Playlist
Show Playlist
Hide Playlist
Overview – Cell Wall Synthesis Inhibitors (Antibiotics)
-
Slides Antimicrobial Pharmacology Overview Cell Wall Synthesis Inhibitors.pdf
-
Download Lecture Overview
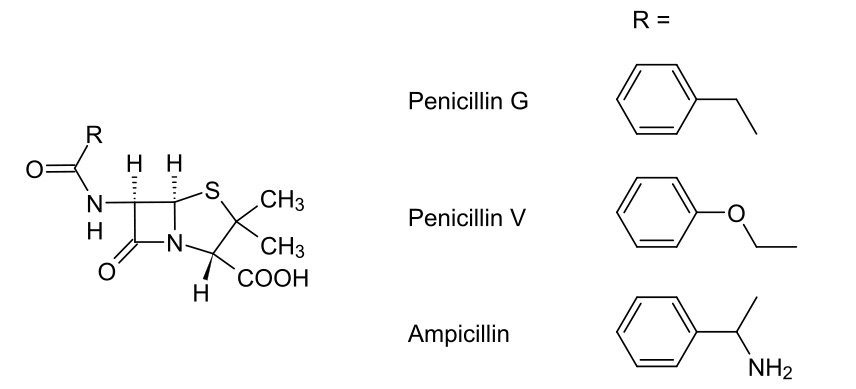
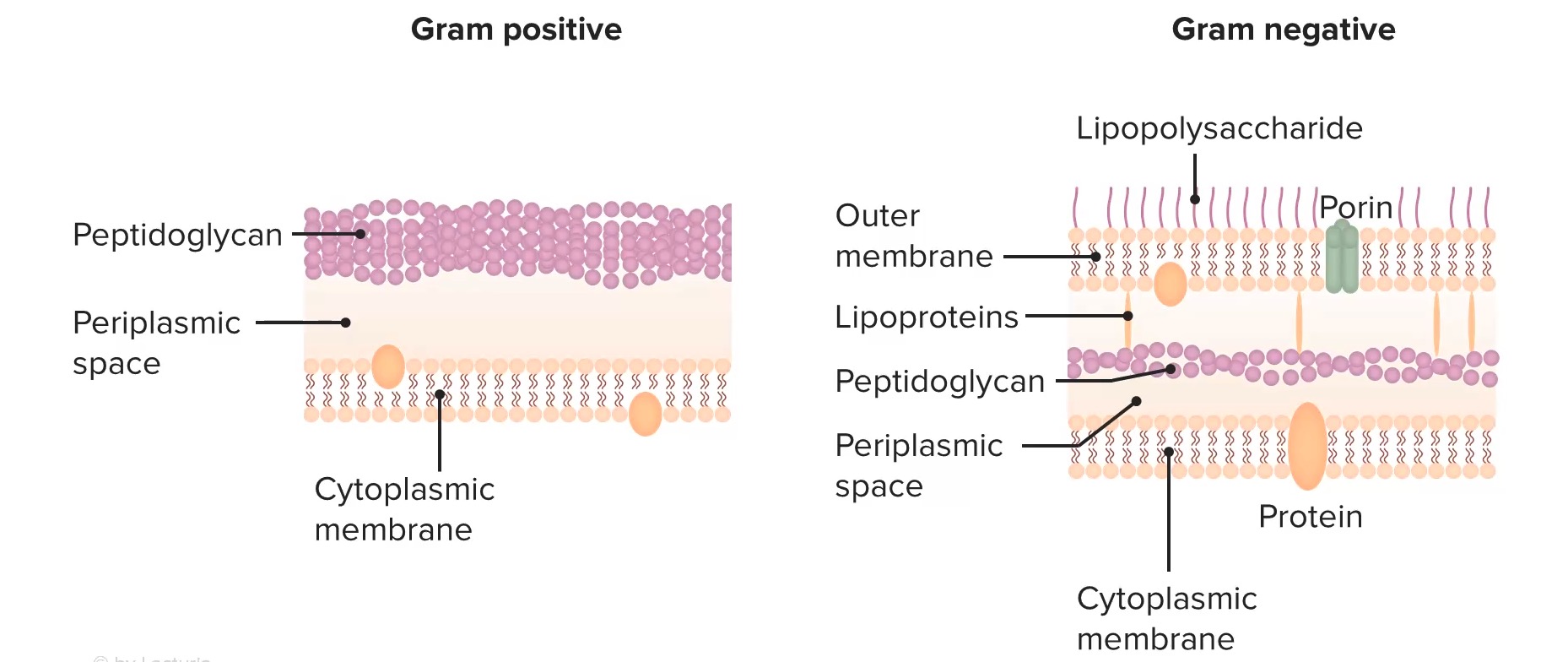
00:01 Welcome to pharmacology by Lecturio. 00:04 I'm Dr. Praveen Shukla, and we're going to talk today about antibacterial agents. 00:09 antibacterial agents fall in several categories. 00:13 We've divided them up here into bacterial cell wall inhibitors, bacterial protein synthesis inhibitors, agents that are acting against DNA and folic acid, and the anti-mycobacterial agents. 00:25 To start off with, let's look at the bacterial cell wall synthesis inhibitors. 00:29 We divide these up into several classes. 00:32 We have the oldest of the group, which are the penicillins, cephalosporins, the penems and other miscellaneous agents. 00:39 How is it that we build a cell wall? Well, cell wall synthesis in the bacteria starts with two major proteins. 00:48 The first one is N-acetylmuramic acid. 00:51 The second is N-acetylglucosamine. 00:53 We'll call them NAM and NAG just to make things a little simple. 00:57 Now they get joined together like cars on a train. 01:00 So there's a very long chain of these NAM and NAG particles that make up a train. 01:05 In order to make a wall, we need two trains bound together. 01:10 So what we do is we take two chains, chains of amino acids, and we lashed them together. 01:15 Now right now when you look at them in the picture here, it's just a loose knot. 01:20 But what we're going to do is we're going to use a thing called a penicillin-binding protein. 01:25 Now this protein comes along, cleaves off two of the end units, binds them together tightly, and keeps on doing that over and over again, until you have a very long set of two trains hooked together to make a strong cell wall for the bacteria. 01:44 How do we stop the production of this wall? We use something called a beta-lactam antibiotic. 01:50 Now this beta-lactam ring binds to the penicillin binding protein and prevents it from doing its job. 01:57 What ends up happening is you have a wall that isn't being built. 02:02 The beta lactam antibiotic binds to the penicillin binding protein, and it prevents the cross linking of NAM and NAG chains to each other. 02:14 Well, what does that do to an existing bacteria? Nothing, the cell wall was already built. 02:20 What really matters though, is when the cell wall, pardon me, when the cell wants to start replicating itself. 02:26 So as the cell stretches and decides to divide, the dividing cell can't build new cell wall. 02:35 What you end up with is the existing bacteria and something else called a spheroplast. 