Playlist
Show Playlist
Hide Playlist
Retired - Oral Agents for Diabetes Mellitus Type 2 – Treatment of Diabetes Mellitus
-
Slides HyperglycemiaDiabetesMellitus EndocrinePathology.pdf
-
Download Lecture Overview
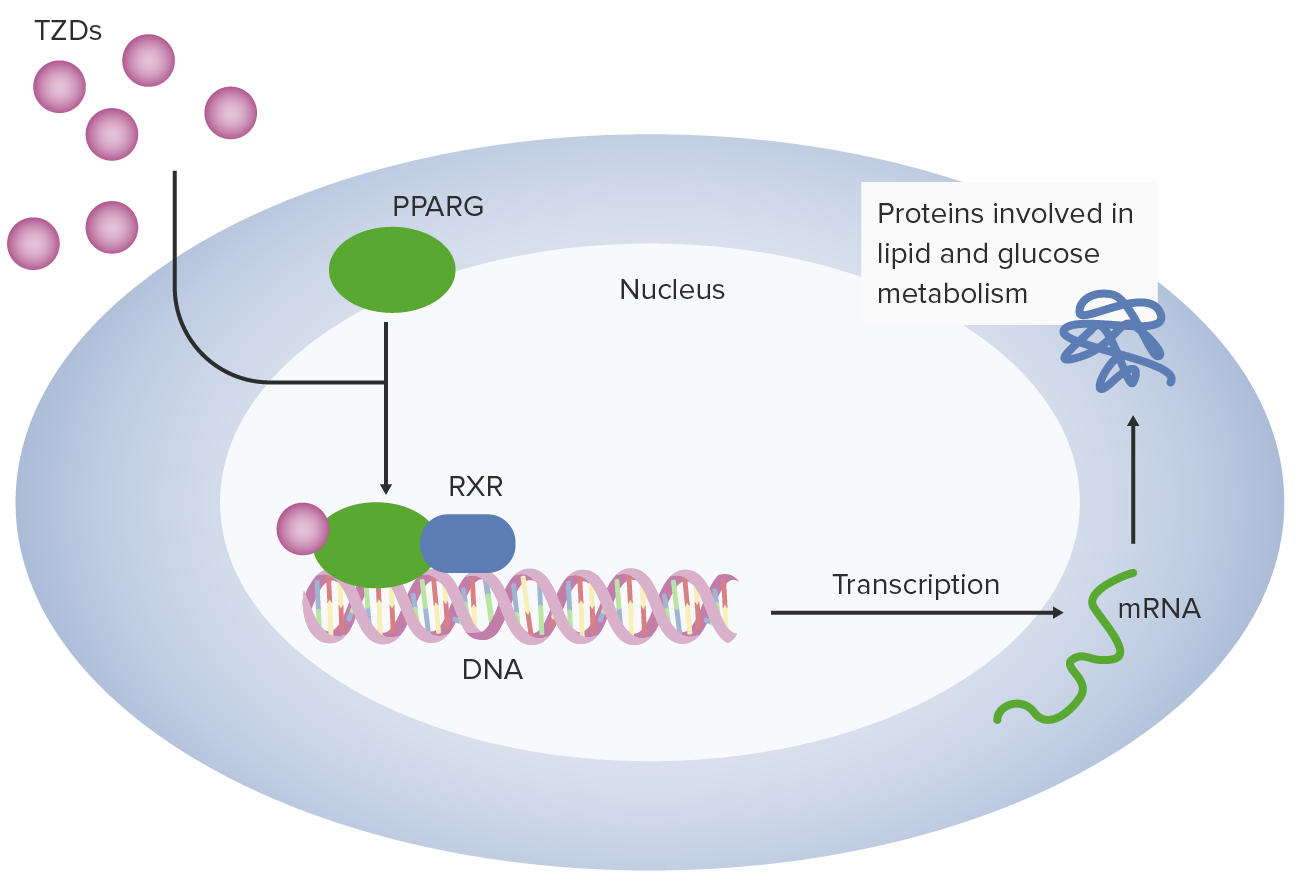
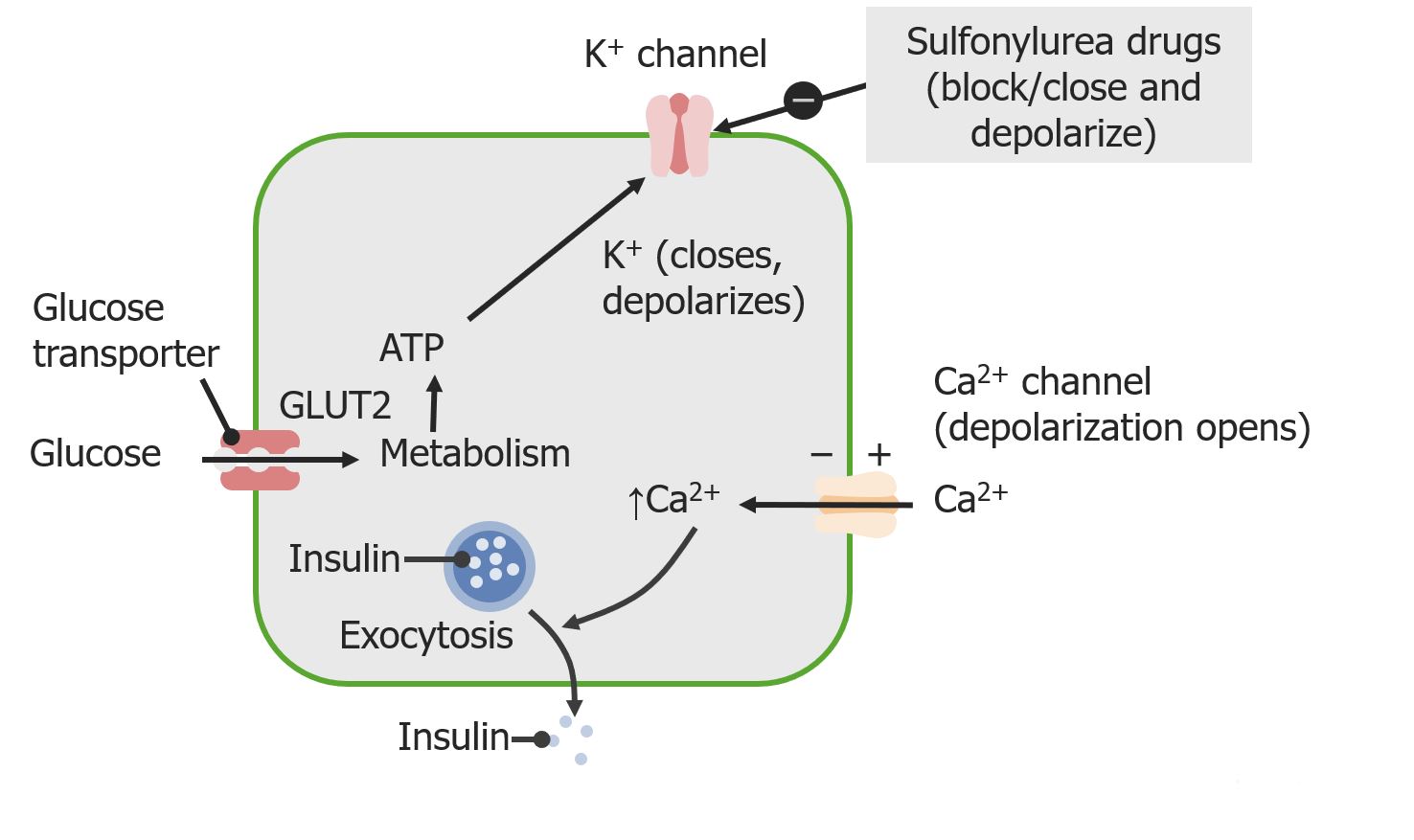
00:01 Let’s take a look at metformin. 00:03 Mechanism… you’re doing everything in the power these drugs are so that it can properly exhaust the glucose within your circulation. 00:12 How does it go by doing that? It actually inhibits the liver from releasing glucose, inhibits gluconeogenesis and also peripherally may then increase the uptake of glucose. 00:26 Metformin, the clinical use, typically first line of treatment in overweight patients. 00:32 Before you do any of this, what’s your first step of management? I’ve mentioned this over and over again, lifestyle modification, exercise, diet… exercise, diet. 00:41 It is associated with modest weight loss, no risk of hypoglycemia as monotherapy. 00:48 But,, there is an interesting side-effect that you want to know from metformin, it’s lactic acidosis. 00:54 It is also very importantly contraindicated in a renal disease, severe hepatic disease and congestive heart failure. 01:00 Put liver and kidney together contraindicated when such diseases are concomitantly present. 01:08 The GI side effects of metformin are the following. 01:11 Nausea, diarrhoea; minimized by starting low with dose type of titration. 01:17 Metformin and its complete, complete picture of what you want to know for your boards and wards. 01:23 Now, we come to a family and this family, well, maybe your uncle’s name is thiazolidine and your aunt’s family’s name is dione, put them together you have thiazolidine-dione. 01:34 What’s up with that? We have two of them the drugs that you want to know, rosiglitazone and we have pioglitazone. 01:42 Look for the suffix glitazone. 01:47 How does this decrease your glucose? Increase in peripheral sensitivity of the receptors for insulin thus enhances and increase the uptake of glucose. 01:58 Once again, here under monotherapy, no hyperglycemia and reduces the insulin requirement. 02:03 Remember this is type II diabetic. 