Playlist
Show Playlist
Hide Playlist
Iron Deficiency Anemia: Iron Studies
-
Slides Iron Deficiency Anemia-Iron Studies.pdf
-
Download Lecture Overview
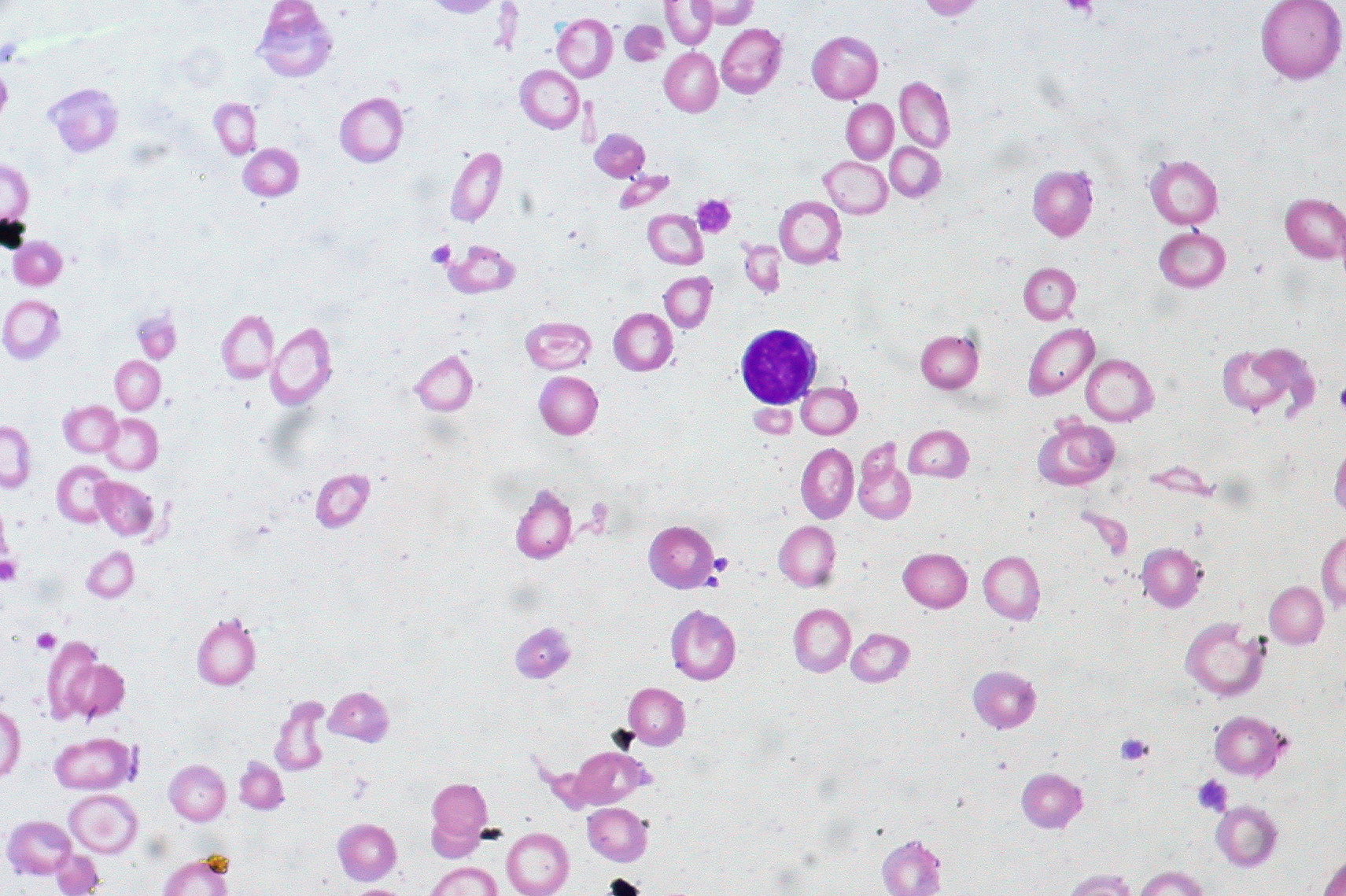
00:02 Okay. 00:02 So now, let’s walk through in order how to then evaluate your iron studies, shall we? Number one, and I’m going to walk you through this slowly again. 00:13 And then as we go through more of our type of microcytic anemias, I am going to go a heck a lot quicker. 00:17 So get it down now. 00:20 I introduced the normal in the previous discussion. 00:23 I told you number one, pay attention to serum iron. 00:25 Number two, you take a look at ferritin. 00:28 Ferritin has an inverse relationship with? What are you going to use, laboratory? Transferrin or TIBC? TIBC. 00:37 Inverse relationship with TIBC. 00:38 And number four, what’s that called? Transferrin saturation. 00:42 Okay, so those are the four that we looked in normal. 00:45 Let us now play around with iron deficiency. 00:50 Serum iron, obviously, decreased. 00:53 Number two. 00:54 You see that ferritin box right there? Wow! Very little green shade. 01:00 That green shade represents iron. 01:04 So very little ferritin, number two. 01:06 What kind of relationship does ferritin have with TIBC? Inverse relationship. 01:11 So therefore, a decrease in ferritin means an increase in TIBC. 01:16 Number three, your next question that you’re asking yourself is what is it that fills up this transferrin, this column that you see here on your left. 01:29 Now, it’s moved up because TIBC’s increased up to 500. 01:33 Total iron binding capacity’s increased. 01:36 So if your binding capacity’s increased, but you’re iron deficient, well, what is the body trying to do? It’s trying to bind as much iron that it can. 01:43 But it can’t find any, huh? Because you’re iron deficient. 01:48 Why? Maybe your female had menorrhagia, you get my point. 01:50 So the binding capacity’s increased. 01:54 But you can’t bind to any. 01:56 So therefore, what’s your saturation percentage? Decreased. 02:00 Clear? Now, tell about how the transferrin’s being saturated. 02:07 What does that mean? Does this mean that transferrin is delivering iron to itself? That makes no sense. 02:13 The transferrin is transporting the iron, Fe, to the bone marrow. 02:22 Why? Oh, I think that’s where RBC production is taking place? Yeah, that’s exactly what’s happening. 02:26 Okay. 02:28 So then, what is it that’s filling up this transferrin. 02:31 You won’t think of this as being -- ferritin kind of regulates that, okay? So if your ferritin’s decreased, then how in the world can you then release enough iron to saturate this big block. 02:40 You'd find it completely empty. 02:43 See this column here, and that whole thing is TIBC. 02:46 Welcome to iron deficiency. 