Playlist
Show Playlist
Hide Playlist
Normal Hemostasis
-
Slides NormalHemostasis.pdf
-
Download Lecture Overview
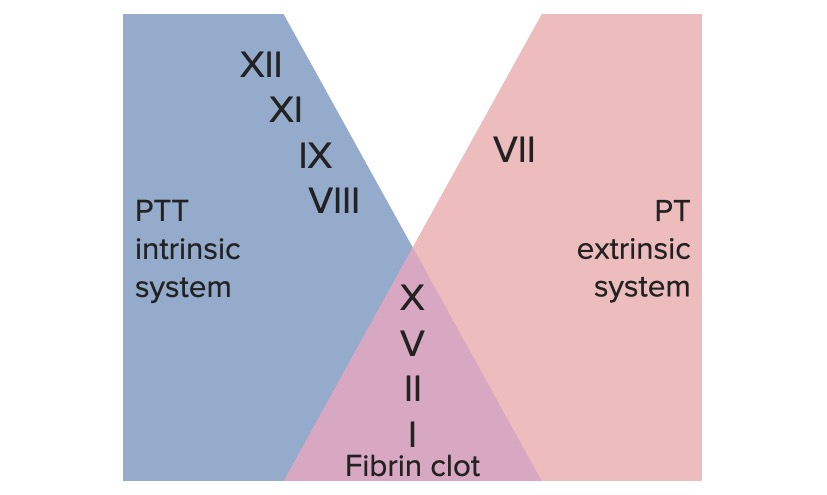
00:01 Hi there. My name is Dr. Raj. 00:03 And let's take a look at what happens when you have damaged taking place within your blood vessel. 00:09 The process called hemostasis. 00:12 The primary cell responsible for hemostasis would be which we've seeing here. 00:19 Now, what are you seeing here? Let's take a look at the arrows. Those are your platelets. 00:22 Would you be able to tell me as to what the normal count of a platelets are? At least 150,000 to maybe approximately 400,000 that's a lot of platelets that we have circulating. 00:35 And therefore, this picture here is a peripheral blood smear. 00:39 If you were to take a look at platelet before it matured that would be way back in the bone marrow. 00:46 So, what we're not seeing here is a bone marrow aspirate, and you can tell because around the platelet the cells that you seeing their are your RBC's notice a central pallor, right? Normal. 00:59 There's a peripheral blood smear of your platelet. 01:02 So that baby or immature platelet way back in the bone marrow is then known as your megakaryocytes and one of the things that you need to know at your point in medical education is being able to identify a megakaryocyte in your bone marrow. 01:16 Now, why is it important that we have to have so many platelets? The weakest point in you and I right now is that the junction between this picture. 01:24 Between the capillary and the venule. 01:27 So, as blood is moving from the capillary into the venule at that junction, it's the weakest point. We need to make sure that at all times we have enough platelets so that we fill up that particular hole. 01:39 That you and I normally. 01:41 But what happen if the cells of a blood vessel known as your endothelial cells were to then get injured? When does endothelial cells become injured? Due to -- you and I right now, maybe a blood pressure rise a little bit. 01:57 Maybe we bump our arms into something or maybe you listen to me, got bored, you fell asleep and you fell off your chair. 02:02 And then, you cause damage to your endothelial cell. 02:06 When you do, you're then going to express a particular ligand from the sub-endothelial collagen. Remind me what that collagen is made up of. 02:15 Collagen making up your basement membrane, is of the type 4 type. 02:20 It is done expressing a particular ligand called Von Willebrand factor. There you go. 02:25 And what does that Von Willebrand factor going to bind to? Well, that'll come up next. 02:30 What I'm gonna show you is a picture of where we're headed. 02:33 And then, we'll go into details. 02:35 And then, as you shall see, we're gonna make this clot stronger, and stronger, and stronger. 02:41 You notice, this is a temporary hemostatic plug. 02:46 You'll notice at the very bottom. 02:49 I want you to have this picture in your head as we move through the next few discussions. 02:55 The very bottom here is your Von Willebrand factor. You see that? Huh, that Von Willebrand factor was being expressed by the sub-endothelial collagen. 03:04 How did that happen? The endothelial cells then became damaged, didn't they? How? Maybe hypertension, smoking, what have you. 03:11 When does endothelial cells become damaged? Express Von Willebrand factor, and then Von Willebrand factor as you see here as to then bind to receptor. 03:21 The receptor that you're seeing that it binds to is then called glycoprotein 1B. 03:27 Well, all of this is of course a central point of all this would be then your platelet. 03:32 At this point, the only, only hemostatic factor that we brought in is your platelet. 03:38 It is not your clotting factors yet or your coagulation cascade factors. 