Playlist
Show Playlist
Hide Playlist
Normocytic Anemia: Overview
-
Slides Normocytic Anemia Overview.pdf
-
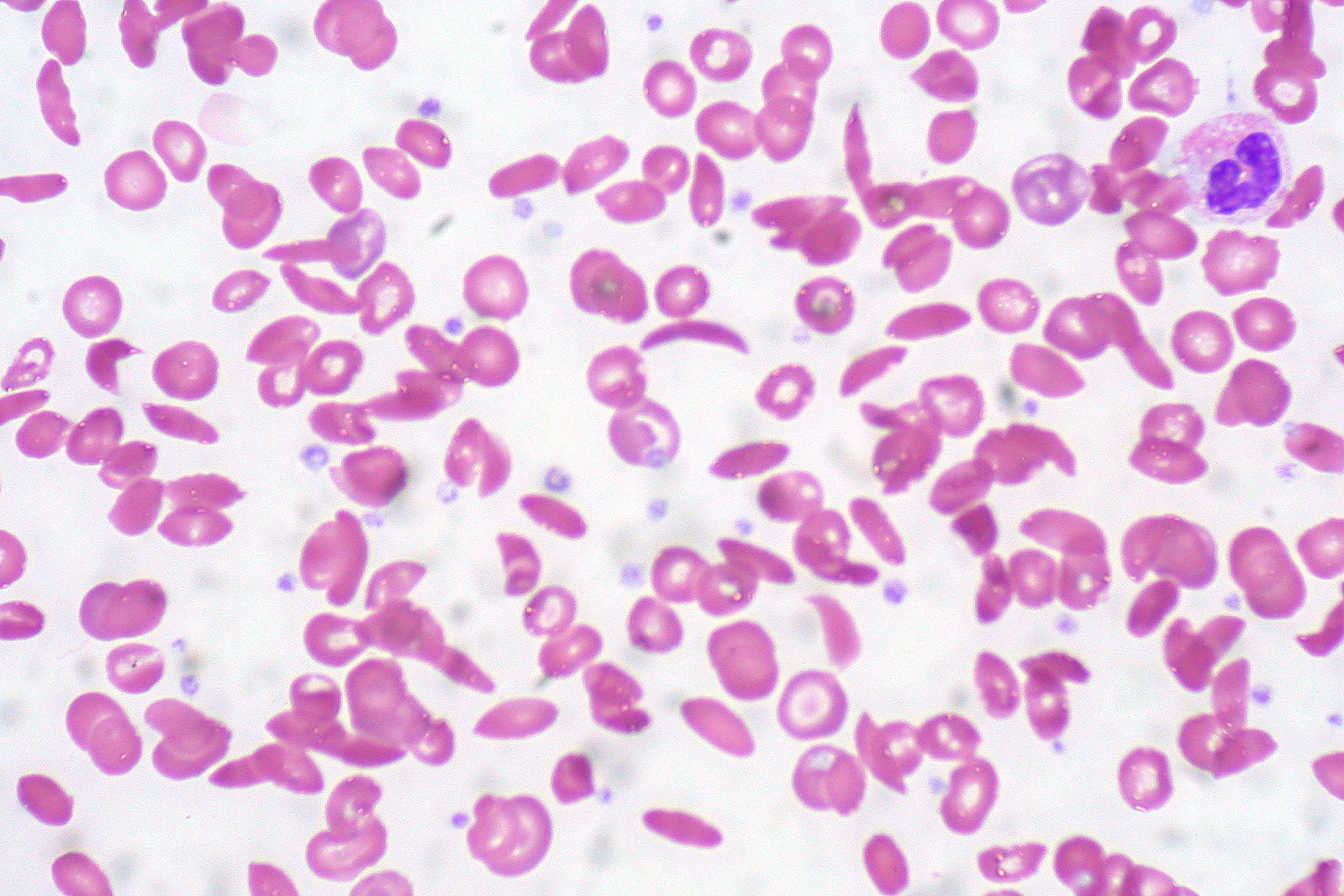
Download Lecture Overview
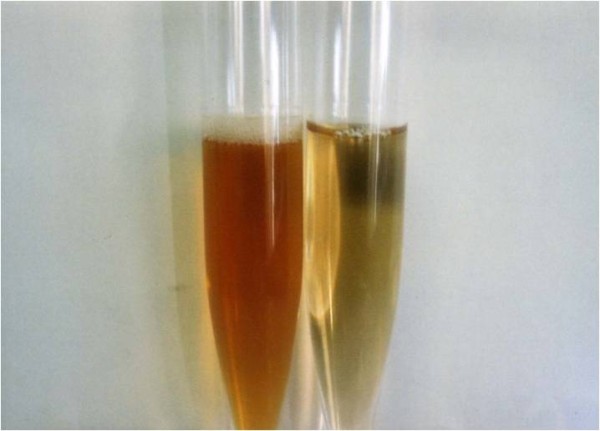
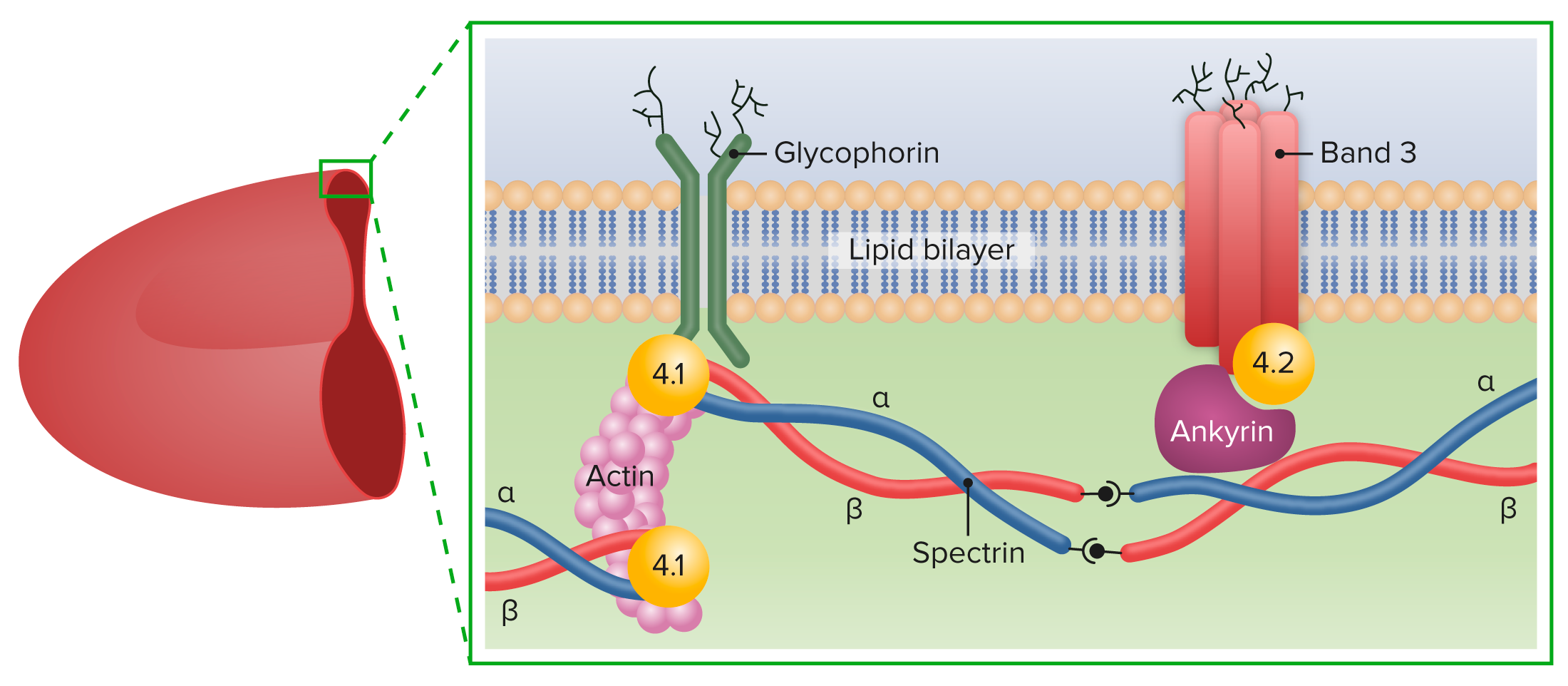
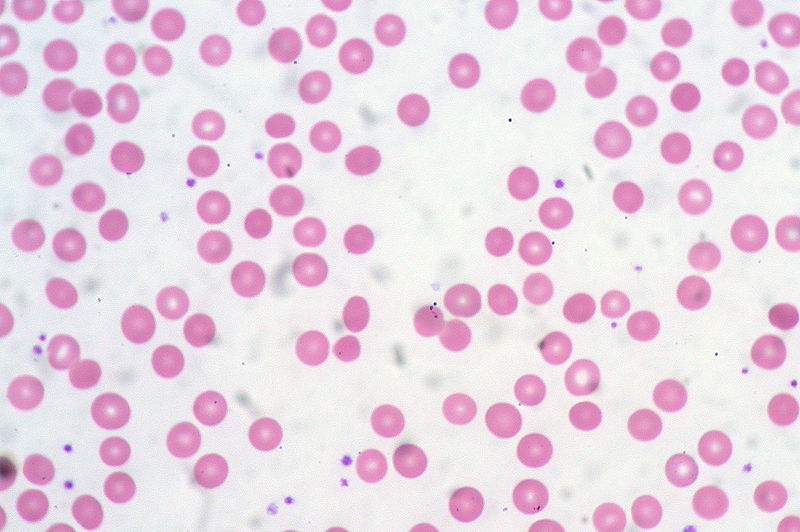
00:01 Students tend to have a hard time with normocytic anemia only because of the organization. 00:07 So it’s exactly what we will focus upon initially with the overview. 00:13 This will be the largest category of anemias. 00:16 Here, the MCV will, in fact, be between 80-100, perfectly normal. 00:21 Next, what do you do once you have a patient who gives you the symptoms of each of one of these diseases that we will go through and the MCV has 80-100. 00:31 Well, next you check to see as to whether or not the bone marrow in fact is working properly. 00:37 How do you know? Well the bone marrow if it’s working properly and the RBCs are being destroyed quickly or there is massive hemolysis, either through intra or extravascular hemolysis, now, please understand the bone marrow is going to do what? Churn, churn, churn more reticulocytes into circulation. 00:58 So therefore, in clinical practice, we call this reticulocyte production index or RPI. 01:04 For you, you want to know RPI, so be it, but it’s equivalent to the concept of increasing reticulocyte. 01:11 So therefore, the two on the right that you’re looking at here, the magic number is a corrected reticulocyte being greater than 3%. 01:19 All it means is that the RBCs are being destroyed either within the vasculature, intra or extravasculature mainly the spleen in which now the bone marrow is increasing or compensating and increasing the production of reticulocytes, concept number 1. Concept number 2 will do the opposite. 01:40 What if you have a condition in which the bone marrow has been shut down? Such as, well, maybe your patient was taking chemotherapy. 01:46 Maybe chloramphenicol, maybe there is a concomitant infection parvovirus B19. 01:52 If that is the case, your bone marrow, in fact, is being shut down. 01:55 And so therefore, how in the world could the bone marrow produce any reticulocytes? It does not. 02:00 And so therefore, you would have a decreased RPI or reticulocyte production index. 