Playlist
Show Playlist
Hide Playlist
Penis Disorders: Types and Clinical Representation
-
Slides Introduction Male Repro.pdf
-
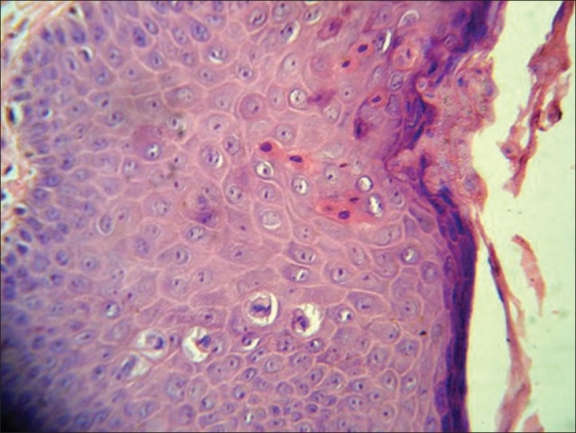
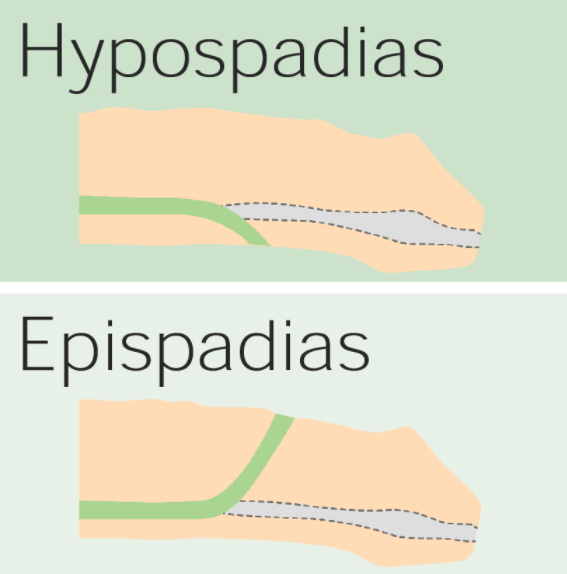
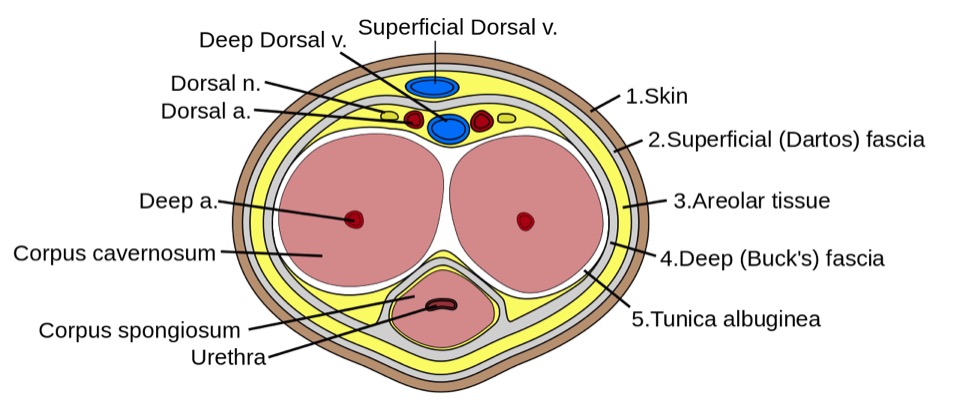
Download Lecture Overview
00:01 Our topic here in this table, incredibly important. 00:04 And it summarize some of the conditions embryologically and also we’ll go into our adult penile pathologies. 00:12 We’ll begin by looking at hypospadia. 00:14 If you take a look at simple picture here, we have the ventral portion of the penis in which that you find an opening. 00:19 And what does this mean to you? Embryologically, it’s the ventral surface of the penis due to failure of the urethral folds to fuse. 00:28 What happens? Well, hypospadia’s more common than epi, and you’re worried about with hypo, infection type of issues especially, well, if an organism get’s into -- Take a look at the picture -- that access to the ventral portion, then it might then get into urethra, and then get into the urinary bladder, welcome to cystitis. 00:50 Everything’s a story. 00:52 For the most part, 95% of your boards in medicine use concepts. 00:57 That’s what you should focus on always. 01:00 And we have epispadia, take a look at where the opening here is and this is on the dorsal surface of the penis. 01:06 What does this mean to you? This means that you have extrophy of the bladder which is a serious complication. 01:12 Just to make sure we’re clear, We have due to malpositioning of the genital tubercle, is the embryologic malformation with epispadia. 01:20 Whereas with hypospadia, what was it? Failure of urethral folds. 01:27 Well, if your patients in the above two were young because of congenital issues, well, here we’re still discussing penile pathology, but yes, this is also a young patient. 01:39 However, the problem is with phimosis is that the prepuce, inability to retract the prepuce over the glans. 01:48 Can you picture that, please? I want you to picture the glans and then let’s say that you have a child that did not have circumcision yet, okay? And so therefore, there is the fold, the foreskin, and literally what happens is the fact that the foreskin is trapping the structure underneath it. 02:04 What’s the structure? The penis. 02:07 So therefore literally you’re suffocating and you’re strangulating the penis with the foreskin. 02:14 You can’t even retract the prepuce over the glans versus -- I’ll talk to you about another condition upcoming called paraphimosis in a second. 02:23 So what happens here? Well, accumulation of smegma. 02:27 Smegma would be the type of fluid that – not the most hygienic and there used to be a research and there used to be theories out there that maybe perhaps smegma, accumulation of smegma in uncircumcised males then perhaps at some point lead into squamous cell cancer. 02:44 Well, that’s too controversial. 02:46 They won’t ask you that. 02:47 But imagine if you can’t properly clean up the area and then smegma and then perhaps infection known as balanitis. 02:57 As I said, there might be small risk of squamous cell cancer. 03:01 Circumcision gives a decreased risk of spread of -- well it is important. 03:04 Well, it is important. 03:06 Circumcision decreases spread -- now this is statistically proven -- of both very important viruses that are a part your STI or sexually transmitted infections, HPV and HIV. 03:18 At least know that much in terms of what the process or what circumcision will provide in terms of protection for your male. 03:31 Continuing our discussion of penile pathology, this time with paraphimosis. 