03:44 I will tell you when we will transition from our platelet plug, which is temporary here. 03:50 In which we will then notice -- you see the beads, called fibrinogen. 03:56 What is the suffix -ogen mean to you? It means weak. You've heard of trypsinogen. You've heard of pepsinogen. 04:03 You've heard of angiotensinogen. 04:06 In order for something to become strong, what has to happen? Oh, the -ogen has to be cleaved. 04:11 And once the -ogen has been cleaved, it becomes strong. 04:14 But at this point, notice, we're only in the form of fibrinogen. 04:17 So therefore, this is a weak temporary hemostatic plug, but yet we did form a plug. 04:25 Now, subsequently now, we'll have discussions about how to split, it gets activated. 04:31 And then, it'll aggregate, and as we move further, we will then take the fibrinogen and you should already be thinking of the "enzyme" that cleaves off your -ogen, which is then called? You got this. What is it? Thrombin, at that point we'll get into our coagulation cascade. 04:54 Let's go ahead, and activate that platelet, shall we. 04:58 Now, that platelet will get activated. 05:00 There's a particular receptor on that platelet, it's called P2Y12, P2Y12. 05:08 When that P2Y12 receptor gets activated, you have a dense granule within your platelet. 05:16 That dense granule is then going to release ADP. 05:19 And all that platelet then gets activated and then inside the platelet, you have a particular arachidonic acid metabolite, called thromboxane, TXA2. 05:30 And thromboxane, obviously is going to take the platelet and it will help you or facilitate further aggregation. 05:37 In the meantime, remember, all of this is hemostasis. 05:41 In other words, what are we trying to do? Well, let's say that you gotta a big picture. 05:45 You got a paper cut or you nick yourself with a knife in the kitchen because whatever you're cutting carrots, and when you do, you cut yourself, you gotta stop that bleeding, don't you? Well, you have the process of inflammation that discussion we've had before. 05:59 And that would be neutrophils, and then here you have to stop the bleeding. 06:03 So, obviously platelets. So vasoconstriction is also part of the protocol. 06:08 Remember that beads that I showed you in the previous discussion? Those beads represent a fibrinogen. 06:15 Those fibrinogen then bind to particular receptor on the platelet. 06:20 The name of those receptors are glycoprotein IIb/IIIa. 06:25 Now, how important are these receptors? Oh, my goodness, really important. 06:29 So, by the time we've gone through the normal, and then we start integrating our pathology, and start integrating our pharmacology. 06:38 Then you'll have a firm understanding of these glycoprotein, so GP stands for glycoprotein. 06:42 For example, a condition in which you're missing glycoprotein Ib is called Bernard-Soulier. 06:50 A condition in which you're missing glycoprotein IIb/IIIa, is called Glanzmann's thrombasthenia. 06:56 Or management, pharmacology. A particular drug that is a monoclonal antibody, Fab fragment that targets that glycoprotein IIb -- IIb/IIIa, you must know, that's called abciximab, isn't it? These are things to come, but I'm just trying to give you a little bits of appetizers so that you'll know is to why it's important. 07:18 Ultimately, we need to make sure that the platelet has now come together, and you form, what kind of plug again? Temporary. Why do we say temporary? Because the fibrin is in the form of fibrinogen. 07:30 We haven't cleaved it yet. 07:32 We haven't brought in our discussion of coagulation factors. 07:35 The only thing we've discussed so far is the activation of platelet in forming a temporary hemostatic plug. 07:41 Let's take a look at this picture now in greater detail. 