02:06 And here, the magic number is corrected reticulocyte count of less than 3%. 02:11 These are concept that you want to make sure that you have down. 02:13 Now, one little thing that I want to point to you before we move on is that couple of anemias can occur at the same time. 02:22 For example, coming off the discussion of both microcytic and macrocytic anemias, Well, the microscopic anemia that you might be thinking about being, well, quite common, is iron deficiency. 02:35 And if you have a type of intravascular hemolysis, then you’re going to then release hemoglobin into the urine along with the hemoglobin there goes the iron, doesn't it? So you might have concomitant iron deficiency as well. 02:49 Now, which one of these is hemolytic or non-hemolytic that may result in reticulocytosis? Good, the hemolytic. 02:57 RBCs are dying and as they do so, well, the bone marrow is now churning out increase amounts of reticulocytes. 03:04 And therefore, we have reticulocytosis. 03:07 Would you give me the size of reticulocyte when compared to a mature RBC? It is larger. 03:13 So what is that going to give you with MCV? Greater than 100, every possibility that you might have a nonmegaloblastic macrocytic anemia with reticulocytosis. 03:25 Are we seeing this at this point? Let’s continue to the overview. 03:29 Now continuing from the previous slide, on your left, you will notice that your reticulocytosis is not increased, magic number less than 3% for corrected. 03:40 And if you take a look at the differentials, I will give you the ones that were obvious here. 03:44 We have aplastic anemia due to many, many reasons, viruses, chemotherapy, chloramphenicol or renal disease if the kidneys are dead then you do not have EPO or erythropoietin and so therefore, who's not functioning properly? Good. 04:00 The bone marrow. 04:02 And then, let's say that you had malignancy such as breast cancer. 04:05 And if it's breast cancer, then there is every possibility that it might then metastasize into your bone marrow, therefore really impeding the development of an RBC. 04:17 So you can see here clearly that your patient is in fact suffering from anemia, but the bone marrow might be shut down or is not working properly. 