03:34 What does this mean to you? Phimosis means, once again, you weren’t able to properly retract the foreskin over the prepuce. 03:43 Whereas now, paraphimosis literally – Now I want you to picture the glans and you’re right about to get into the shaft. 03:50 And at that point literally, it’s like you taking your hands and choking me around me my neck and you're choking literally underneath the glans. 03:58 The retraction of tight foreskin over the prepuce can lead to strangulation and infarction of the glans penis. 04:07 Please know this as being the definition for paraphimosis. 04:11 If you’re confused, go back to the previous discussion that we just had with phimosis. 04:19 Iatrogenic in children and congestive type of ischemia is what you’re thinking about here with paraphimosis. 04:29 Next, we have what’s known as Peyronie disease. 04:31 If it’s one word to describe Peyronie disease, it’s the fact that there is fibrosis. 04:36 And there’s a couple of other things here that you’d find to be interesting with Peyronie disease. 04:42 It’s chronic inflammation. What does that mean to you? Fibrosis. 04:46 It’s fibrosis taking place over the penis, that’s correct. 04:49 So what does that mean to you? This is going to then be painful. 04:53 Painful, keep that in mind. 04:55 Chronic inflammation causing increased thickness of the tunica albuginea and with that thickness surrounding the corpus cavernosa. 05:04 With that increase in thickness at some point in time, it may then cause – well, we’ll take look. 05:09 Differential diagnoses: Rupture of corpus cavernosa due to penile fracture. 05:14 So with that Peyronie disease, with this type of fibrosis, well, there’s another association to – If my hand looked like this, I can’t help it, okay? Let’s say I’m a patient that has this condition in my hand and my penis are both curved. 05:30 Why is my hand curved and why is my penis curved? Because in Peyronie disease in the hand that I’m the maneuver that I’m doing here is something called Dupuytren and these are all fibromatosis or fibrosis that’s taking place of these organs. 05:47 And when there is chronic inflammation of the penis, you call this Peyronie. 05:50 If it’s chronic inflammation of the hands and it contracts, that’s called Dupuytren. 05:55 Okay. So you’ve heard of Peyronie before, but you probably have heard it in the context of Dupuytren. 06:02 You have ischemic priapism, what does this mean to you? It means that you don’t have proper blood supply to the penis, and you should be thinking about something like sickle cell disease. 06:15 And sickle cell disease, think about that African American boy, and when he is playing, then you have your RBCs, which get sickled. 06:23 And when they get polymerized, then they behave like a thrombus. 06:27 So when they’re behaving like a thrombus in penile circulation, we have a condition called ischemic priapism. 06:34 In other words, what does this mean to you? This is opposite of erectile dysfunction. 06:38 This means that you will -- or the child or the boy or the male is experiencing painful erection, you must know the definition of greater than 4 hours. 06:49 Of course, we have drugs that do that such as Viagra and such, totally different mechanism. 06:53 Our focus here will be pathology. 06:56 Immediate treatment with, well, you have to, have to now decompress or decrease the amount of blood we have, corporal aspiration. 07:04 We have intracavernous type of phenylephrine and surgical decompression. 07:09 You almost want to think of this as being like increased intracranial pressure. 07:14 For example, if there’s a hematoma sometimes, what do you want to do? You put in a burr hole in the skull, you can relieve the pressure. 