Playlist
Show Playlist
Hide Playlist
Thalassemia – Red Cell Disorders
-
Slides Disorders of red cells.pdf
-
Download Lecture Overview
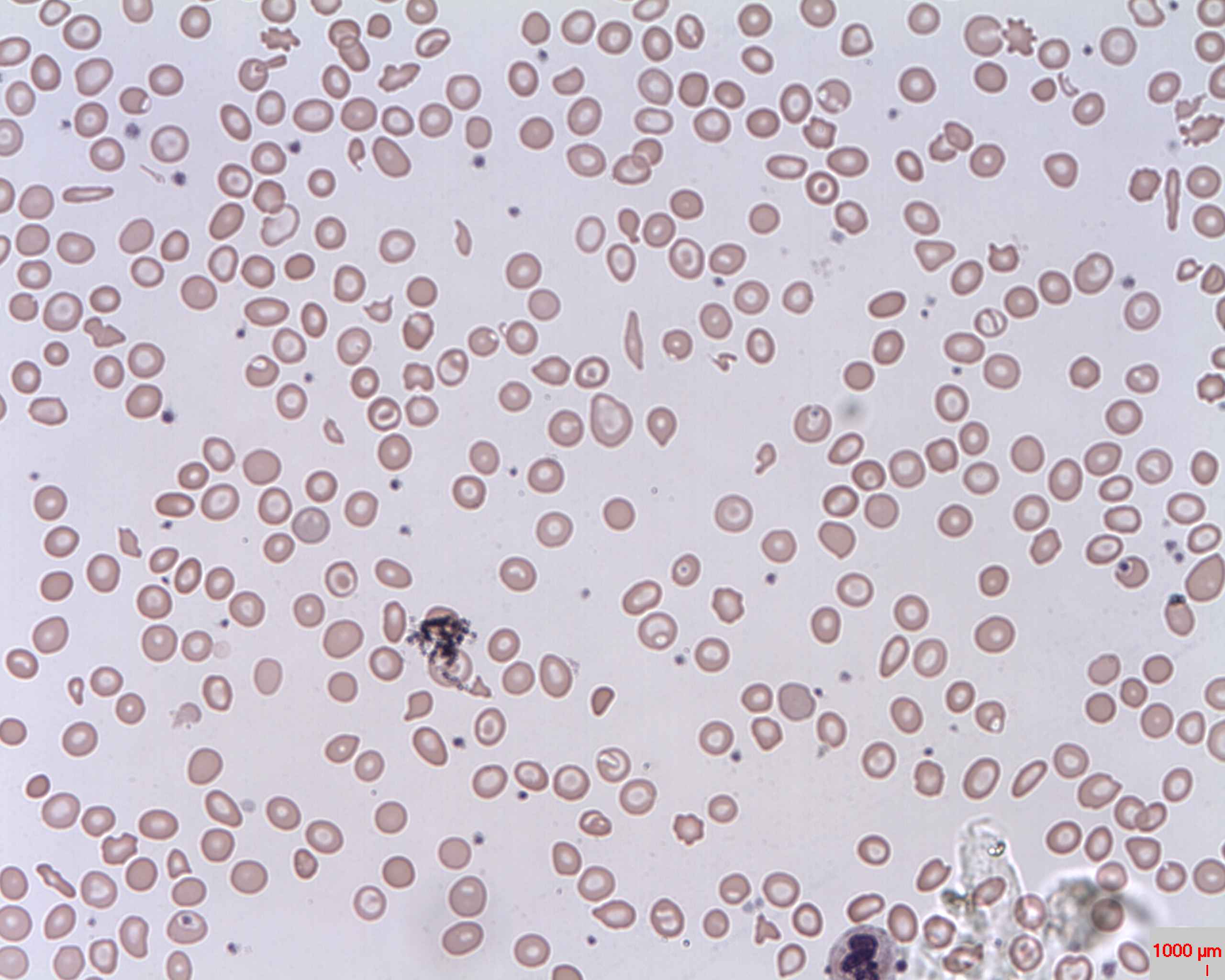
00:02 The second major cause of microcytic anaemia is thalassaemia, the word itself is extraordinary comes from the Greek the sea and when Greek soldiers came back after the wars, they look to the sea thalasses and that is the thing they said. Thalassaemia gets its name because it was common in the Mediterranean. It is due to an imbalance in the production of alpha or beta globin. You need to make equivalent amounts of alpha globin or beta-globin make adult haemoglobin. Alpha-thalassaemia results from a deficiency of alpha-chains. 00:48 Beta-thalassaemia results from a deficiency of beta-chains and treatment if required is with a blood transfusion, which can replace the blood. Now on the right we have an example of electrophoresis of haemoglobin and this electrophoresis allows us to identify different subsets of globin. So if you look on the left of the normal, you will see haemoglobin A is dominant. That is alpha-2, beta-2. 01:21 That is the type of haemoglobin in most adults in the world. Below that is a small amount of haemoglobin F, alpha with gamma and a small amount of A2 alpha with delta chains. 01:38 Now if you look next to that, there is a patient with the beta-thalassemia trait. That means they are lacking one beta globin genes and they are still making beta chains, but the balance between too much alpha and too little beta is disturbed and you will see that the A band is reduced. What is interesting there is you can see that the haemoglobin A2 is slightly increased. I mentioned that because that is a very useful diagnostic test. 02:07 If you have somebody, you have small red cells and you think they may have a beta-thalassaemia trait, then measure haemoglobin A2 and it will be slightly increased. Just to the right of them is somebody with a most severe form of beta-thalassaemia and you can see that the A-band now is very thin. There is still some production of beta globin clearly, but it is very small. And here when I see more production of haemoglobin F, which is useful and can help to provide oxygenation of tissues, but it is not as effective in an adult as haemoglobin A. Finally on the right, there is an example of an alpha-thalassaemia and this is haemoglobin H disease. It is quite a severe form of alpha-thalassaemia. 