Playlist
Show Playlist
Hide Playlist
Types – Heart Failure
-
Slides 08 Cardiology Alpert.pdf
-
Download Lecture Overview
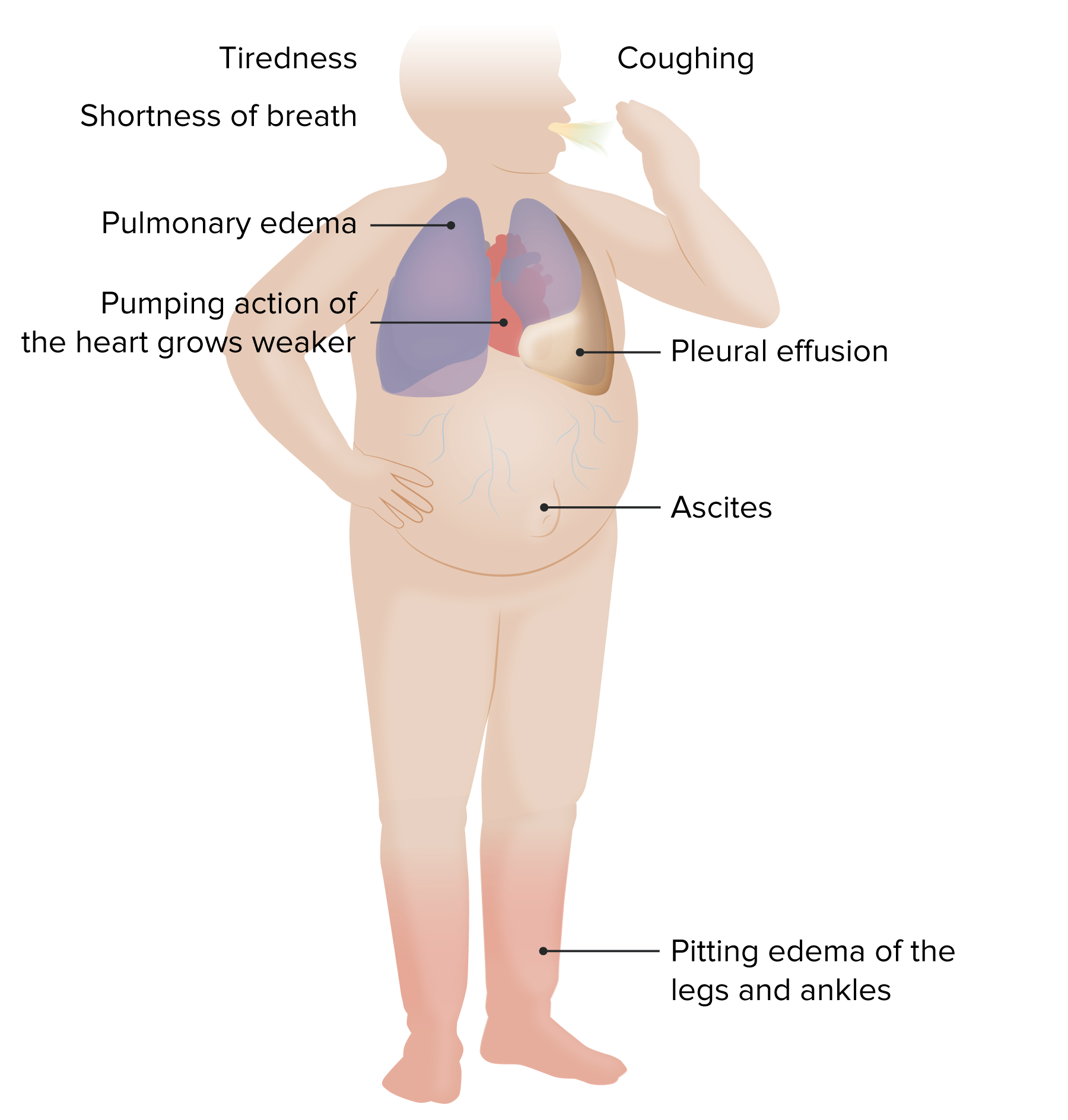
00:00 Now, again, we talked about the different kinds of heart failure systolic and diastolic. 00:06 But sometimes there are definitions based upon which ventricle is in the most trouble. 00:13 Most common is left-sided heart failure. 00:15 That's because the left ventricle has been injured. 00:18 But in some conditions such as severe lung disease with high pressures in the lung, you may just see isolated, right-sided heart failure. 00:28 So let's think about this for a moment. 00:29 With left-sided heart failure, the backup is going to be into the lungs. 00:34 Patients get fluid in the lungs, and they're short of breath. 00:37 So the edema is in the lungs with left-sided heart failure. 00:40 With right-sided heart failure, the backup is into the veins. 00:44 So you often see patients with fluid in the abdomen, fluid in the in the legs, so called peripheral edema. 00:53 And the left ventricle may be working just fine but it's not getting any blood from the right ventricle because the right ventricle is failing. 01:01 And of course, it's obvious. 01:03 What the left ventricle puts out depends on what the right ventricle puts out. 01:06 If they have to balance out, if they don't balance out, all the blood is going to end up on one side of the circulation or the other. 01:13 And then we've talked about before systolic heart failure, failure of contraction. 01:17 Diastolic heart failure, failure of relaxation. 01:21 Patients with chronic heart failure can be divided into two broad categories based on whether their ejection fraction is normal or reduced. 01:30 These two categories are heart failure with preserved ejection fraction called HFpEF, and heart failure with reduced ejection fraction called HFrEF. 01:40 Sometimes the third category is implied and used and that's heart failure with mildly reduced ejection fraction of 41 to 49%. 01:49 Because normal, of course, is above 50%. 01:52 For the most part, it's important to know the differences between the two distinct types of heart failure. 01:58 About half of the patients with heart failure have HFpEF and about half have HFrEF. 02:03 This distinction has prognostic value and it also helps guide therapy for the patients with heart failure. 02:09 Since therapy is different for HFpEF and HFrEF. 02:13 HFpEF is defined as a left ventricular ejection fraction of 50% or more in a patient with signs and symptoms of clinical heart failure. 02:22 Although most patients with HFpEF have diastolic dysfunction with elevated filling pressures. 02:27 Asymptomatic diastolic dysfunction can be seen with normal aging in individuals who do not have clinical symptoms. 02:35 So although people with diastolic dysfunction have a risk factor for HFpEF, these two terms are not synonymous. 02:43 HFpEF must be distinguished from other causes of heart failure in patients with an ejection fraction greater than 50%. 02:50 And these include patients with valvular heart disease, pericardial disease, cardiac amyloidosis, and high-output heart failure, such as that seen with severe anemia or hyperthyroidism. 03:03 Heart failure with reduced ejection fraction or HFrEF is defined as a left ventricular ejection fraction less than 50%. 03:11 Although an ejection fraction in the 40s is sometimes called mildly reduced ejection fraction. 03:17 Patients with HFrEF have difficulty with the pumping function of the left ventricle, the heart and by definition, a reduced ejection fraction in the left ventricle known as impaired systolic function. 