Playlist
Show Playlist
Hide Playlist
Small Lung Cancer
-
Slides PulmonaryNeoplasia RespiratoryPathology.pdf
-
Download Lecture Overview
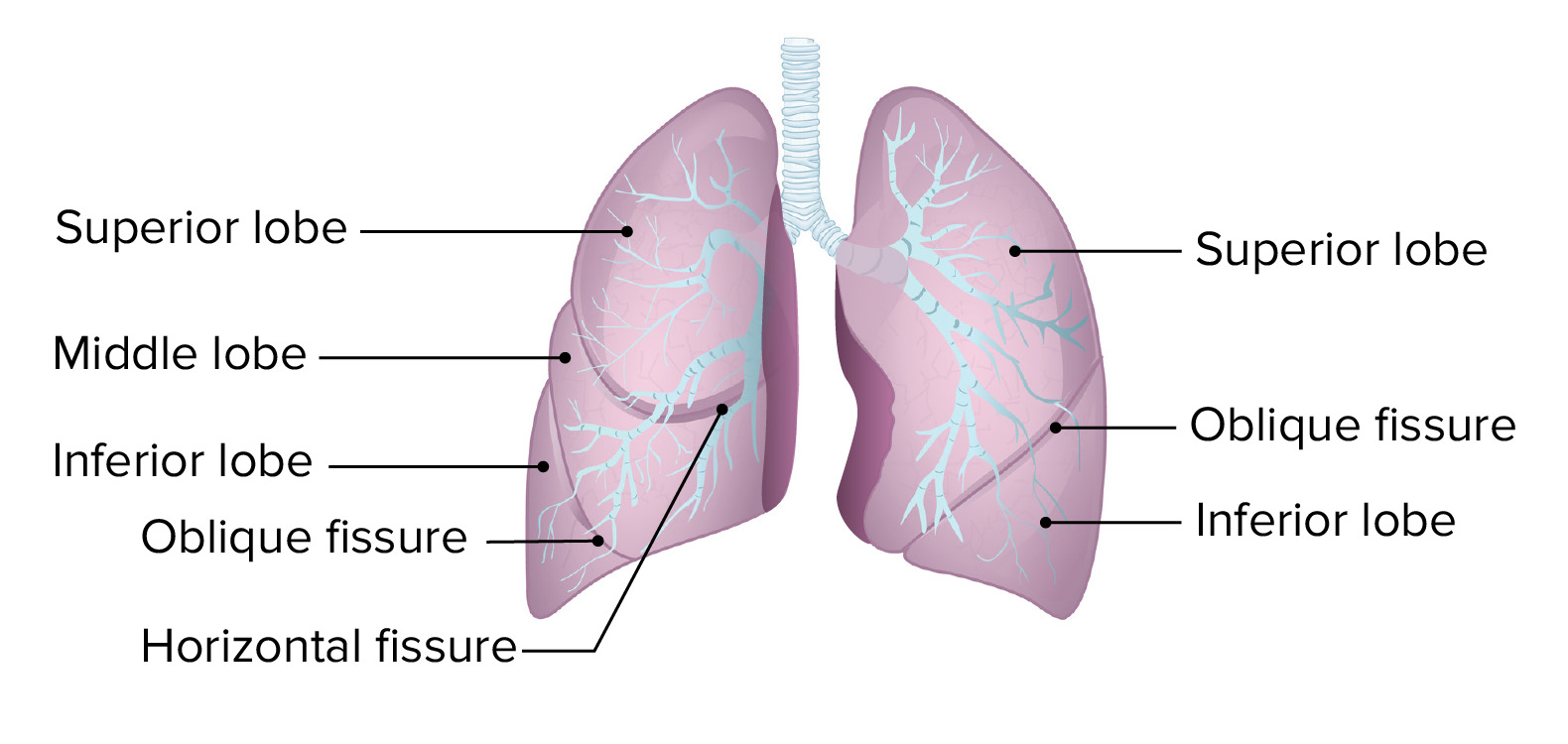
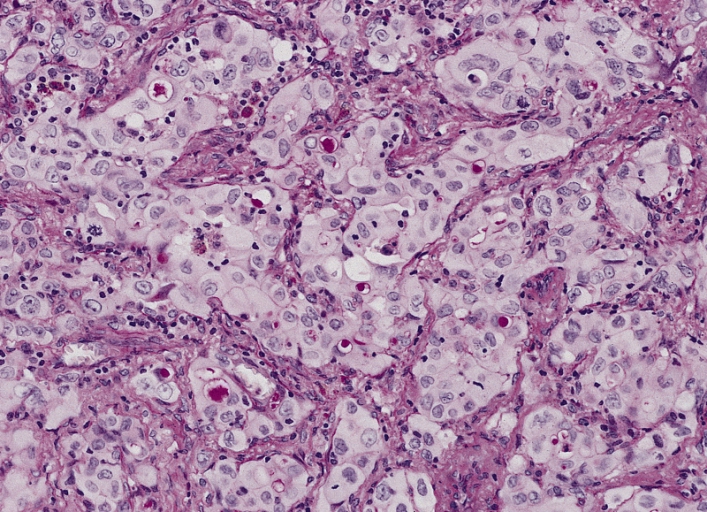
00:02 However, let's get into actual cancer. 00:05 The way that this is divided into clinical lung cancer is the following. 00:09 We'll take a look at our first family and this then includes our bronchogenic carcinoma. 00:14 Under bronchogenic carcinoma, the way that this is then worded, if you take up any, if you pick up any medical journal, New England, Lancet, whatever. 00:23 On the first few pages, often times, you have this huge plastered advertisements and it’s dealing with how to treat with what’s known as non-small cell lung cancer. 00:35 Why do they choose, and as we walk through here, things that you want to keep in mind, why do they choose on every single magazine to be talking about a non-small cell lung cancer? This is because lung cancer is the leading cause of mortality from cancer and the 6th leading cause of mortality overall, according to the World Health Organization. 00:54 Of all the lung cancers, it is one of the non-small cell lung cancer. 00:59 And what is that? Adenocarcinoma. 01:01 So, that’s where our focus shall be. 01:02 But before we get there though, a couple of things that you want to keep in mind as we go through. 01:06 Small cell lung cancer. 01:08 It’s also called oat, oat cell. 01:11 Location. 01:12 This is a primary lung cancer. 01:15 This means it will be one nodule first. 01:19 Understood? So, the fact that you found a solitary nodule in a previous discussion could be concerning because if it’s a primary lung cancer, it would be one nodule. 01:28 Now usually, if it’s benign in nature, it would then be, well, let's say within 3 cm. 01:34 Keep that in mind. 01:36 Now, where is this nodule located? If it’s a small cell lung cancer? Well, this would be by the mediastinum. 01:42 Hence we call this, take a look, pay attention, what is significant here is the word 'centrally located'. 01:49 And by centrally located, we mean that you will find on a chest X-ray (CXR) a primary nodule, one, dark calcific by the mediastinum. 02:00 That’s what’s meant by central. 02:03 Characteristics, there’s a bunch. 02:04 Let's walk through this. 02:06 First, let's get into our patients and then I’ll walk you through the verbiage, just like I’ve been doing. 02:11 Otherwise, I mean, what’s the point of me reading this to you, you could do that on your own. 02:14 So, the small cell lung cancer, say that your patient comes in, then they have a broomstick appearance of the extremities. 02:21 The arms, the extremities down by the legs. 02:26 They have truncal obesity, they have moon faceies. 02:28 Well, it kind of looks like you, Dr. Raj. 02:30 No, it’s not, I don’t have moon facies. Maybe I do. 02:33 But, I definitely, and I do have truncal obesity, I’ll give you that. 02:36 Broomstick appearance, oh, now, I’m kind of doubting myself, huh? What am I referring to? Good. Cushing’s syndrome. 02:42 What’s causing this Cushing’s syndrome in a patient that has small cell lung cancer? The hormone. 