Playlist
Show Playlist
Hide Playlist
Diabetes Insipidus and Pituitary Tumors
-
Slides 01-02-01 Adrenal Pituitary.pdf
-
Download Lecture Overview
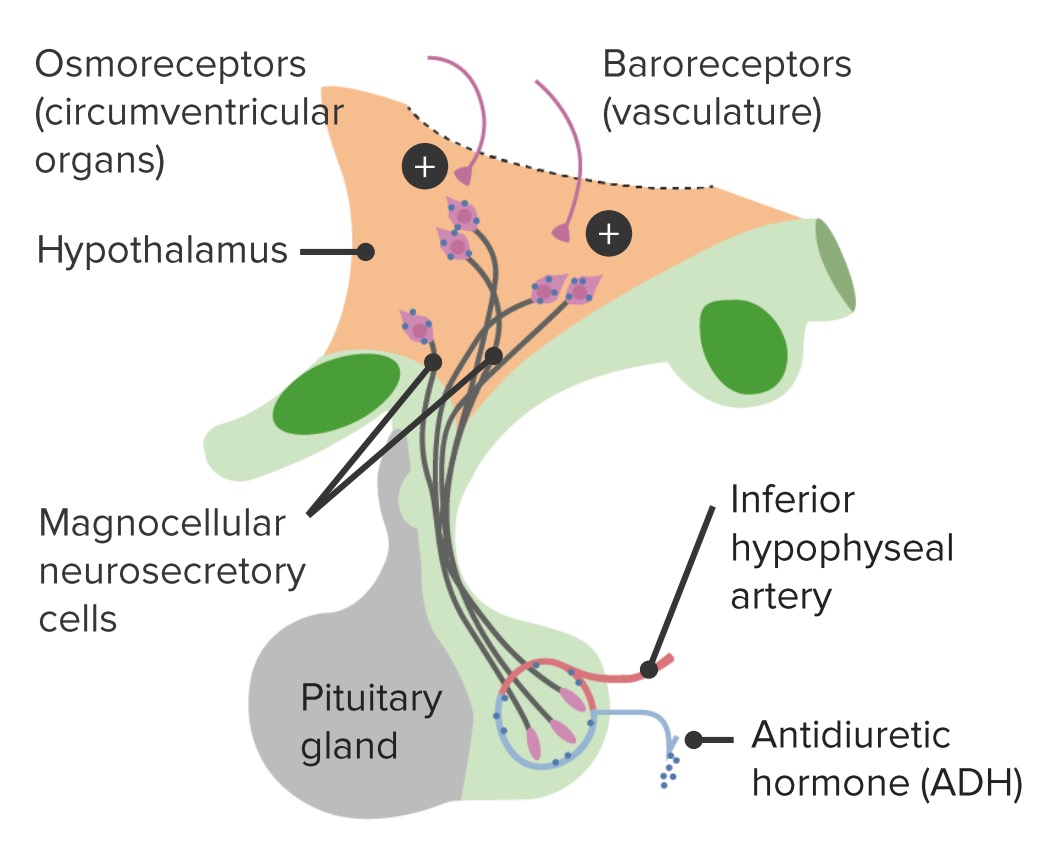
00:01 The causes of diabetes insipidus include neurosurgery or head trauma, pituitary mass lesions, and infiltrative disorders of the pituitary like sarcoidosis. 00:12 It is an inadequate production of antidiuretic hormone by the posterior pituitary gland. 00:17 In the presence of ADH, aquaporin water channels are inserted into the collecting tubules and allow water to be reabsorbed. 00:25 In the absence of ADH, excessive water is excreted by the kidneys. 00:30 Excretion of more than three liters of urine per day is considered polyuria. 00:34 The severity of diabetes insipidus varies with the completeness of the deficiency. 00:40 Patients describe mild to extreme polyuria and corresponding thirst, and partial diabetes insipidus is common. 00:49 Frank hypernatremia is unusual because patients develop extreme thirst and polydipsia, and with free access to water, they can maintain their serum sodium in the high normal range. 01:01 When patients do not drink enough to replace water lost in the urine due to poor or absent thirst drive or lack of free access to water, they develop hypernatremia. 01:12 In the patient with polyuria, diabetes insipidus is diagnosed with a simultaneous lab evidence of inability to concentrate urine in the face of elevated serum sodium, and osmolarity with inappropriately low urine osmolarity. 01:28 If necessary, a water deprivation test can be performed. 01:33 The treatment of DI consists of the infusion of desmopressin otherwise known as DDAVP. 01:41 This can be administered intranasally or subcutaneously. 01:47 Let's revise the clinically significant pituitary hormones deficiency states. 01:53 In the case of ACTH and cortisol, the initial test is a simultaneous ACTH and cortisol test. 02:01 The causes of the deficiency include exogenous oral, intravenous, intramuscular, or topical steroid supplementation which suppresses the hypothalamic pituitary axis. 02:14 In the case of TSH, T4, and T3, the initial test is a simultaneous TSH and free T4 evaluation. 02:22 Remember that you can't use a TSH response to monitor therapy because of the secondary nature of the hypothyroidism. 02:33 With regards to growth hormone, the test is insulin-derived growth factor 1 and a growth hormone-releasing hormone-arginine test can be used to confirm the diagnosis. 02:45 In the case of luteinizing hormone and follicle-stimulating hormone, simultaneously checking both hormones, and a total testosterone in a male and estradiol in a female will help making the diagnosis. 02:58 The causes of these deficiencies are in those patients who have known Kalman syndrome, or in women who exercise excessively, have severe illness or severe infection. 03:10 Let’s talk about the workup of a pituitary mass. 03:13 This first step is to determine whether or not the mass is causing any mass effect and clinical symptoms. 03:20 Also, is the mass secreting excess hormones, and finally, whether the mass has a propensity to grow and cause problems in the future? Benign pituitary adenomas are the most common tumor of the pituitary gland. 