04:25 And so therefore, is going to present with normocytic non-hemolytic type of anemia. 04:30 Now in addition to that, we’ll walk through in greater detail the blood loss being acute, less than 1 week. 04:37 And what that means, is that when you’re having blood loss, it’s whole blood and so therefore, you’re losing RBCs and you’re losing your plasma. 04:45 So therefore, in terms of the symptoms might be there obviously. 04:49 But in terms of actually looking at the anemia and the MCV, it will be perfectly normal. 04:57 Less than 1 week becomes very important for us and you’ll see why. 05:00 And the early stage of both anemia of chronic disease and iron deficiency could be normocytic. 05:08 So early on, but interesting enough, the anemia of chronic disease, normocytic will perhaps even persist even into the long run. 05:18 So remember I told you about -- Can you think of anemia of chronic disease? Last time we talked about that was chronicity, chronicity, chronicity. 05:25 You have that acute phase reactant known as hepcidin which then blocks release of your iron from your ferritin. 05:31 So that is going to be non-hemolytic. 05:33 Under hemolysis and hemolytic, well -- here both take a look at your reticulocytosis, increased. 05:40 Magic number corrected reticulocyte greater than 3%. 05:42 And what you will do next, if you want, is maybe divide this into intrinsic and extrinsic, but I can assure you that is not really going to give you clinical features. 05:55 What question that you need to ask yourself that truly gives you the clinical features for all hemolytic anemias, both intrinsic and extrinsic and I’ll give you the definition later is whether or not this hemolysis was intravascular or extravascular. 06:12 Let me give you one big intravascular type of hemolysis. 06:17 If you go under membrane and actually, what you might want to do here is maybe create a mnemonic called MAD. 06:25 MAD. 06:27 M is membrane defect hemolysis. 06:30 A is abnormal hemoglobins. 06:33 And D is deficiency of enzymes. 