02:48 Is the lung cancer producing too much cortisol or is it producing too much ACTH? You tell me. 02:54 You stick to letter A. 02:56 ACTH, clear? Now you tell me two major places or origin or sources where ACTH would be produced in excess, resulting in excess cortisol. 03:10 Good. 03:10 One would be the anterior pituitary. 03:12 You call that Cushing a disease, right? And then second one would be the lung and this would be small cell lung cancer. 03:20 Now, if you want, I might want take a look at the A in small cell and use it to your advantage. 03:26 You have ACTH. 03:28 Let me give you another patient. 03:29 This patient is one in which, well, they’re not urinating a whole lot, they’re really not. 03:33 It’s not polyuria, it’s oliguria. 03:36 The urine that they are producing is extremely concentrated. 03:39 Maybe the urine osmolarity is up to 900. 03:44 Take a look at the plasma osmolarity and it’s at 250. 03:47 Diagnosis, SIADH. 03:51 Syndrome of inappropriate ADH. 03:54 ADH, another hormone that also begins with letter A. 03:59 So now you tell me a couple of places where ADH might be released in excess. 04:03 Good, maybe from the hypothalamus, maybe from the posterior pituitary, centrally, or maybe you’re releasing it paraneoplastically. 04:12 You see your patients, too much ADH, concentrated urine, plasma osmolarity decreased. 04:19 Move on. 04:20 What else might you find? Well, this is a patient in which, “Hey doc, when I wake up in the morning and I’m not feeling that great, I’m kind of tired and fatigued. 04:28 As the day progresses, I get stronger, get stronger, get stronger. 04:32 Wow, I feel great in the afternoon. 04:34 This is how I feel.” What am I referring to? This is Lambert-Eaton myasthenic syndrome. 04:40 Right? What is this? This is associated with small cell lung cancer. 04:45 It is an autoantibody disease, completely opposite of myasthenic syndrome. 04:51 So, myasthenia gravis is one in which your female patient, most likely. 04:57 She wakes up in the morning and what happens? She’s feeling good. 05:02 In Lambert-Eaton, you wake up in the morning and maybe not so good. 05:06 In myasthenia gravis, as the day progresses, maybe at noon time, she’s working in front of a computer and she can’t see too well because of the eye drooping. 05:15 And by 3 or 4 o’clock, she rolls around, she tells you, “I can barely get out of my chair.” Whereas with Lambert-Eaton, what happens? Do you have any problem with your acetylcholine receptors? In Lambert-Eaton, no. 05:29 Do you have any problem of acetylcholine supply? In Lambert-Eaton, no. 05:33 Where is my problem? The problem lies in the fact that you’re having a hard time releasing your acetylcholine at the neuromuscular junction, aren’t you? What is it that allows for acetylcholine to be released from the presynaptic terminal at the neuromuscular junction? Good. 05:49 That is your voltage-gated calcium channel. 05:51 You see that? So, your voltage-gated calcium channel are then being destroyed or targeted by the autoantibodies that may be produced paraneoplastically by small cell lung cancer. 06:02 Amazingly complicated, but once you get it all down, it all makes sense. 06:07 So, Dr. Raj, how is the individual getting stronger? If you can’t even release acetylcholine, you sure you know what you’re talking about? I do, trust me. 06:15 The body will find a way in which it will release the acetylcholine from the neuromuscular junction. 