03:32 Decreased ejection fraction leads to inadequate tissue perfusion, and of course influences the prognosis of the patient. 03:39 As you might expect, the lower the ejection fraction, often the worse the patient does and the more symptoms they have. 03:46 Cardiac remodeling is a response to hemodynamic load as well as neurohormonal activation. 03:53 Pathological remodeling can be seen with pressure overload due to hypertension or aortic stenosis can also be seen with volume overload with valvular regurgitation, or with cardiac injury, for example, myocardial infarction. 04:08 The management of HFrEF is quite different from the management of HFpEF. 04:13 And it's important to know the differences. 04:17 Here's just a little diagram to remind you how the whole body is a coordinated system. 04:22 You see the brain is connected to the heart. 04:25 The brain is connected to the kidneys. 04:27 They're all connected to the peripheral blood vessels. 04:30 And as we've talked about, when there's heart failure, or when there's dehydration or when there's hemorrhage, all of these factors become activated in an attempt to (A) restore the blood volume, and (B) restore the pumping ability of the heart. 04:46 And here they are all listed again. 04:48 Just as as we've talked about before, the central nervous system is critical. 04:53 The sympathetic nervous system is activated, the kidney through the renin-angiotensin system is activated. 05:00 And the ventricle gets increased volume and therefore uses the starling mechanism. 05:06 All of these things work together. 05:08 They work great if the patient's blood volume is down because of dehydration and hemorrhage. 05:13 They work against you when the problem is that the heart is not pumping enough. 05:18 And again, here you see a diagram that just shows you how all of these interact, how the decreased cardiac output can lead to lung congestion, and how increased peripheral pressure can lead to peripheral edema, the neurohormonal activations through the kidney that go on. 05:40 All of these things are working in a complete circus motion like a horse riding around the track in a circus, around and around they keep reinforcing each other. 05:53 And unfortunately, in heart failure leads to marked retention of water and salt that leads to the various symptoms that the heart failure patient has. 06:03 And the American Heart Association guidelines talk about various levels of heart failure. 06:09 Level A is somebody who's really predisposed to heart failure but has not developed it yet. 06:14 So that's somebody with high blood pressure, diabetes, hypercholesterolemia, hyperlipidemia, as we've talked about, that leads to atherosclerosis. 06:22 Heart failure hasn't developed yet, but the substrate if you will, is ready to go on and cause a heart condition that will lead to heart failure. 06:30 Grade B is when you're starting to have some very early signs of heart failure by some of our fancy tests, such as from the echocardiogram, but the patient is still asymptomatic. 06:43 Stage C is when the patient is already having symptoms. 06:46 They're tired, they're short of breath, they have peripheral edema, and stage D is when they're really incapacitated with heart failure marked severe symptoms of heart failure.
About the Lecture
The lecture Types – Heart Failure by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following is most likely to cause peripheral edema?
- Right-sided heart failure
- Heart failure with preserved ejection fraction
- Heart failure with reduced ejection fraction
- Interstitial lung disease
- Ischemia-induced heart failure
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |