Playlist
Show Playlist
Hide Playlist
Insulin: Therapy and Types – Treatment of Diabetes Mellitus
-
Slides HyperglycemiaDiabetesMellitus EndocrinePathology.pdf
-
Download Lecture Overview
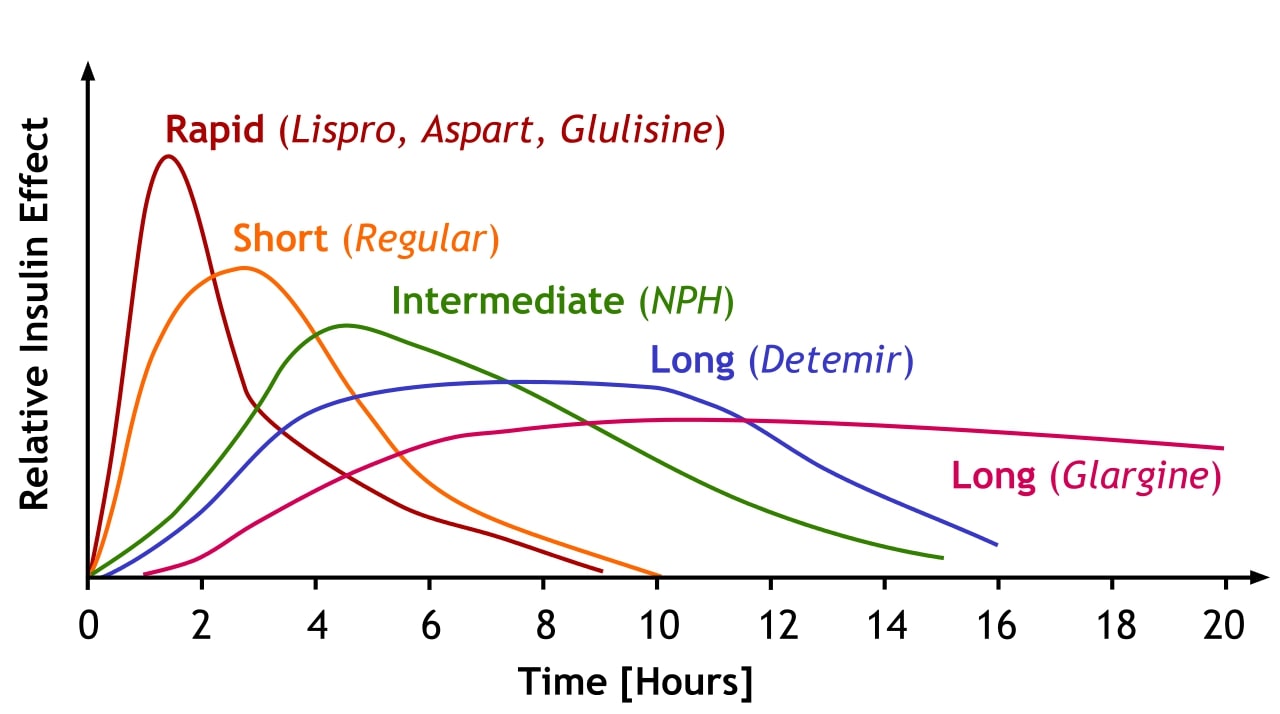
00:02 Now that we have the pathogenesis and the complications of diabetes mellitus behind us, we’ll take a look at an important topic of management of diabetes mellitus. 00:17 Ultimate objective… glycemic control, if you were able to properly monitor it, it would decrease the complications, big time, of… especially of your blood vessels. 00:29 Once again, we talked about microvascular complications of type I and type II diabetes mellitus. 00:35 You’re referring to your issues of diabetic retinopathy, diabetic nephropathy, diabetic neuropathy. 00:43 If it’s macrovascular diseases, that-that is referring to your atherosclerosis and you’re referring to coronary arterial disease, referring to your renal arterial stenosis, referring to cerebrovascular accidents, peripheral vascular disease… things that we have talked about with complications. 01:04 The Diabetic Association offers the following recommendations. 01:10 Prior to eating preprandial, you want your glucose level to be between 80 to 120… 80 to 120 milligrams per decilitre. 01:18 At bedtime before going to sleep, you would want your glucose levels to be between 100 and 140. 01:27 After eating, obviously your glucose levels would rise. 01:31 However, you still want it to be less than 180 because a big time pathologic effect of your diabetes mellitus is after you eat and you have the spikes and that’s the problem, isn’t it? The spikes over a long period of time, say years and years and years… the spikes are what really, truly causes the ultimate damage to let’s say the blood vessels in vascular diseases. 01:56 For you to be able to control the spikes, you should be able to control your complications. 02:04 You would like the HbA1C to be less than seven percent and what this means, once again, is that you have your glucose that is then being bound to haemoglobin and over let’s say the lifespan of an RBC will give you an average. 02:20 Less than seven percent is equivalent to… BG is blood glucose of approximately 150 milligrams per decilitre. 02:29 Therefore, if it starts rising above seven percent, you’re highly suspicious of your patient having diabetes mellitus. 02:36 Now, a type I diabetic requires insulin whereas with type II diabetes, we will be talking about a whole host of medications that hopefully will be able to give you what ADA recommends with glycemic control. 02:55 Begin our topic with insulin therapy and we have total daily dosage, TDD. 03:03 For type I typically 0.5 units. 03:05 I would know this in great detail and diabetes is such a huge issue in our society and so, therefore, the more that you know about this, the better off you’ll be on your wards and on your boards. 03:18 For type II diabetes the recommended starting dose for insulin is 0.2 per kg per day. 03:24 With type II, typically one to two units per kilogram per day; if on insulin therapy alone roughly half of your total daily dosage is given as basal. 03:33 insulin in the form of what’s known as glargine subcutaneous daily… daily. 03:38 Glargine, we’ll talk more about the drugs in detail. 03:42 We have determir subcutaneous two times a day; your NPH subcutaneous and I will talk to you about NPH coming up, or continuous subcutaneous insulin diffusion CSII. 03:54 To continue our discussion of insulin… the remaining half of TDD, so we have half and half, is given as parandial coverage. 04:04 Remember I told you once again, it’s quite important for you to make sure that you cover the spikes that take place with glucose after eating so this then covers the meal and the spikes. 04:17 Generally, this is given as a rapid acting insulin just prior to breakfast so that you are then preventing the spikes that I was referring to. 04:25 I’ll give you a few management or regimens and which we will walk through the different times of the day and different regimens that are quite commonly asked on your boards. 04:36 Insulin is the only current approved therapy for treatment of diabetes during pregnancy. 04:45 The types of insulin… it’s important that you pay attention to the types, big time. 04:50 If it’s rapid acting, the drugs include… one of the names include lispro, aspart and what’s known as glulisine. 05:00 Rapid acting, onset… minutes five to fifteen. 05:06 This is typically given so that you can then prevent the spikes from occurring. 05:10 The peak will be approximately an hour. 05:12 Keep it simple for right now, give yourself a clue. 05:16 Generally speaking, as you go through the table, and then at some point come back in, highlight or commit to memory the details. 