02:41 Well, what's a spheroplast? Essentially a spheroplast is a bacteria without a cell wall. 02:46 Now these spheroplasts are essentially useless, they can't do what they're supposed to do, which is infect the body. 02:53 So bacteria that attempt to grow and divide in the presence of penicillin, end up shedding their cell walls and they stop dividing. 03:03 The remaining spheroplasts auto catalyze, they break down on their own and they die. 03:09 How is it that we get resistance to these antibiotics? There's three major ways. 03:14 First, there's beta-lactamase-mediated resistance. 03:18 Now, what is beta lactamase-mediated resistance? Beta lactamase is our enzymes within the bacteria itself that actually break down that beta-lactam ring. 03:28 If you think about it, it's kind of like warfare. 03:31 The mechanism of most types of resistance occurs through beta lactamases. 03:36 They break down the very antibiotic that's supposed to be killing them. 03:40 This will affect many antibiotics that have a beta-lactam ring. 03:44 So this includes the penicillins, cephalosporins, some of the cephamycins, and other carbapenems. 03:52 So what is a beta-lactamase? Well, you have here a picture of a beta-lactamase. 03:58 It's a beautiful illustration, you can see how complex a structure this actually is. 04:03 They're also called penicillinases or cephalosporinases. 04:07 But I would just like you to use the term beta-lactamase, because it really reminds us of where these drugs are acting. 04:14 Now they're produced by gram-positive organisms, but they also can be produced by gram-negative organisms. 04:20 They're usually secreted and may be secreted in response to the presence of an antibiotic. 04:26 So sometimes beta lactamase-mediated resistance isn't really obvious until you actually expose the organism to an antibiotic. 04:34 And then all of a sudden you realize, oh my gosh, this, this particular organism is resistant. 04:39 This has become a huge problem now with cephalosporins. 04:42 And of course, you all probably know already that we use cephalosporins much more than we have been using penicillins. 04:49 Now, sometimes the resistance with cephalosporins is a little bit different. 04:54 This is a new chromosomal- mediated mechanism. 04:57 It's a new threat that we're starting to see. 04:59 We started seeing at around 2016, and over the last several years has become more and more prominent. 05:06 We're also seeing now beta-lactamase-mediated resistance with some of the cephamycins. 05:11 So this is something that we're seeing more and more over time, it's going to be more and more important as practice goes on. 05:19 Now, what do we do about these beta-lactamases? Well, specifically with the penicillin based beta-lactamases, we can counter it with certain types of inhibitors of these enzymes. 05:30 One of them and probably the most commonly known is clavulanic acid. 05:34 So, for example, we will pair clavulanic acid with amoxicillin so that we have a combination of medications that's relatively beta-lactamases resistant. 