06:22 Once that acetylcholine comes out of the presynaptic terminal, it’s gonna cross the cleft. 06:27 Where does it bind to? Yes, it will continue. 06:29 It binds to acetylcholine receptors, open up the sodium channel, you have an amplified potential, end up hitting threshold, action potential, welcome to, increase contraction. 06:41 Let's move on. 06:42 What else might you have? Antibodies against neurons in Paraneoplastic myelitis. 06:48 Keep that in mind. 06:49 So, every once in a while, you might have issues with the nerves. 06:53 It’s called Paraneoplastic myelitis. 06:55 Maybe encephalitis. 06:57 There could be subacute cerebellar degeneration. 07:01 Amplification of MYC oncogenes, is the big one. 07:04 Management with chemotherapy, chemotherapy, chemotherapy and that then becomes your pharmacology. 07:09 So, small cell, a lot of stuff going on here in bronchogenic. 07:12 And then as I told you earlier, our next set of cancer we’ll take a look at will be non-small cell. 07:17 Histology becomes important for us. 07:20 We have neuroendocrine. 07:21 Lot of paraneoplastic. 07:22 Take a look at this. 07:23 Paraneoplastic myelitis, encephalitis. 07:26 So, whenever you have CNS issues within the cancer, you can expect there to be neuroendocrine. 07:31 Okay. 07:31 So, neoplasm, neuroendocrine, Kulchitsky cells appear – small dark blue cells. 07:39 Okay. 07:40 What else might you find? You want to be specific here. 07:43 By that I mean, neuron-specific enolase positive. 07:46 That’s important. 07:47 And you want to know chromogranin A. 07:49 And many of these you actually find in many of your neuroendocrine type of cancers, including carcinoids. 07:55 We’ll talk about that later. 07:57 Welcome to small cell. 07:59 Let's continue our discussion of bronchogenic carcinoma. 08:02 Now, we’ll take a look at non-small cell and these are the ones that are much more common as we go through this.
About the Lecture
The lecture Small Lung Cancer by Carlo Raj, MD is from the course Lung Cancer .
Included Quiz Questions
Which of the following paraneoplastic syndromes is LEAST likely to occur in small cell carcinoma of the lung?
- Hypercalcemia
- Subacute cerebellar degeneration
- Lambert Eaton
- SIADH
- Cushing’s syndrome
In a patient with small cell carcinoma complicated by a paraneoplastic syndrome of SIADH, which of the following lab results would you expect to find?
- High urine osmolarity
- Low urine osmolarity
- Polyuria
- Hypernatremia
- High serum osmolarity
Which of the following would you be LEAST likely to find on histology of a patient with small cell carcinoma?
- Mucin+
- Chromoganin A+
- Kulchitsky cell proliferation
- Neuro-specific enolase+
- Small dark blue cells
What is the typical management for small cell carcinoma of the lung?
- Chemotherapy with radiation
- Radiation alone
- Wedge resection
- Pneumonectomy
- Lobectomy
Customer reviews
4,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
1 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
The best teacher ever , wonderful lectures , it would be awesome that lecturio hired him again to do more lectures
Most videos by this speaker are too short sometimes cut in the middle. Also, too many repetitive nonsense statements.