02:06 This is contraindicated in class II and IV CHF or active liver disease… the glitazones are. 02:16 Monitor liver function test extremely important may then… remember a lot of effects in the liver here; causes weight gain and edema because it may actually release insulin and insulin is anabolic. 02:28 Concern over increased cardiovascular event seen with especially rosiglitazone; associated with bone fracture risk in women. 02:38 Important side-effects here for both your metformin and thiazolidinediones. 02:43 Let’s continue with our discussion and here, we have sulfonylureas. 02:47 Well, sulfonylureas include the following. 02:49 We have glyburide, we have glimepiride and we have glipizide. 02:54 You want to know the suffix -ide, -ide, -ide. 02:56 What’s sulfonylureas? We’ve talked about the mechanism of action, blocks the potassium channel, increase the release of insulin and you are absolutely at risk of hypoglycemia. 03:08 Here, however, remember you have increase in insulin release, you can have increase in C-peptide and you will find here sulfonylurea perhaps in serum or the urine. 03:21 There is a hypersensitivity that you want to be very familiar with sulfonylureas, sulfonamides… sulfo, sulfo, sulfo drugs. 03:29 Next, we take a look at our glinides, if you see this suffix glinide then you’re thinking about pancreatic insulin secretion, reduces post prandial hyperglycemia that your most obvious, important clinical application of your meglitinides. 03:54 Mild type of glycemia risk, liver disease, multiple daily dosing with meals, meals, meals… that’s what your focus should be on please with the suffix glinides. 04:03 And we have acarbose. 04:07 Now, for the most part ,rarely used; however, you need to know it because of mechanism of action. 04:15 It delays glucose absorption by inhibiting intestinal alpha-glucosidase… they love that. 04:23 If you inhibit intestinal alpha-glucosidase then what are you doing? You’re not taking up the glucose from the intestine. 04:32 Now because of this, its indication would be with once again post-prandial, there’s no hyperglycemia here with monotherapy. 04:41 However, if you block the glucose being taken up by the intestine after meal, you can expect there to be, well, I’m not sure as to whether or not you want to be near this patient. 04:53 Flatulence, cramps and diarrhoea is what you’re paying attention to. 04:58 Where are you with acarbose? Think about this way, a – without carbohydrate reabsorption… acarbose… flatulence and diarrhoea. 