Playlist
Show Playlist
Hide Playlist
Renin-Angiotensin-Aldosterone-System (RAAS) – Adrenal Cortex
-
Slides AdrenalCortex EndocrinePathology.pdf
-
Download Lecture Overview
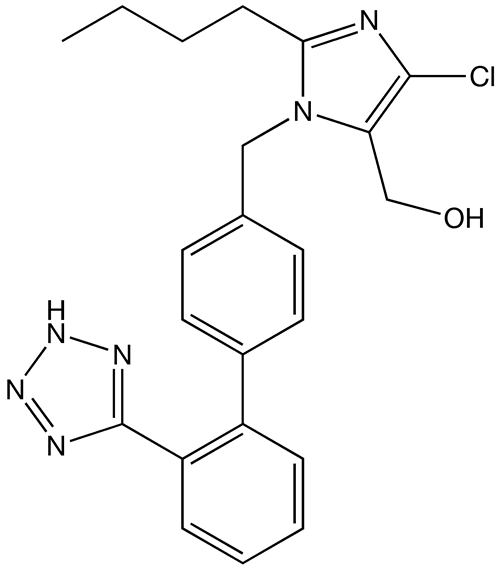
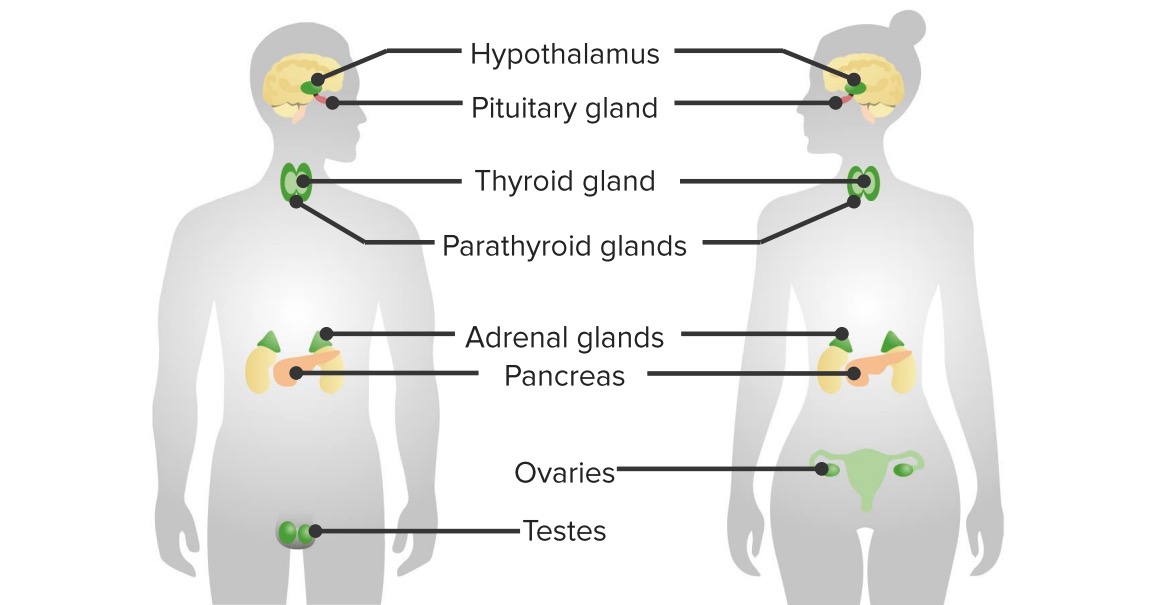
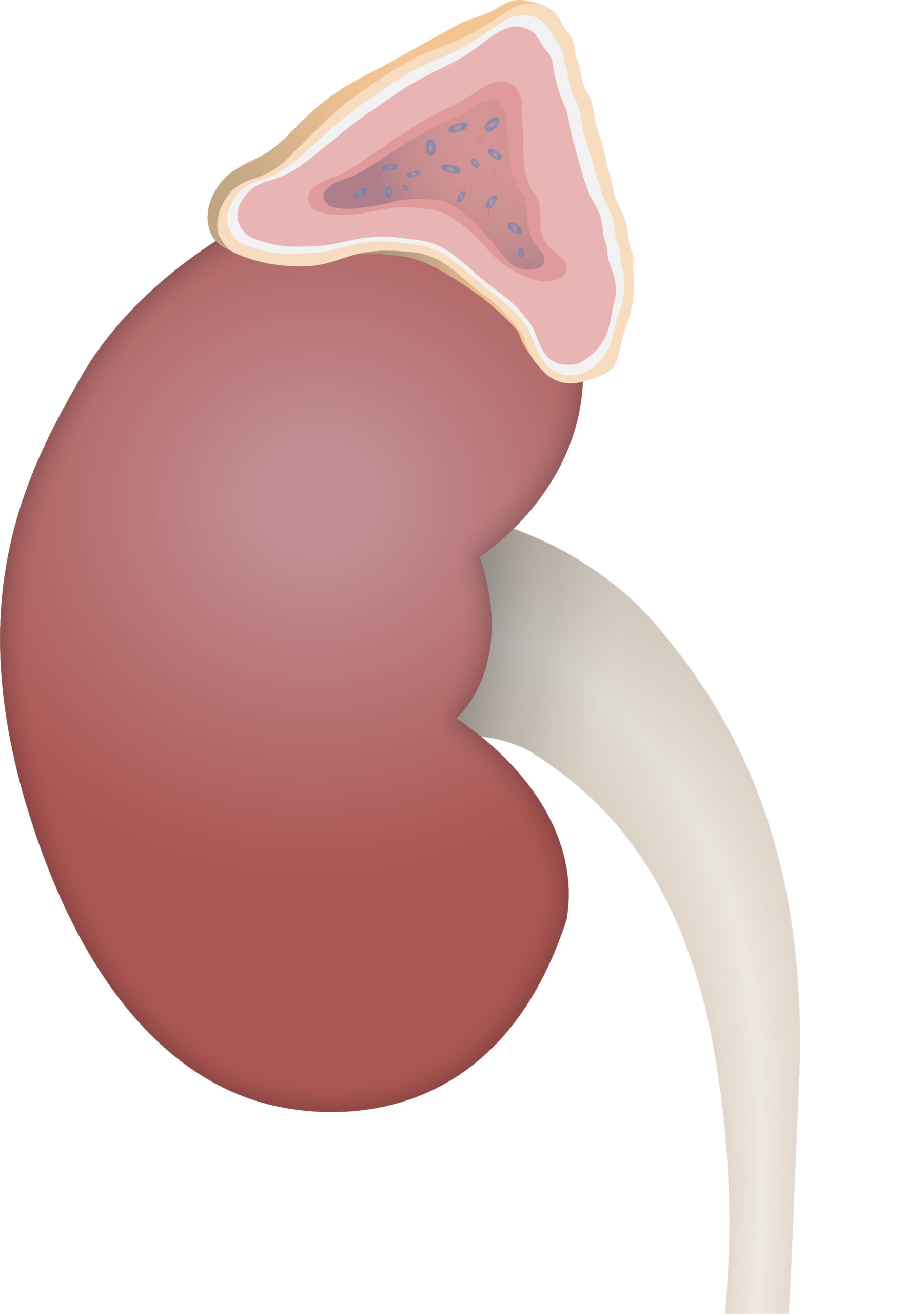
00:02 What about this RAAS system in aldosterone? Let’s quickly go through the steps here. 00:06 Let’s say that you have a patient who has decreased blood pressure. 00:11 Number one, if there’s decreased blood pressure taking place, then as far as profusion is concerned to the kidney in the afferent arteriole, it is depressed. 00:21 The juxtaglomerular cells via your beta-1 receptors will be releasing rennin, ah, out comes your renin. 00:27 The renin will then convert the angiotensinogen which is coming from the liver... remember ogen, ogen, ogen is a precursor. 00:34 Fibrinogen, angiotensinogen, trypsinogen, pepsinogen, those are all ogens. 00:39 This is angiotensinogen coming from the liver with the help of renin which behaves like an enzyme, you have your angiotensin I. 00:47 Next, what happens? What’s your… what is your objective here and why would you even want to have angiotensin II and why would you want to have aldosterone? Because your blood pressure is decreased, that is your inciting event, right? Now, the first reflex usually is going to be sympathetic tone, that’s a reflex that occur quickly. 01:08 The hormone, however, takes a little bit of time. 01:11 Also, the middle here that you see here, very important physiologic concept of a really quick feedback mechanism is called the MD cells, the macula densa cells that you’ve learned about in physio. 01:27 All of these amazingly will play a role so that it-it restores blood pressure back towards normal, right? If it’s macula densa, it’s a reflex mechanism and I’m just going to quickly tell you because there’s decreased blood pressure, you have decreased hydrostatic pressure over the glomeruli, therefore decreased filtration, decreased delivery of sodium to the macula densa cells and therefore, what does it want to do with the afferent arteriole to then increase the GFR, the glomerular filtration rate? It wants to vasodilate. 02:03 If you’re unfamiliar with that then please refer back to physio and make sure that you know what’s known as a tubuloglomerular feedback… quite important, quite important. 02:13 In the meantime, let’s continue. 