Playlist
Show Playlist
Hide Playlist
Central Diabetes Insipidus
-
Slides ActionOfADH EndocrinePathology.pdf
-
Download Lecture Overview
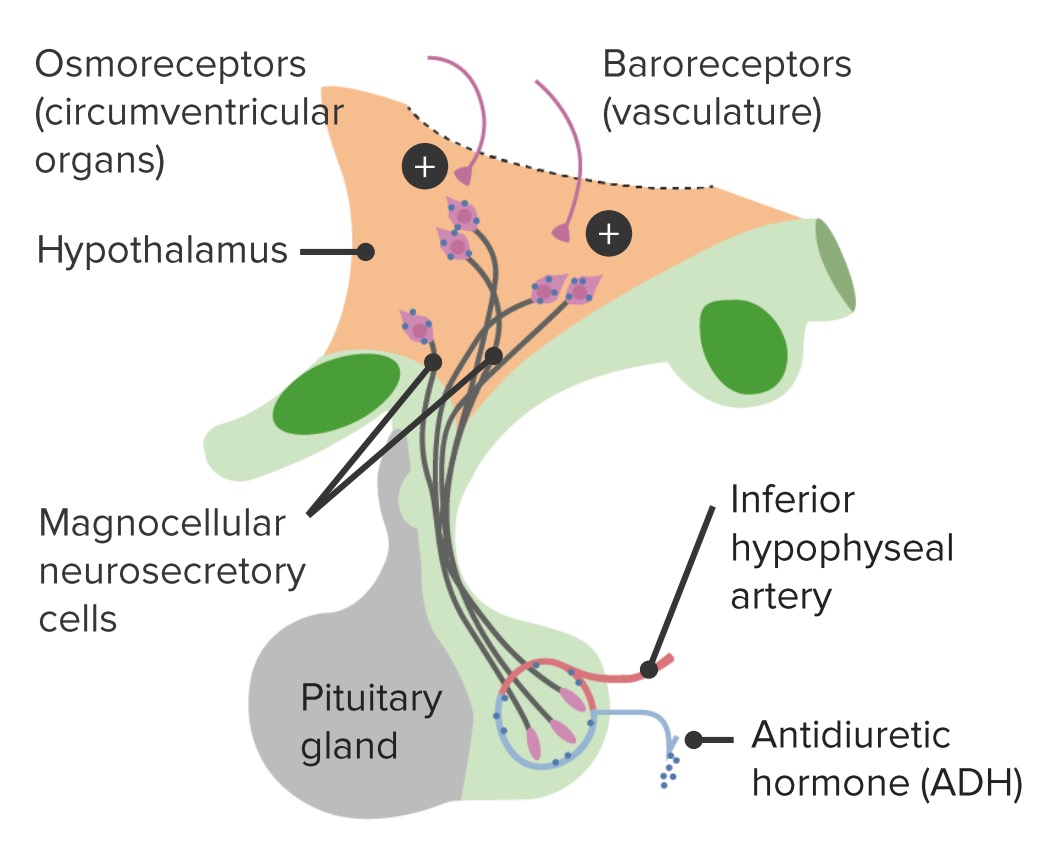
00:02 Let’s talk about central diabetes insipidus. 00:04 What’s my problem? I don’t have enough ADH, I just don’t. 00:10 What happened? Before we get there, urine osmolality - low; plasma osmolality - high; ADH level - decreased; receptor activity – well, even if the receptors are perfectly normal, which they are in central, it does not matter, the patient does not have ADH. 00:31 May follow head injury, now, be very careful here. 00:33 We talk about head injury. 00:35 That’s interesting, right? You would think-You would think by having head injury that you would lose ADH, that’s a possibility. 00:45 Or what if there is head injury and initially, you may actually release too much ADH? “So, Dr. Raj, you’re telling me both instances are possible?” That’s exactly what I’m telling you. 00:57 We see… we’re going to see this concept again in thyroid disorder. 01:01 In thyroid gland, with the colloid, initially when you destroy it, you might have too much T3, T4, as we shall see. 01:10 Okay. 01:11 So, with head injury, the trauma depletes the posterior pituitary gland of ADH stores. 01:16 Sure, that could happen. 01:17 Posterior pituitary, it cannot-it cannot properly secrete your ADH, your patient is central diabetes insipidus, but the receptors? Perfectly normal, keep that in mind because that’s important for us to manage your patient. 01:31 Because circulating levels of ADH are low, the entire DT/CD, by that we mean distal convoluted tubule and collecting duct are impermeable to water. 01:42 So, what kind of urine are you producing? Good, diluted urine. 01:45 What’s my plasma osmolality? Increased. 01:49 Large volume, polyuria, look how much urine you’re losing per day, 15 litres per day, that’s amazing. 01:58 So, what’s your next step of management? IV fluids, but “Dr. Raj, I’m already losing water.” Correct, you are, but my goodness gracious, you’re losing 15 litres of water per day, you need to hydrate your patient or your patient is dead. 02:17 Plasma osmolality, obviously increased, high values, extremely excessive. 02:21 Normally, when you have plasma osmolality that’s increased, what’s those receptors up in the hypothalamus? Good, osmoreceptors that we stimulated so that you normally secrete ADH. 02:34 So, how do you manage your patient with central diabetes insipidus? I told you over and over again, the receptors are perfectly normal, so go ahead and administer ADH and analogue such as, here you go, d-arginine vasopressin. 02:49 Keep arginine in mind, big time please. 02:53 Arginine is going to be a precursor for creating or synthesizing your vasopressin. 03:00 And as soon as you give this, what happens to urine osmolality? Initially, it was low, it starts rising; your plasma osmolality was high, it starts lowering. 03:12 Please, from henceforth, keep your two compartments completely separate and be able to do it as quickly as I’m doing it on your boards, you have to be able to. 03:22 Let’s talk about central more. 03:25 Most common cause would be, MC stands for most common, idiopathic autoimmune. 