06:36 And we’ll go through each and every single one of these as we then peruse through our various types of pathologies. 06:42 But I told I will give you one major intravascular hemolysis here. 06:46 This is PNH, paroxysmal nocturnal hemoglobinuria. 06:50 And pretty much, the name tells that it’s intravascular. 06:54 Whenever -- you tell me, where is hemoglobin supposed to go normally for its complete metabolism and destruction? To the spleen, right? And so therefore, the heme will then be further broken down to biliverdin and then your indirect unconjugated bilirubin and the globin will then be recycled. 07:11 We can’t breakdown globin. 07:12 That’s your genes. 07:14 So that would have to be spleen So how is it that you end up hemoglobinuria? If the blood vessel then destroys your RBC intravascular, your blood vessel normally cannot metabolize your hemoglobin all the way down into your indirect bilirubin. 07:31 So therefore, you’re going to have quite a bit of hemoglobin that is being released into circulation. 07:36 Are you with me? Are you picturing this? This hemoglobin is then going to be delivered to the glomerulus where it then passes through, welcome to red urine or hemoglobinuria, intravascular. 07:46 What if it was external or extravascular? If it is extravascular hemolysis, I am going to give you the prototype here under abnormal hemoglobin. 07:54 Not to mention, we’re going to go to a little bit more detail with hemoglobin C as well. 07:58 We have to. 07:59 But sickle disease, is that homo or heterozygous type of pattern? Good, it’s homozygous. 08:07 Homozygous is always more dangerous. 08:09 So let’s say that you have an African-American child who has sickle cell disease. 08:14 And well you know the symptoms like acute chest pain, maybe there is going to be difficulty with vision, maybe dactylitis, so on and so forth. 08:22 And if you take a look at the eyes, well you'll find icterus, icterus. 08:26 What is icterus and perhaps yellowing of the skin? That’s jaundice, isn’t it? All of this is -- What kind of substance is this? This is indirect unconjugated bilirubin. 08:40 So sickle cell disease, you would know that upon exertion of the child, exercising or whatever, that now, all of a sudden, the RBC becomes sickled. 