07:45 So, where we left off was where Von Willebrand factor was being expressed by the endothelial cell. Disrupted endothelial surface. 07:53 This was a ligand that bound to which receptor, please? Glycoprotein Ib. Memorize that. 08:01 This process is called what? Is this aggregation or adhesion? That's important. Is it adhesion? The platelet firmly -- not firmly, but it is adhering to the sub-endothelial collagen, via Von Willebrand factor. 08:18 Next, you see the beads again. These beads are the fibrinogen, -ogen means what to you? Weak. If fibrinogen binds to, what receptors? Oh, glycoprotein IIb/IIIa, you see that? Also, very importantly that glycoprotein IIb/IIIa receptor was being expressed by the platelet with the help of whom? ADP. 08:48 Why is that important? Oh, how about some drugs called clopidogrel, prasugrel. 08:54 You know about those drugs. 08:56 You may have heard of trade name, called Plavix and such. 09:01 The point is these are drugs that will then inhibit ADP. 09:05 Therefore not release or express IIb/IIIa, and therefore, you would not be able to then bind the fibrinogen with the other platelet. 09:15 In other words, you wouldn't be able to properly aggregate or maybe perhaps you're deficient of IIb/IIIa. 09:22 And that would be something Glanzmann's thrombasthenia, or maybe, maybe there is a type 2 hypersensitivity reaction in which a patient developed these auto-antibodies of IgG type. 09:34 Which were then attacking IIb/IIIa. 09:35 You see, what I'm trying to get at? You must memorize at this point that IIb/IIIa is the receptor responsible for aggregation. 09:43 Now, ultimately as we move forward, we'll talk about that coagulation cascade. 09:49 We're then going to bring in the thrombin. 09:52 You see that thrombin, that's factor II. Now, big picture. 09:56 Please close your eyes and think about factor II. 09:59 Factor II is activated by the combination or the convergence of both, what's known as the extrinsic and the intrinsic branch of the coagulation cascade, which we haven't discussed yet. 10:11 And ultimately the thrombin will take the -ogen and cleave it off the fibrinogen to form a stable fibrin clot, as we shall see.
About the Lecture
The lecture Normal Hemostasis by Carlo Raj, MD is from the course Hemostasis: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is associated with immature platelets?
- Megakaryocyte
- Reticulocyte
- Myelocyte
- Promyelocyte
- Megalocyte
Which of the following is NOT a typical step in hemostasis?
- Vasodilation
- Epithelial cell damage
- Von Willebrand factor binding to factor VIII
- Platelet adhesion to collagen
- Adenosine diphosphate release by platelets
Which of the following is NOT a component of hemostasis?
- Activation of protein C and S
- Conversion of prothrombin to thrombin
- Conversion of fibrinogen to fibrin
- Platelet activation
- Vasoconstriction
Which of the following receptors binds von Willebrand factor, mainly allowing platelet adhesion at sites of vascular injury and its deficiency leads to Bernard-Soulier syndrome?
- Glycoprotein Ib
- Glycoprotein IIb/IIIa
- Glycoprotein IIIa
- Glycoprotein IIb
- Glycoprotein IIa
Which of the following is an important receptor in platelet activation and a target of several drugs including abciximab, eptifibatide, and tirofiban?
- GpIIb/IIIa
- GpIIIb/IIa
- GpIIb
- GpIIIa
- GpIIa/IIIb
Customer reviews
3,6 of 5 stars
| 5 Stars |
|
7 |
| 4 Stars |
|
1 |
| 3 Stars |
|
2 |
| 2 Stars |
|
1 |
| 1 Star |
|
3 |
The lower reviews than normal kept me from watching Dr. Raj, he is stellar.
I love Dr. Raj's style of explanation. Excellent as always.
speech not fluent and hard to listen to. too basic and not useful
...I don’t believe his accent isn’t hard to understand? Very concise and straight to the point. Helped me understand hemodynamics foundation much better than most lectured videos. Thank you Dr. Raj !