03:30 We have something called Wolfram syndrome; congenital hypopituitarism. 03:36 So, congenitally, the posterior pituitary was not present. 03:43 Tumors, primary or secondary, infiltrating the disease or infiltrating the posterior pituitary. 03:50 Let me give you an example. 03:51 What if your patient was the following? The patient had a “rash”, the-the patient was then given cortisol, but didn’t work. 04:00 The patient goes on to develop, let’s say couple of years later, arthritis type of issues. 04:05 NSAIDs and ibuprofen didn’t seem to work, years went by and now, the patient is polyuria. 04:13 Upon electron microscopy, you find birbeck granules. 04:16 Oh, I pretty much gave it away. 04:18 These tennis racket-type of structures and the patient comes back to be positive for CD1A, who is my patient? Good, Langerhans cell histiocytosis. 04:27 In Langerhans cell histiocytosis, do you remember when we talked about a cancer in WBC pathology? A cancer that is then, if left unimpeded, at some point in time, can infiltrate the posterior pituitary resulting in central diabetes insipidus. 04:47 Keep that in mind because Langerhans cell histiocytosis many times goes unnoticed for years upon years upon years until you get these bizarre symptoms such as polyuria, important causes of central diabetes insipidus. 05:05 Let’s talk about what happens. 05:10 Neurosurgery and trauma with typical triphasic response, what do you mean? Watch this. 05:17 Initial… anytime that you wish to choose any type of surgical answer for dealing with ADH in the posterior pituitary, you want to keep the triphasic response in mind. 05:32 What do you mean triphasic? It is possible that you might then destroy the posterior pituitary, initial polyuria phase begins within 24 hours. 05:43 ADH phase on, well, let’s keep that approximately a week, then permanent central diabetes insipidus once the ADH stores are completely, completely depleted. 05:58 Keep the triphasic in mind. 06:01 This theme or concept can also be used for thyroid, as you shall see. 06:06 So, if there’s neurosurgery being a cause of central diabetes insipidus, initially, you might actually release too much ADH. 06:14 Your patient looks and presents as SIADH. 06:20 Worst case scenario, if there is enough damage, you might completely deplete your patient, your patient presents with central diabetes insipidus. 06:30 Hypoxic encephalopathy, what does that mean? Another cause. 06:34 If there’s enough hypoxia taking place, especially of the brain region, understand the posterior pituitary is not going to function and nor is it going to release ADH. 06:46 These are all causes that you want to keep in mind for CDI, central diabetes insipidus. 06:54 Your patient presents with polyuria, nocturia is a big point and polydipsia. 07:02 Remember, this could be any age of a patient, it could be congenital or it could be an adult. 07:08 So, if you find the symptoms that we talked about along with the labs that I’ve given you and there’s nocturia highly differential should be CDI. 07:18 May present with neurologic deficit May develop a decreased bone mineral density at the lumbar spine and femoral neck, so think about where you are, lower back or by the hip. 07:31 Even when managed with desmopressin, the unfamiliar mechanism of V1 could be responsible for some of the issues that we’re seeing here for proper bone density. 07:41 You’re going to find this quite a bit with central diabetes insipidus, important clinical symptoms of your patient. 07:50 What I wish to show you here more so than the cranial nerves, this is not a review of neuroscience, but what I do want to show you immediately is the sphenoid sinus. 08:03 The manner in which you are then going to approach, take a look at the pituitary gland please and take a look at the sphenoidal sinus, the manner in which you will be then approaching the pituitary gland will be transsphenoidal surgery and as you pass through here, you are very close to a number of cranial nerves that you see here on the left. 08:28 And so, therefore, during transsphenoidal surgery and you have internal carotid artery, you want to keep all this in mind. 08:36 For example, anytime that you do surgery with a gland, things that you want to keep in mind is, well, let’s say that I’m trying to pass through the parotid gland, well, you know about the facial nerve. 08:48 As you are trying to reach up into the pituitary gland for whatever reason, maybe your patient has issues with an adenoma, there’s every possibility that you might have collateral damage.
About the Lecture
The lecture Central Diabetes Insipidus by Carlo Raj, MD is from the course Pituitary Gland Disorders.
Included Quiz Questions
What is NOT a characteristic of arginine vasopressin deficiency (AVP-D/central diabetes insipidus [CDI)?
- Normal functioning posterior pituitary
- Normal vasopressin receptors
- Low or no circulating vasopressin
- Urine concentration in response to vasopressin administration
- A large volume of dilute urine
Why is desmopressin the preferred treatment for arginine vasopressin deficiency (AVP-D/central diabetes insipidus [CDI)?
- Normal vasopressin receptors and low vasopressin are typical in AVP-D (CDI).
- Normal vasopressin receptors and high vasopressin are typical in AVP-D (CDI).
- Abnormal vasopressin receptors and low vasopressin are typical in AVP-D (CDI).
- Abnormal vasopressin receptors and high vasopressin are typical in AVP-D (CDI).
- Desmopressin is not the preferred treatment for AVP-D (CDI).
What is the most common cause of AVP-D (CDI)?
- Idiopathic
- Head trauma
- Congenital hypopituitarism
- Wolfram syndrome
- Tumor
What is not a common clinical manifestation in treatment-naive patients with complete AVP-D (CDI)?
- Edema
- Polyuria
- Nocturia
- Polydipsia
- Neurologic deficit
What is the triphasic response resulting in AVP-D (CDI) after neurosurgery?
- Polyuric phase — vasopressin phase — permanent CDI
- Vasopressin depletion — polyuric phase — vasopressin phase
- Vasopressin phase — polyuric phase — permanent AVP-D (CDI)
- Polyuric phase — vasopressin depletion — vasopressin phase
- Vasopressin depletion — polyuric phase — permanent AVP-D (CDI)
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
good explanation ye ye ye ye ye ye ye ye ye ye