03:36 The tumors of less than one centimeter are defined as microadenomas and tumors larger than one centimeter are termed macroadenomas. 03:47 Incidentally, noted pituitary tumors are common. 03:50 Biochemical testing informed by findings on history and physical exam is a much more cost effective approach. 03:57 Initial tests for pituitary incidentally noted masses include an 8 AM cortisol level, a thyroid-stimulating hormone level, a T4, a prolactin level, and an IGF-1. 04:11 The mass effects of pituitary tumors mainly manifest as headache. 04:15 Pituitary masses can also compress the normal pituitary gland causing hormone deficiencies. 04:21 A large pituitary mass can cause panhypopituitarism which is the impaired secretion of all pituitary hormones. 04:29 The optic chiasm, just superior to the pituitary gland, in a large pituitary mass, may be compressed causing a result in loss of vision. 04:40 Mild peripheral vision loss may manifest as bitemporal hemianopsia and progress on to complete blindness, usually as the tumor expands and compresses more of the optic chiasm. 04:54 Visual field testing is a sensitive measure of optic nerve damage and should be evaluated by an ophthalmologist. 05:02 Seizures and neurologic manifestations and invasion of the cavernous sinus cause damage to the cranial nerves particularly three, four, and six. 05:12 These are the ones that pass through the cavernous sinus and may manifest with diplopia and extraocular muscle palsies or paralysis. 05:22 Let's talk about the treatment of clinically nonfunctioning pituitary tumors. 05:27 In nonfunctioning pituitary tumors that cause a mass effect, we need to remove them by surgery. 05:32 The most common surgical approach is the transsphenoidal approach which takes place through the nares or the mouth. 05:39 Indications for surgery include mass effect particularly if there's a visual field defect, a tumor that abuts the optic chiasm, tumor growth or an invasive tumor invading into the brain or cavernous sinus, and a tumor close to the optic chiasm in a patient who plans to become pregnant because with the physiologic enlargement of the pituitary during pregnancy, that smaller tumor may increase and impinge on the optic chiasm. 06:07 The empty sella syndrome is diagnosed when the normal pituitary gland is not visualized or is excessively small on MRI. 06:14 It is a radiologic finding rather than a distinct clinical condition.
About the Lecture
The lecture Diabetes Insipidus and Pituitary Tumors by Michael Lazarus, MD is from the course Pituitary and Hypothalamic Disorders. It contains the following chapters:
- Diabetes Insipidus
- Pituitary Tumors
Included Quiz Questions
Which of the following best defines polyuria?
- More than 3 L of urine per day
- More than 6 L of urine per day
- More than 4 L of urine per day
- More than 5 L of urine per day
- More than 2 L of urine per day
Which of the following tests can confirm a diagnosis of diabetes insipidus?
- Water deprivation test
- Dexamethasone suppression test
- Oral glucose tolerance test (OGTT)
- Liver function tests (LFTs)
- Hemoglobin A1c
Which drug is used to treat central diabetes insipidus?
- Desmopressin
- Conivaptan
- Atosiban
- Bromocriptine
- Ganirelix
Customer reviews
2,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text