02:15 Angiotensin I with the help of ACE which stands for angiotensin-converting enzyme is then releasing angiotensin II and you tell me. 02:24 Our discussion here, angiotensin II stimulates what enzyme? Aldosterone synthase. 02:30 We have our aldosterone, what are we trying to do? Restore blood pressure back towards normal. 02:35 Hence, it will reabsorb sodium and water. 02:38 In the meantime, do not forget about a little pharmacologic side effect, huh? This is known as ACE inhibitors. 02:48 At any point in time, if you wish to give an ACE inhibitor, which is normally responsible for breaking down your bradykinin; if you gave an ACE inhibitor, bradykinin will be elevated, your patient is now complaining of ugh, ugh, ugh… dry cough. 03:06 Angiotensin II, in addition, remember your patient has decreased blood pressure; angiotensin II overall is a potent, potent vasoconstrictor. 03:18 If you vasoconstrict an arteriole, you’re increasing your TPR in the hope of increasing blood pressure. 03:24 A simple physiology question is the following. 03:26 If you inhibit angiotensin II, the vasoconstriction has been lifted vascular and you drop your after load increasing your cardiac output... a simple physiology question in the formal form. 03:38 Down the kidney… afferent/efferent arteriole, angiotensin II prefers to work-prefers to work at normal levels at the efferent arteriole. 03:50 Remember, when you have decreased blood pressure, what happened to profusion in the kidney? Oh, it decreased, you have decreased filtration. 03:57 Wouldn’t you want to constrict the efferent arteriole? Think about that, are you there? The efferent arteriole… if this is my-if this is my glomerulus and this here is my efferent arteriole, if you constrict this, what then happens to your hydrostatic pressure? It increases. 04:13 Take a look at filtration fraction. 04:15 Remember this from physio… what’s filtration fraction mean to you? It’s GFR over RPF, right? Please make sure you commit that to memory, if you haven’t already. 04:26 It’s GFR over RPF. 04:29 If you constrict the efferent arteriole, what happens to renal plasma flow? Take your time… decreases. 04:36 Where is the RPF in the ratio? In the denominator, so that’s decreased. 04:42 If you constrict the efferent, what happens to hydrostatic pressure approximately? It increases. 04:48 What happens to GFR with efferent vasoconstriction? Oh, it increases. 04:52 Now, this part, I can’t help you, this is simple math. 04:55 If you increase the numerator and decrease the denominator, what happens to filtration fraction? Obviously increases, there you have it. 05:04 Let’s continue. 