07:20 Kind of like what you’re doing here as well. 07:22 Important penile pathologies that you want to know for sure, some would be children and some would be adults. 07:28 Keep your patient in mind every single time you go through one of these diseases. 07:36 Our topic here brings us to what’s known as penile type of carcinoma in situ. 07:43 So CIS stands for carcinoma in situ. 07:47 So what does this mean to you? It means there is malignancy. 07:50 However, it doesn’t mean at this point that we’ve invaded. 07:54 Is that clear? Same concept that we did with cervix and vulva. 08:02 Remember the intraepithelial neoplasias. 08:04 At some point, they then went on to become in situ and if they invade, then it’s a totally different story. 08:11 Okay, so let’s talk about penile in situ. 08:14 Bowen disease in penile shaft presenting as leukoplakia. 08:20 I want us to stop here for a second. 08:22 Bowen disease, you want to memorize that. 08:25 Next, leukoplakia. 08:28 Well, many times, med students take a topic or whatever and they’re just kind of like put it somewhere and then they use it as a buzzword. 08:38 Don’t do that. 08:39 What I’m saying is leukoplakia, a lot of students and residents think, “Oh, it must be on the tongue.” Well, no. 08:45 You could have it on the tongue, but you must understand the definition of leukoplakia. 08:51 What it means is that the squamous cells are undergoing hyperplasia. 08:57 When they do, it takes on whitish color, leuko-plakia. 09:02 What kind of cells do you have on your tongue? Squamous cells. 09:07 What if there was trauma that was introduced to the tongue and now, the squamous cells undergo hyperplasia and it appears white. 09:15 Leukoplakia, that, you’ve heard of. 09:17 And with a tongue depressor, you can’t scrape that off. 09:21 You can’t scrape off squamous cells like you would oral thrush. 09:25 That’s when most – Med students have heard of this. 09:28 But if there’s leukoplakia elsewhere which just means squamous cell hyperplasia and there is a risk of going to cancer, here it’s on the penis. 09:38 Then you have Bowenoid. 09:40 Pick the name and dissect it. 09:42 The suffix –oid means like, correct? Epitheliod, leukomoid. 09:48 Here’s Bowenoid. 09:50 It’s called Bowenoid papulosis and presents as reddish papules and here, HPV16 in young men seems to be the causative agent perhaps. 10:01 Reddish papule, Bowenoid. 10:04 Red – D. 10:06 Bowenoid – D. 10:08 Bowen would be leukoplakia, whitish. 10:11 All part of a spectrum of CIS, carcinoma in situ. 10:18 Then we have erythroplasia of Querat of glans, presents as erythroplakia. 10:24 Very much sounds exactly the type of organization that you did with the tongue, doesn’t it? You have the white, that was leukoplakia. 10:31 and then you had the red, it was called erythroplakia, That was on the tongue and if there’s hyperplasia. 10:35 Here, if it’s on the penis, we have Bowen which is white. 10:39 And bowenoid, which is more reddish papules. 10:42 Whereas if it’s what’s something called erythroplasia of Queyrat of the glans, this then presents as erythroplakia. 10:50 Three different presentations, all the spectrum of CIS. 10:54 Students tend to confuse this and get questions wrong because you just didn’t take enough time to reinforce the information. 11:01 Just take a couple of things here, white, red and red. 11:04 Red papules and erythroplakia. 11:07 Now, we’re going into actual squamous cell cancer of the penis. 11:11 More common in Africa, Asia, South America, associated with the higher strains of HPV and we also have detected alter in a particular tumor suppressor gene called p16. 11:25 And if you remember correctly, p16 will be a tumor suppressor gene. 11:29 It inhibits the kinase, I-N-K, I-N-K, I-N-K. 11:33 If there’s a mutation in which the INK then becomes mutated, if you inhibit the inhibitor, “Uh-oh, what have you done?” You phosphorylated the Rb, removed the BRCA, E2F is allowed to run free and my G12S phase is unimpeded, my cells spend eternity in cell cycle. 11:50 Welcome to cancer. 11:51 Okay. 11:52 So single 60s, these are risk factors. 11:56 Single, amazingly. 11:57 So if a male is single, I’m saying that -- interesting, isn’t it? That he, by just default, single has increased risk for squamous cell cancer. 12:07 60s, the older you are and you’re single. 12:10 And also later circumcision, just know that and, as a theory, that often tested on the boards. 12:18 Big time important. 12:19 So this is with the penis. 12:21 And let’s talk about its spread, okay? Now what I’m trying to get at is there’s two spreads that students get confused with all the time. 12:30 Periaortic and para-aortic versus something here that we see with the penis. 12:36 What kind of cancer are we dealing with here? Penile cancer. 12:39 At some point, what other type of cancer will we deal with in which its spread would be para-aortic? Good. 12:46 Testicular. 12:48 Two different cancers, two different anatomical parts of the male. 12:53 Penile cancer, if it wishes to spread, would be lymphatic to superficial, to deep inguinal then to the external iliac lymph node. 13:04 Memorize that, commit that to memory. 13:06 I don’t care how you do it. 13:08 All I’m saying is do not confuse this with the spread that we will take a look at with testicular cancers in which it will then spread to the, lymphatically, para-aortic. 13:18 It’s easy to confuse the two. 13:19 They’re in the same vicinity, but please make sure you keep that separate for your boards and wards.
About the Lecture
The lecture Penis Disorders: Types and Clinical Representation by Carlo Raj, MD is from the course Male Reproductive System Diseases.
Included Quiz Questions
Which congenital malformation leads to hypospadias?
- Failure of the urethral folds to fuse
- Early fusion of the urethral folds
- Congenital absence of the urethral fold
- Malpositioning of the genital tubercle
- Hypertrophy of the urethral folds
What condition is associated with phimosis?
- Balanitis
- Exstrophy
- Abdominal wall defects
- Carcinoma in situ
- Scrotal squamous cell carcinoma
Congestive ischemia is seen with...?
- ...paraphimosis.
- ...phimosis.
- ...balanitis.
- ...epispadias.
- ...hypospadias.
What description best correlates with Peyronie disease?
- Chronic inflammation and thickness in the tunica albuginea
- Chronic inflammation and thickening in the tunica vaginalis
- Chronic inflammation and thickening in the corpus cavernosum
- Atrophy in the corpus cavernosum
- Atrophy in the tunica vaginalis
After how many hours with ischemic priapism does tissue damage start to occur?
- 4 hours
- 24 hours
- 0.5 hours
- 12 hours
- 1 hour
Which condition is NOT associated with carcinoma of the penis?
- Peyronie disease
- Leukoplakia
- Bowenoid papulosis
- Bowen disease
- Erythroplasia of Queyrat
In what order is the lymphatic spread of penile cancer?
- To superficial, then deep Inguinal lymph nodes, then to external iliac lymph nodes
- To para-aortic lymph nodes, then to left supraclavicular lymph nodes
- To external iliac lymph nodes, then to inguinal lymph nodes
- To superficial, then deep inguinal lymph nodes, then to para-aortic lymph nodes
- The lymphatic spread of penile cancer does not follow a particular pattern.
Customer reviews
3,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
1 customer review without text
1 user review without text