02:57 Still as haemoglobin A so there is some alpha globin production, but not enough and some of the beta chains are precipitating out has haemoglobin H at the top. Noticed that haemoglobin A2 is not increased enough of thalassaemia. So we do not have an easy test for milder forms of this disorder. Now if the patient has severe thalassaemia, they will be chronically and severely anaemic. The treatment as I mentioned can be blood transfusions. But if that is not done to an adequate level, the patient can be chronically anaemic and that can lead to massive expansion of haemopoiesis within the bone marrow. The bone marrow tries to expand to make more red cells and the characteristic x-ray although now thankfully very rarely seen is this the skull x-ray showing 'hair on end' appearance and that is due to the expansion of the haemopoietic tissue within the skull in this patient who has inadequately transfused thalassaemia. Although transfusions are effective one of the problems is that they have a lot of iron in every blood transfusion, 200 mg and so you must remove the iron through chelation that can be given by deferoxamine subcutaneous injections or through oral tablets.
About the Lecture
The lecture Thalassemia – Red Cell Disorders by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
Which of the following statements about thalassemia is FALSE ?
- Beta chains are overproduced in beta-thalassemia
- It is a major cause of microcytic anemia
- It is due to an imbalance in the production of alpha and beta globin chains
- Treatment, where required, is through blood transfusion
- Electrophoresis is useful in diagnosis
Which of the following is found in higher amounts in beta-thalassemia major?
- Hb F
- Hb A1C
- Hb H
- Hb delta
- Hb A
Which of the following conditions will result in a mild increase in HbA2, mild decrease in HbA1, a normal fetal hemoglobin, and absent Hb H on electrophoresis ?
- Beta-thalassemia trait
- Beta-thalassemia major
- Alpha-thalassemia
- Normal hemoglobin
- Hb H disease
What is the characteristic radiological sign of thalassemia on skull X-Ray?
- Hair on end appearance
- Punched out lesions
- Increased radiolucency in the frontal sinus area
- Increase in the size of the width of the sutures
- Marbelling and radiodense areas within the skull
What is the common complication of treatment of thalassemia?
- Iron overload
- Iron deficiency Anemia
- Copper deficiency
- Zinc increase
- Copper overload
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent lecture and I really enjoy it and it is a useful resource for medical student like me. I have a high probability that I will recommend it to a friend.
conceptual... awesome...appreciated...i liked it very much...my concepts are cleared..thanks