05:05 Aldosterone works where? Collecting duct, principal cells. 05:09 It works to do everything in its power to reabsorb-reabsorb sodium. 05:14 On your boards, you can either work on the sodium potassium pump on the basolateral membrane or can work on the epithelial sodium channel on the luminal membrane. 05:23 Either case, you’re reabsorbing sodium along with that out comes the water in the hopes of doing what? Once again, increasing blood pressure. 05:32 Now, you’re reabsorbing sodium, keep it simple. 05:37 Aldosterone wishes to get rid of two elements into the urine. 05:42 It will get rid of potassium, it will get rid of hydrogen. 05:47 Any condition in which there’s an increase in aldosterone, you will then find hypokalaemia, increased blood pressure and your pH is increased. 05:58 Why? Because you’re getting rid of hydrogen… alkalosis. 06:01 Be careful, be able to do that quickly. 06:05 Create a favourable sodium gradient for sodium and water reabsorption. 06:11 In addition, if you have decreased blood pressure, that angiotensin II will do everything in its power to restore blood pressure including stimulating the posterior pituitary to release your ADH. 06:25 ADH, as you know, will work upon your V2 receptors, it will then open up the aquaporins, reabsorb your water. 06:33 In addition, you increase your proximal convoluted tubule… your proximal tubule… sodium reabsorption. 06:39 Once again, you’re trying to increase your blood pressure. 06:45 This is what something that’s called can permit contraction alkalosis. 06:49 What that means is the following. 06:51 Water reabsorption can permit contraction alkalosis, meaning to say that you would have increased proximal tubule sodium reabsorption, you get rid of your hydrogen and may result in contraction alkalosis. 07:04 Stimulates the hypothalamus for thirst, once again all… you begin with your inciting event being decreased blood pressure. 07:13 Be able to go through this in great detail and you should be able to answer any angle of patho-physiology that they might ask you. 07:22 Angiotensin II affects baroreceptor function, limit reflex bradycardia. 07:27 ANP, atrial natriuretic peptide. 07:28 What does it do? Well, if it works in the atrial in response to increase in volume, it will do everything in its power so that it checks the amount renin-angiotensin aldosterone, so check and balance, check and balance. 07:46 If there’s too much fluid retention, ANP will be released… atrial natriuretic peptide. 