02:49 Number one, serum iron decreased. 02:49 Number two, decreased ferritin. 02:50 Number three, increased TIBC. 02:53 And number four, you’d find a decrease in percentage saturation. 02:57 Let’s continue. 02:59 Laboratory values, in words, is what we just talked about. 03:01 A decreased hemoglobin, hematocrit, RBC count. 03:06 Well, that’s pretty nonspecific. 03:07 MCV, decreased, definitely puts you into the realm of microcytic. 03:12 What’s your magic number? Good. 03:16 Less than 80. 03:17 Next, stop. 03:18 If you have iron deficiency – I can’t even from proper heme or globin, which one? Heme. 03:25 Okay? So what is that iron gives -- What kind of color does iron give your heme? Red. 03:35 Red. 03:35 So if you’re iron deficient and you can’t form proper heme, what color is your RBC? Rather pale. 03:41 What do you call that? Pallor. 03:44 What about that central pallor? Should you have a little bit of central pallor in a normal RBC? Sure. 03:49 But what about in iron deficiency? That pallor, pallor, pallor increases. 03:53 So increased central pallor. 03:55 What do you call this clinically? Oh, yeah. 03:59 Hypochromic, there you go. 04:00 So what lab tells you that the RBC is hypochromic? Take a look. 04:08 MC -- you pay attention -- HC. 04:11 Hemoglobin concentration. 04:12 So once again, if you don’t have iron, I don’t have proper production of heme. 04:18 I don’t have proper amounts of hemoglobin concentration in my RBC. 04:24 What color is your RBC? Hypochromic. 04:25 Look at that. It makes perfect sense. 04:27 You have a decreased MCV and you had MCHC, what do you call this clinically? You call this hypochromic microcytic. 04:34 That you’ve memorized so many different times. 04:37 But to actually see in laboratory, isn’t that fascinating? I’m a dork. 04:42 I love this stuff because the labs actually speak to you. 04:44 Anything that laboratory was, EKG, ultrasounds, all these give you vital information. 04:51 Next, well, tell me about the RBCs in a peripheral blood smear. 04:55 Peripheral blood smear. 04:56 They’re microcytic, correct. And they’re hypochromic. 05:00 All at the same time? Could it be possible that you might have some RBCs that are bigger? Some are smaller. 05:06 So bigger, smaller, bigger – Can I be any more dramatic? So in a peripheral blood smear, you have big RBCs, little RBCs, big RBCs, little RBCs, and you then call this red blood cell distribution width. 05:21 Because you don’t have uniformity of your RBCs on a peripheral blood smear, guess what your RDW is. 05:30 Increased. 05:30 So what does that mean? Uniformity is what should come to mind when we think RDW. 05:36 You don’t have it usually with an iron deficiency type of picture. 05:41 Let’s move on. 05:42 That’s huge, huge. 05:44 That second and third bullet point are huge, aren’t they? For iron deficiency. 