05:27 Duration about two to four hours, so rapid acting… lispro is a big one. 05:32 Regular… this is once again minutes, but double that of rapid with onset. 05:40 The peak here regular a little bit later, so approximately two to four hours; duration is a little bit longer five to eight hours. 05:48 To make your life a little bit easier, if you wish to double each one of this, for example, rapid onset 15 minutes, regular onset 30 minutes. 06:00 Peak in rapid one hour; the peak in regular two hours. 06:04 The duration in rapid four hours; regular we have eight hours. 06:09 At first, keep it simple, give yourself a pattern; if you’re not familiar with the details then you go back. 06:16 Then we have something called intermediate and we’ll refer to this as being NPH. 06:22 Onset here a lot longer two hours; peak a lot longer at 10 hours or 6 to 10; duration almost an entire day… intermediate. 06:35 Then we have long-acting…we have glargine and detemir. 06:40 Two hours for onset pretty much the same as intermediate; there is absolutely no peak or non-effective peak. 06:47 The duration here will be a day at least or perhaps even more especially with glargine. 06:55 We’ll take the table here and I’ll give you a few graphs upcoming in which a couple of regimens become very important to you so that you have an idea as to what kind of graph and how to utilize it when you’re dealing with management. 07:06 Let’s take a look, examples of insulin regimens. 07:09 Remember that NPH means intermediate and we have the rapid acting regular and with regular, you probably want to double that of what you find with rapid-acting referring to lispro. 07:21 At first, I’d like for us to start at the top and the middle. 07:25 The X-axis refers to the times in a day so we have morning, we have afternoon, evening at night. 07:32 And you’ll notice that we have given in the morning regular and with regular, remember it takes about double that of onset. 07:40 So, you’re looking at approximately 30 minutes of onset and you’re looking at approximately two hours of it peaking. 07:46 In the meantime, the one in the morning gives… well, we have given your NPH intermediate. 07:53 This then covers what’s occurring throughout the entire day. 07:58 Next, in the evening, you’ll be given regular once again and you’ll also give your intermediate so that you can cover what’s occurring at night with your spikes. 08:12 Let’s take a look at what happens in the bottom another regimen. 08:17 Lispro refers to your rapid acting and by rapid acting, we’re referring to 15 minutes with it, onset approximately an hour for it to peak. 08:27 What’s occurring here is that with every meal… morning breakfast, afternoon lunch, evening dinner… you’re trying to maintain or trying to control that spike by giving the rapid acting. 08:39 In the meantime, to make sure that you cover yourself throughout the entire day, you then have your NPH. 08:47 Now, what we’re seeing here on the X-axis would be various meals obviously… breakfast, Now, what we’re seeing here on the X-axis would be various meals obviously… breakfast, lunch and supper, okay, supper S, dinner. 08:55 And then on the bottom and to the right, we have another regimen. 08:57 Different coverages just to give you an idea as to how insulin regimens work. 09:01 You divide these with the times of the day, you divide these with the meals of the day and depending as to what you want to use or combination of intermediate-regular, intermediate-rapid-acting and so on and so forth.
About the Lecture
The lecture Insulin: Therapy and Types – Treatment of Diabetes Mellitus by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
What is the recommended range of pre-meal blood glucose levels in healthy non-diabetics?
- 72-90 mg/dL
- 100-120 mg/dL
- 100–140 mg/dL
- >180 mg/dL
- 140–180 mg/dL
What is the HbA1C goal for diabetic patients?
- < 7%
- < 6%
- < 8%
- < 9%
- < 10%
What is the typical total daily dosage of insulin for type I diabetes mellitus patients?
- 0.5 units/kg/day
- 1 unit/kg/day
- 1.5 units/kg/day
- 2 units/kg/day
- 3 units/kg/day
Which insulin preparation would be given to avoid drastic blood glucose spikes immediately after a meal?
- Insulin aspart
- NPH
- Intermediate insulin
- Insulin glargine
- Insulin detemir
What is NOT true regarding the use of insulin regimens?
- TDD is identical for type I and type II DM patients.
- Long-acting insulin preparations are intended to maintain blood glucose throughout the day.
- Meals require the addition of short-acting or regular insulin in order to control blood glucose.
- Half of the administered insulin maintains basal blood glucose levels; the other half addresses blood glucose spikes associated with meals.
- Insulin is the only approved therapy for diabetes during pregnancy.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |