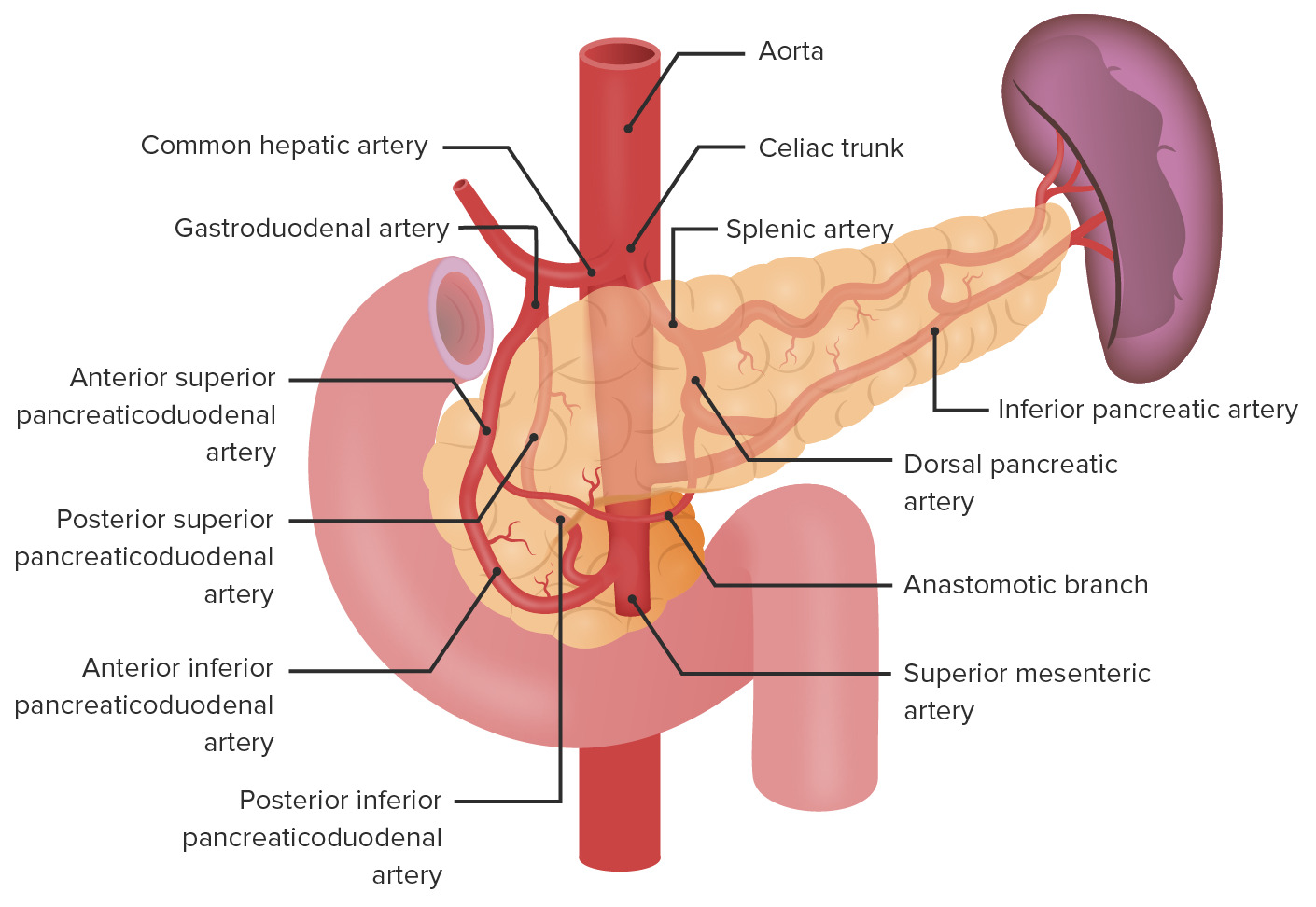
00:01 In order for us to truly understand endocrine pancreatic pathology, it is imperative that we have a good understanding of pancreatic function and hormones. 00:12 The endocrine pancreas itself, we have Islet cells and our focus in this entire section is going to be dealing with insulin and its effects on various organs throughout the entire body. 00:29 The picture here is showing you the pancreas and beta Islet cell. 00:35 We do something called immunohistochemistry in which it then identifies the insulin within the beta Islet cell. 00:44 On this table, a brief review of various hormones that are important for you to know from the pancreas. 00:51 The Alpha cells, measly 10 percent, but, my goodness, responsible for releasing an important hormone called Glucagon. 01:00 In pharmacology, you have heard of some of these GLP-1 analogues, things that you want to keep in mind. 01:08 Dorsally derived, embryologically anterior head, body and tail. 01:15 Beta cells comprise majority of your Islet cells at 70-80 percent, responsible for releasing insulin and every time there is insulin being released, do not forget endogenously, from your beta Islet cell, you are going to release your C peptides. 01:34 The D cells, 5 percent, release Somatostatin. 01:38 There is something called F cells, Pancreatic polypeptide, PP. 01:44 Let’s go to talk about that insulin. 01:47 Whenever-Whenever it is being produced in your beta Islet cells, it goes through the process of preproinsulin, proinsulin and insulin and you notice here at the bottom, a C peptide and that C peptide to you means that every time insulin is being churned out of a beta Islet cell into a circulation. 02:09 It is also along with it releasing C peptide. 02:12 The measuring of C peptide came to use for clinically to distinguish between that insulin which is being produced endogenously, example Insulinoma, versus that type of insulin in which maybe perhaps your patient is taking exogenously minus the C peptide. 02:27 Let’s go ahead and talk about what promotes insulin secretion. 02:33 What are we looking at here is in fact once again a beta Islet cell. 02:40 The glucose binds the gluc… glucose 2 transporters in the beta cells and these glucose 2 transporters are absolutely insulin independent, they have to be. 02:53 Why? What is this cell that we are looking at here? A beta Islet cell. 02:59 Where in the body are you? In the pancreas. 03:01 It is responsible for releasing insulin. 03:05 If it is responsible for releasing insulin, how could you have receptors that are dependent on insulin? Doesn’t make sense. 03:13 At the top left corner, you notice a flux of glucose coming into the cell and that is through your glucose transporter 2, insulin independent. 03:23 The glucose, close your eyes, the glucose will go through a biochemical process known as your glycolysis, just like you would in any healthy cell, right? And any healthy cell, the glucose will go through, well, we as humans, you carry out exhale, we breathe, bringing in oxygen and that is aerobic glycolysis. 03:44 Through aerobic glycolysis produce pyruvate going to [Inaudible 00:03:48] into the electron transfer chain and what did you produce? ATP, right, ATP, aerobic glycolysis, keep that in mind. 03:59 Let’s keep going. 04:01 What are we trying to do? Objective is to release insulin from a beta Islet cell. 04:08 You see the right lower quadrant of this cell? They are remaining dormant right now, who is remaining dormant? The vesicles, the vesicles remaining dormant and they are filled with insulin. 04:22 The objective of this entire discussion is how do we release insulin when we consume a piece of chocolate, carbohydrates, this is how we are doing it. 04:36 That ATP that was just produced, look what it does. 04:40 It blocks the potassium channel, pause. 04:44 When you, normally, [Inaudible 00:04:46] potassium, move into out or out to in… Normally, it moves from in to out, right? Always, efflux. 04:58 What charge does potassium have? Positive, hmm. 05:03 So, you… this ATP amazingly produced by glucose and through aerobic glycosylation, so on and so forth it, will block the potassium channel. 05:12 So, therefore, potassium is trapped within the cell. 05:16 Hmm, what kind of charge? A positive charge. 05:18 If you increase the positive charge within the cell, simple, simple physiology that you learned way back when, when you increase the positive charge what then happens? You create depolarization. 05:31 When it creates depolarization, you then hit threshold. 05:36 What do you do when you hit threshold? All or none theory, remember actual potential. 05:41 An actual potential has been generated by blocking the potassium channel and it doesn’t want to leave. 05:46 Is that important? Is it just all crazy by chemical details that I am giving you is irrelevant? Not at all. 05:53 There is a drug that blocks exactly where you see that ATP. 05:57 It is called sulfonylurea, right? Interesting. 06:02 Next, that potassium is blocked. 06:04 When it does, it creates your potassium that SU that you see there in green, the abbreviation stands for sulfonylurea drugs. 06:11 That’s exactly how they work. 06:14 Now, what kind of patient will be taking sulfonylurea, type 1 diabetic or type 2 diabetic? Obviously, type 2. 06:21 A type 1 diabetic doesn’t have insulin to begin with. 06:25 So, if the insulin isn’t there, how in the world is this drug even effective? It is not, use common sense. 06:32 So, type 2 diabetic using sulfonylurea, whenever you give sulfonylurea, what is the huge side effect that you are always worried about? Uh-oh, I might be releasing too much insulin from the pancreas and the patient may suffer from? Good, hypoglycemia. 06:50 Here you go, this is why. 06:52 And we are not quite done yet, are we? No, no, no. 06:55 So far, we have created an actual potential, whenever an actual potential is being generated, then you will then open up, here you go, down at the lower bottom, we are going to open up these Voltage-gated calcium channels. 07:06 Doesn’t this sound an awful, awful lot like your neuromuscular junction? That it does. 07:13 Here comes the calcium, here comes the calcium, here comes the calcium, fluxing in, massive influx, what do you think this calcium is going to do? It is going to then take these dormant vesicles that you see in the lower right quadrant, it is going to take these vesicles and fuse it with the membrane, but this time, the vesicles contain what? Insulin, not acetylcholine, this is not the neuromuscular junction, but my goodness, similar in behavior and then out will then come the insulin. 07:44 Out will then come the insulin and what does it do? It is then going to regulate the amount of glucose in circulation because you just took a piece of chocolate, you just had an appetizer with bread, whatever it may be, of course you are going to release insulin.
About the Lecture
The lecture Endocrine Pancreas and Control of Insulin – Endocrine Pancreatic Hormones by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
Which cells release somatostatin?
- Delta cells
- Alpha cells
- Beta cells
- PP cells
- F cells
A patient with type II diabetes was found unconscious and severely hypoglycemic. The patient had very high levels of circulating insulin. What laboratory study would be used to determine if the excess insulin was injected or produced by the patient?
- C-peptide
- Glucagon
- Proinsulin
- Somatostatin
- Fasting serum glucose
What is a step that leads to the release of insulin from a beta cell?
- Opening of Ca2+ channels
- Glucose oxidation to ADP
- Efflux of K+
- Opening of K+ channels
- GLUT 4 receptors bind to glucose
How do sulfonylurea drugs stimulate insulin secretion?
- By closing the K+ channels in a beta cell
- By preventing depolarization in a beta cell
- By preventing the release of glucagon from alpha cells
- By the closing of Ca2+ channels in beta cells
- By decreasing the sensitivity of GLUT 2 receptors
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Buena explicación introductoria, integra la explicación con farmacología, buena clase