08:50 Really bad, right? Sickled, gets polymerized is what it's called. 08:53 And when it becomes sickled, then it’s taken to the spleen, splenomegaly. 08:58 Welcome to extravascular. 09:00 The spleen is then going to remove the RBCs out of the vasculature and then it will further break things down. 09:06 And welcome to significant jaundice. 09:09 The question that you want to ask yourself, on the right side, for intrinsic and extrinsic, more importantly is is my disease intravascular or is my disease extravascular? And we’ll go through the details as to membrane, abnormal hemoglobin and deficiency of enzyme and then we’ll walk through the extrinsic part where it includes our micro and macroangiopathic type of hemolytic anemia. 09:33 So those become important for us.
About the Lecture
The lecture Normocytic Anemia: Overview by Carlo Raj, MD is from the course Normocytic Anemia – Red Blood Cell Pathology (RBC).
Included Quiz Questions
Which of the following is the most likely etiology in a patient with normocytic anemia and a corrected reticulocyte count of 2%?
- Chloramphenicol use
- Glucose-6-phosphate dehydrogenase deficiency
- Immune hemolytic anemia
- Pyruvate kinase deficiency
- Sickle cell disease
Which of the following conditions is mainly an intravascular type of hemolytic anemia?
- Paroxysmal nocturnal hemolysis
- Autoimmune hemolytic anemia
- Hereditary spherocytosis
- Beta thalassemia
- Aplastic anemia
All of the following types of anemia result from an intrinsic erythrocyte defect EXCEPT which of the following?
- Microangiopathic hemolytic anemia
- Hereditary spherocytosis
- Glucose-6-phosphate dehydrogenase deficiency
- Sickle cell disease
- Paroxysmal nocturnal hemoglobinuria
Hemoglobinuria is mainly a feature of which of the following types of anemia?
- Intravascular hemolytic anemias
- Sideroblastic anemias
- Aplastic anemias
- All hemolytic anemias
- Extravascular hemolytic anemias
Extravascular hemolysis mainly takes place in which of the following organs/tissues?
- Spleen
- Blood
- Bone marrow
- Lymph nodes
- Thymus
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Great way of teaching and easy to remember superbly organised lecture series.