05:10 Then we have something called DPP-IV inhibitors and these are gliptines. 05:16 So, a couple of suffixes that you want to pay attention to, you have –gliptines, we have our –ides, we have –glinides, and we have our –glitizides. 05:28 Here, if you are to inhibit your dipeptidyl peptidase DPP-IV which then inactives GLP-1. 05:38 That’s the mechanism of action for this newer agent, but really at this point, none of the studies clinically at this juncture for need to comment any further. 05:49 Please note 1 DPP-IV and this is a gliptin drug. 05:54 Now, we have a drug, we’ll talk about a few drugs in greater detail here and this known as your exenatide incretin effect… incretin is an important topic, a lot of research on this. 06:07 Oral glucose has a greater stimulatory effect on insulin secretion than IV glucose for sure because you must be able to get that glucose metabolized and get from the intestine into circulation so that you can then allow for that glucose to work on the beta-islet cell to release the insulin. 06:24 Hence, any type of test that you do here… have you heard of an IV glucose tolerance test? No, oral glucose tolerance test… incretin effect. 06:35 Now, this effect is mediated by severe or, excuse me, several GI peptides particularly what’s known as your glucagon-like peptide 1. 06:43 GLP-1 is produced in small intestine known as the L cell GLP in response to nutrients. 06:51 The action of GLP is the following. 06:53 Stimulates pancreas to make insulin, slows gastric emptying and inhibits inappropriate post-meal glucagon release and reduces your food intake, will give you a feeling it’s incretin effect, a GLP-1 type of issue. 07:10 Exenatide naturally occurring component of your, well, here we have what’s known as the heloderma suspectum saliva and sequence identified with GLP-1. 07:22 Resistant to DPP-IV degradation and therefore exhibits a prolonged half-life. 07:26 Remember DPP-IV, the –gliptine that I was talking to you on that table earlier, this is resistant to DPP-IV so that you can have more of your incretin effect. 