Playlist
Show Playlist
Hide Playlist
Chronic Pelvic Pain
-
Slides Chronic Pelvic Pain.pdf
-
Download Lecture Overview
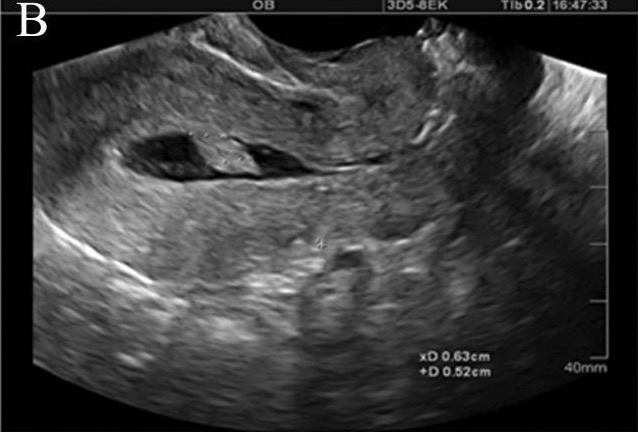
00:01 Hello. In this lecture series, we'll be going over chronic pelvic pain. What is chronic pelvic pain? How long do you have to have pelvic pain before it’s considered chronic? I’ll give you a second to answer that. Well, if you said I don’t know then you’d be right. It’s yet to be defined. 00:30 Chronic pelvic pain is defined as pain symptoms perceived to originate from pelvic organs or structures. 00:37 It typically last more than six months it's often associated with negative cognitive, behavioral, sexual and emotional consequences. 00:47 Pelvic pain can present symptoms suggestive of urinary tract, sexual bowel, pelvic floor, myofascial or gynecological dysfunction. 00:59 No definition is universally accepted. However, many investigators define chronic pelvic pain as: noncyclic pain that persists for six or more months, pain that localizes to the anatomic pelvis, and pain sufficiently severe to cause functional disability or lead to medical intervention. 01:20 Chronic pelvic pain is a very common GYN problem. About 15% of reproductive-aged women report that they have chronic pelvic pain. Chronic pelvic pain falls within a broad spectrum of causes. 01:37 However, endometriosis, symptomatic fibroids or leiomyomas, and IBS are very often diagnosed. 01:45 Endometriosis is a frequent cause, but typically is also associated with cyclical symptoms. 01:51 That means symptoms that occur with your menses. Chronic pelvic pain and sexual abuse are strongly associated. Don't forget to screen for history of sexual abuse. 02:03 Chronic pelvic pain unfortunately can change the posture of a patient. Abnormal posture looks like this. 02:11 However, a patient who might have some pain may have some mark of lordosis. 02:17 They can also have kyphosis as well. Concurrent lordosis and kyphosis are common postural changes associated with chronic pelvic pain. Let’s now review what you might find on history and physical exam. 02:34 More than with any other gynecologic problem, a detailed history and physical exam are extremely important to determine the diagnosis. A pelvic pain questionnaire can be used initially to obtain information. In a woman with chronic pain, even a routine examination can be extremely painful and distressing. Therefore, the examination should be slow in relaxed environment with you explaining each step to her before it occurs. 03:06 Moreover, a patient is reassured if she knows that she can halt the examination at any time. 03:12 Let’s now talk about how to do a physical exam on a patient, any patient that’s a GYN patient but specifically a patient who has chronic pelvic pain. For a bimanual exam, you’re going to need two hands. 03:25 Just remember that. Pain elicited under the urethra may indicate a urethral diverticulum. 03:31 That can be a cause of chronic pelvic pain. Also, you can have pain with the anterior vagina. 03:38 This can reflect pain in the bladder maybe from interstitial cystitis. A large uterus may suggest fibroids. 03:46 But a globular uterus may also be consistent with adenomyosis. For more information about fibroids and adenomyosis, check out the AUB lecture. Immobility may actually be a result of scarring or adhesion formation. Tenderness may reflect endometriosis, diverticular disease of the bowel, or pelvic congestion. Again, in the diagnosis of chronic pelvic pain, you should have a urinalysis to rule out any type of infection in the bladder. You should also obtain a TSH or thyroid-stimulating hormone to make sure that that’s not a cause. 04:26 Transvaginal ultrasound with Doppler is also important in the diagnostic evaluation. 04:32 Consider a fasting glucose to rule out any diabetic neuropathic pain. The management of chronic pain is based on the cause. If you identify a pathology then treatment is dictated by the diagnosis. 04:47 If no pathology is identified then treatment is directed toward the dominant symptom. 04:53 Endometriosis is also a common cause of chronic pelvic pain. The endometriotic implants are actually supported by estrogen. So, if you can suppress sex steroid hormones then you can actually help improve the symptoms associated with estrogen supporting the endometrial implants. This can be done with oral contraceptives, GnRH agonists, progestins, and certain androgens. Thank you for listening and good luck on your exam.
About the Lecture
The lecture Chronic Pelvic Pain by Lynae Brayboy, MD is from the course Female Pelvic Medicine.
Included Quiz Questions
Though there is no universally accepted definition, how long must non-cyclic pelvic pain persist to be commonly defined as chronic?
- 6 months
- 4 weeks
- 6 weeks
- 2 months
- 4 months
Which of the following statements regarding chronic pelvic pain is INCORRECT?
- Gynecologic conditions are the only causes of chronic pelvic pain.
- Endometriosis is a frequent cause of chronic pelvic pain.
- Sexual abuse is sometimes associated with chronic pelvic pain.
- Leiomyomas can cause chronic pelvic pain.
- Endometriosis is associated with both chronic and cyclic pain.
What condition is consistent with the finding of a globular uterus palpated on bimanual examination?
- Adenomyosis
- Adhesions
- Endometriosis
- Pelvic congestion
- Diverticular disease
Customer reviews
3,5 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
0 |
Teacher is wonderfully explained the topic. Very practical , clear and concise information
This presentation could use more substance. I wish it was presented better.