05:44 Sulfabactam is another one, we put it together with ampicillin, or Tazobactam, we'll put together with piperacillin as combination products, And they're often sold as combination products on the market. 05:57 The other way that we develop resistance to the beta lactam antibiotics are penicillin-binding protein mediated resistance mechanisms. 06:06 So this is actually a lot simpler than it sounds. 06:09 Basically, we have a penicillin binding protein that is resistant to the effects of the beta lactam. 06:17 Now, how does that work? Now, if you look, here, we have a picture of naked DNA from the resistant bacteria. 06:23 That naked DNA actually gets incorporated into the cell. 06:28 The host DNA is now changed. 06:30 Okay, when that host DNA produces a new penicillin binding protein, it's slightly different. 06:37 And it's different enough that it is resistant to the beta lactam, but is still able to produce a cell wall. 06:44 So you can actually have transmission of DNA from one bacteria to another that provides the resistance, and you produce new penicillin binding proteins. 06:55 This gives you a reduced affinity to the new beta-lactam antibiotic or to the old beta-lactam antibiotic. 07:01 And that's how these types of resistances spread. 07:05 The third type of resistance is called porin-mediated resistance. 07:10 And it sounds exactly like it is. 07:13 So porins are basically pores. 07:15 They're water-filled channels. 07:17 Here's a beautiful illustration of a porin. 07:20 Now a porin is a tubular structure that is seen in the cell walls. 07:25 The antibiotics travel through porins to get inside the bacteria. 07:29 But if you have a bacteria, for example, that adapts and makes fewer porins, you'll have less ability for the antibiotic to get in. 07:38 And we see that actually in Pseudomonas all the time. 07:41 Pseudomonas is very commonly recognized as one of the agents that has porin-mediated resistance. 07:47 Now I'll give you a trick for the exams. 07:50 Porin-mediated, Pseudomonas both start with P. 07:52 And this is something that got me through at least one of the questions on my exams. 07:56 So try to remember, porin, Pseudomonas makes things a little bit easier to remember.
About the Lecture
The lecture Overview – Cell Wall Synthesis Inhibitors (Antibiotics) by Pravin Shukle, MD is from the course Antimicrobial Pharmacology.
Included Quiz Questions
Regarding cephalosporins, which statement is TRUE?
- They inhibit the synthesis of the bacterial cell wall.
- They are used as fungal and bactericidal drugs.
- They inhibit protein synthesis.
- They inhibit dihydropteroate synthase.
- They are more susceptible to penicillinase than other penicillins.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
hello Lecturio Im from Philippines Im so happy that I came to find this very knowledgeable site where I can learn sruffs related to my course which is Pharmacy.