07:53 Later on, well, in cardiovascular, we’ve talked about a very important marker known as BNP and that becomes important too in a patient with congestive heart failure. 08:02 This is ANP, atrial natriuretic peptide and it will then increase your GFR. 08:10 If anything, it will cause vasodilation, relaxes vascular muscle via cyclic GMP. 08:20 ADH also will regulate volume and if there’s decreased blood pressure and if it’s significant enough, not only will you have your aldosterone but you’ll also have ADH and this would then reabsorb your water. 08:38 Aldosterone, we’ve talked about in great detail. 08:43 Low blood volume is prioritized at all costs. 08:46 That’s an important point. 08:48 I expect you to know from physio that if you’re losing enough blood… so, you have a patient that gets into an accident or gets into a knife fight, huh, and gets lacerated so badly that they’re losing massive amount of blood, there it is on the floor and it keeps leaking, leaking, leaking. 09:07 At that point, what becomes more important, osmolality or volume? Volume. 09:12 So, the body will do everything in its power, right? This is hypovolemic shock. 09:19 Everything in its power to make sure that it’s restoring the volume, restoring the blood pressure, otherwise your patient’s dead. 09:26 Hence, you have these hormones such as aldosterone and ADH that will play a major role.
About the Lecture
The lecture Renin-Angiotensin-Aldosterone-System (RAAS) – Adrenal Cortex by Carlo Raj, MD is from the course Adrenal Gland Disorders.
Included Quiz Questions
Where are renin and angiotensinogen produced, respectively?
- Kidneys and liver
- Lungs and liver
- Liver for both
- Kidneys and lungs
- Kidneys and heart
What is the function of angiotensin II?
- Vasoconstriction and increasing blood pressure
- Breakdown in bradykinin
- Conversion of angiotensinogen into angiotensin II
- Decreased GFR
- Decreased SVR
What is the result of the constriction of the efferent arterioles by angiotensin II?
- Increased filtration fraction
- Decreased GFR
- Decreased BP
- Increased sodium retention
- Decreased plasma volume
What is NOT an effect of aldosterone?
- It decreases H+ channels in intercalated cells.
- It increases K+ excretion.
- It increases H+ excretion.
- It increases Na+ channels.
- It increases the activity of the Na+/K+ pump in principle cells.
What molecule is released from the atria in response to increased fluid volume?
- ANP
- ADH
- Aldosterone
- Angiotensin II
- Renin
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |