Playlist
Show Playlist
Hide Playlist
Shock in Children
-
Slides Shock Pediatrics.pdf
-
Download Lecture Overview
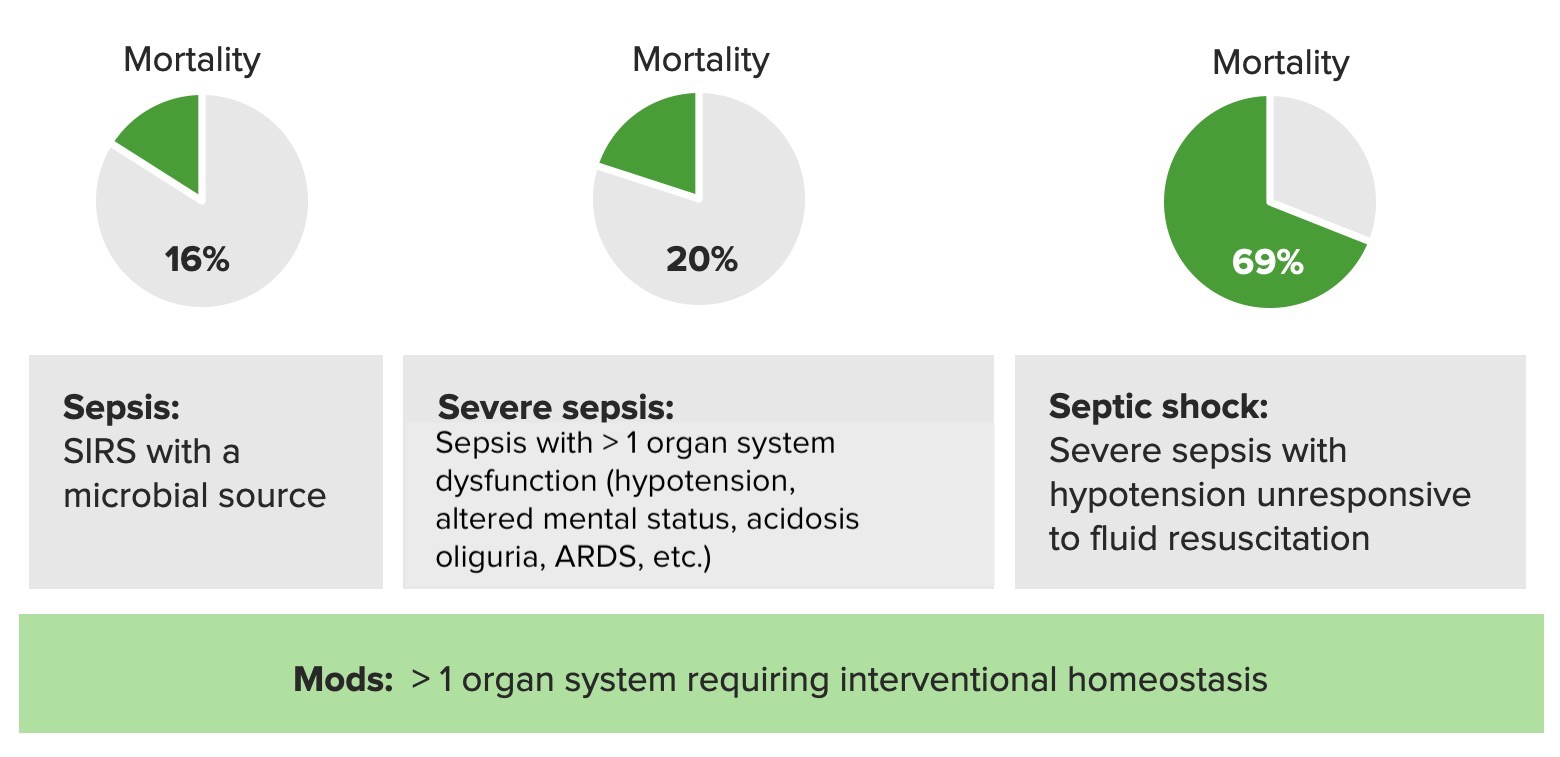
00:01 In this lecture, we’ll review types of shock in children and causes of shock in children. 00:07 First, let’s define shock. 00:08 Shock is defined as an inadequate delivery of oxygen and substrate to meet metabolic demand of tissues. 00:16 We generally break it down into two types, compensated and uncompensated. 00:21 Compensated shock usually happens early in the situation that’s the causing the shock. 00:26 Generally, the blood pressure is still normal. 00:28 So the body is capable of accommodating the lower pressures systemically by raising the heart rate. 00:36 Uncompensated shock happens later. 00:39 This is when now the blood pressure is lower and we can start to see end-organ damage. 00:46 So there are generally four different categories of shock and we’ll go through them. 00:51 Hypovolemic shock typically happens when there’s not enough blood volume. 00:55 This can happen with acute dehydration, fluid loss such as diabetes insipidus, bleeding or third spacing, when the fluid is there but it’s all come out of the blood vessel. 01:09 The next is distributive or vasodilation. 01:13 So distributive shock typically happens in patients who have sepsis or when the have injury to their spine, they can have a neurogenic shock. 01:22 Or they may have anaphylaxis as a reaction to an exposure and then they get vasodilation. 01:31 Cardiogenic shock is when the heart is primarily involved. 01:35 This can happen for example in patients with a bad cardiomyopathy or in patients with arrhythmias. 01:42 And last, obstructive shock is when the heart’s working, it just can’t get the blood out. 01:47 So examples would be tamponade, pulmonary embolism or maybe a tension pneumothorax. 01:53 So those are the general types of shock. 01:57 So let’s talk about how we approach patients in shock. 02:01 Well, we often will see fever in septic shock. 02:05 A heart rate will generally be tachycardic, although maybe bradycardic in newborns. 02:11 The blood pressure was going to be low and, of course, in compensated shock, it will be normal. 02:17 The respiratory rate is often increased. 02:20 This may be to blow off carbon dioxide to correct for any metabolic acidosis. 02:26 Remember, underperfusion can result in a lactic acidosis and that acidosis will then be accommodated for by blowing off extra carbon dioxide. 02:36 Patients may have altered mental status if there’s end-organ damage to the brain and they may have a delayed capillary refill on exam and we can see this typically. 02:47 Also we can see decreased peripheral pulses, although cap refill is usually your first bet. 02:53 If you’re assessing cap refill, remember that nails is a fine place to look, but if they have cold extremities, that will be an inaccurate assessment. 03:01 So you should assess it somewhere centrally, like over the glabella. 03:05 You just press and release and count the seconds. 03:09 So if we see a patient in shock, we of course need the clinical context. 03:15 And we need to know whether this is a patient who is febrile and has a pneumonia or whether this is a patient who just got hit by a car and is bleeding out of their leg. 03:23 But whatever the clinical context is there’s a few labs we should think about. 03:28 The first is the Chem-7 and the blood gas. 03:31 So we get these labs emergently, partially because we can see some very important things in them that can allow us to make decisions about care. 03:41 So the first is the Chem-7 will show sodium abnormalities, which is classic in patients with severe dehydration. 03:48 They can either have a hyper or a hyponatremia, so that sodium’s important. 03:53 Potassium anomalies may cause a cardiac arrhythmia, so certainly in a patient where you’re worried about the potentiality of a high potassium or a low – very, very low – potassium, you might get a potassium. 04:07 The acidosis generally reveals a diagnosis of metabolic acidosis and will also allow you to somewhat assess the respiratory ability to compensate by getting the blood gas as well. 04:21 So if a patient has a low carbon dioxide, but is still acidotic, it implies they’re trying to compensate for their metabolic acidosis. 04:30 If the BUN and the creatinine are elevated, both in prerenal hypovolemia, so a patient is just very dry, or in intrarenal end-organ damage. 04:42 Typically, in a patient with pre-renal hypovolemia, mostly the BUN will go up, the creatinine will stay relatively normal. 04:51 However, in intra-renal end-organ damage, you’ll see both levels go up. 04:55 So you can start to distinguish between those two. 04:59 So what else do we get in a patient with shock? Well, if it’s severe shock and we’re worried about assessing end-organ damage, getting the liver function test is important because we usually see a bump in the ALT and the AST as a result of end-organ hypoperfusion of the liver. 05:17 Likewise, an EKG and an echo may be important for identifying causes of cardiogenic shock. 05:24 And the chest X-ray may be valuable if you’re worried about an obstructive shock because it would show for example a large mediastinum and a large heart for a pericardial effusion or it could show you your tension pneumothorax. 05:38 Although hopefully for tension pneumo, you’ve picked that up clinically before you’re getting a chest X-ray.
About the Lecture
The lecture Shock in Children by Brian Alverson, MD is from the course Pediatric Emergency Medicine.
Included Quiz Questions
Which of the following is a cause of obstructive shock?
- Pulmonary embolism
- A splenic laceration
- Ventricular tachycardia
- Anaphylaxis to a bee sting
- Meningococcemia resulting in hypotension
Which of the following best defines shock?
- Tissue hypoxia
- Low blood pressure
- Low intravascular volume
- Inadequate tissue perfusion
- Organ dysfunction
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Good lecture! Maybe it should have been longer. Also, can't peripheral pulses get buldgy?