05:49 Now, what about your iron studies? Well, you tell me. 05:50 Close your eyes. 05:51 Serum iron, decreased. 05:54 Number two, ferritin, decreased. 05:55 Ferritin, decreased. TIBC, increased. 05:57 Transferrin saturation, decreased. 05:59 You see how easy that was? You spend time with that normal graph first in the previous discussion. 06:05 You go through this cycle that I’m giving you. 06:08 Every single time, you can’t miss a question. 06:12 Increased TIBC. 06:14 What does BC mean? Binding capacity. 06:18 but the problem is, you can’t bind to anything because you’re iron deficient. 06:24 On your left is going to be your pathology. 06:27 Let’s take a look at that central region. 06:28 See that increased pallor? “Compared to what, Dr. Raj?” Take a look at the right, that’s normal. 06:35 You see the central pallor in the right. 06:37 The pallor? Yeah, it’s there. 06:39 But not much. 06:39 On the left, oh, it’s too much. 06:41 There you go. 06:44 What lab gives you increased central pallor or lack of color? What gives you hypochromicity? MCHC. 06:53 Are we clear? So hemoglobin concentration is decreased on the left. 06:56 Therefore giving you hypochromic and to be technical, you know that MCV is decreased. 07:03 So microcytic hypochromic anemia, iron deficiency.
About the Lecture
The lecture Iron Deficiency Anemia: Iron Studies by Carlo Raj, MD is from the course Microcytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following best corresponds to laboratory values in iron deficiency anemia?
- Decreased ferritin, decreased serum iron, increased total iron-binding capacity
- Normal ferritin, decreased serum iron, and decreased total iron-binding capacity
- Decreased ferritin, decreased serum iron, and decreased total iron-binding capacity
- Decreased ferritin, increased serum iron, and increased total iron-binding capacity
- Increased ferritin, decreased serum iron, and increased total iron-binding capacity
Which of the following laboratory tests indicates hypochromia?
- Decreased mean corpuscular hemoglobin concentration
- Increased mean corpuscular hemoglobin concentration
- Increased red cell distribution width (RDW)
- Increased mean corpuscular volume (MCV)
- Decreased mean corpuscular volume (MCV)
The production of which of the following is mainly defective in iron deficiency anemia?
- Heme
- None of these
- Alpha globin chains
- Beta globin chains
- Protoporphyrin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
i love every dr. gaj lecture he gets into details - repeat many times - joyful
I like your lectures Dr, they are all very well explained thus allows us to pick up the concept quite easily! Thanks
Dr. Raj is really funny and makes the lecture engaging. His thought process is very logical, and it helps me really remember some of these more complicated concepts.