07:40 Used twice daily, same effect as GLP-1 which is glucose dependent augmentation associated with weight loss. 07:48 Side effect nausea; acute pancreatitis is a big deal. 07:52 Approved for use for type II diabetes without concurrent insulin use obviously otherwise you’re risking the risk of hypoglycemia. 08:02 It may result to HbA1C up to one percent… that is significant. 08:07 Remember HbA1C of less than seven percent is equivalent to approximately a glucose level of 150. 08:15 Let’s take a look at another one in greater detail and we have our pramlintide. 08:21 Amylin, 37-amino acid detail beta islet cell; deficient in type I diabetes mellitus. 08:28 Relative deficiency in type II; action slows gastric emptying, reduces inappropriate glucagon secretion and weight loss… welcome to pramlintide. 08:41 It’s an amylin analog, mealtime subcutaneous, same effect as amylin itself as we just mentioned in the previous slide. 08:51 Side effect - nausea, here once again may decrease AbH1C up to one percent. 08:57 I would know pramlintide only so that you have one analog of amylin.
About the Lecture
The lecture Retired - Oral Agents for Diabetes Mellitus Type 2 – Treatment of Diabetes Mellitus by Carlo Raj, MD is from the course Pancreatic Disease and Diabetes.
Included Quiz Questions
What is the most serious adverse effect of Metformin?
- Lactic acidosis
- Liver failure
- Hypoglycemia
- Increased ICP
- Hirsutism
A type 2 diabetes patient is told they must get their LFTs measured regularly due to the medication they are on. Which is the most likely agent they are taking?
- Rosiglitizone
- Metformin
- Glipizide
- Acarbose
- Sitagliptin
A patient requires medication therapy for Type II DM. They are compliant on their other medications but state that they are allergic to sulfa drugs. Knowing this information, which of the following would you NOT prescribe to this patient?
- Glyburide
- Metformin
- Nateglinide
- Acarbose
Which of the following is inhibited by acarbose?
- Alpha-glucosidase
- Pancreatic insulin secretion
- GLP-1
- Dipeptidyl peptidase IV
- PPR4
Which of the following medications is naturally secreted from the beta islet cells and can be used in both Type I and Type II DM?
- Amylin
- Nateglinide
- Exenatide
- Glimepiride
- Sitagliptin
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
good summary. The presentation should be updated to include sodium-glucose transport proteins (SGLT2) inhibitors like dapagliflozin.