Playlist
Show Playlist
Hide Playlist
Example Cases
-
Slides 01 PrinciplesandApplicationtoUSMLE IntroductiontoFamilyMedicine.pdf
-
Download Lecture Overview
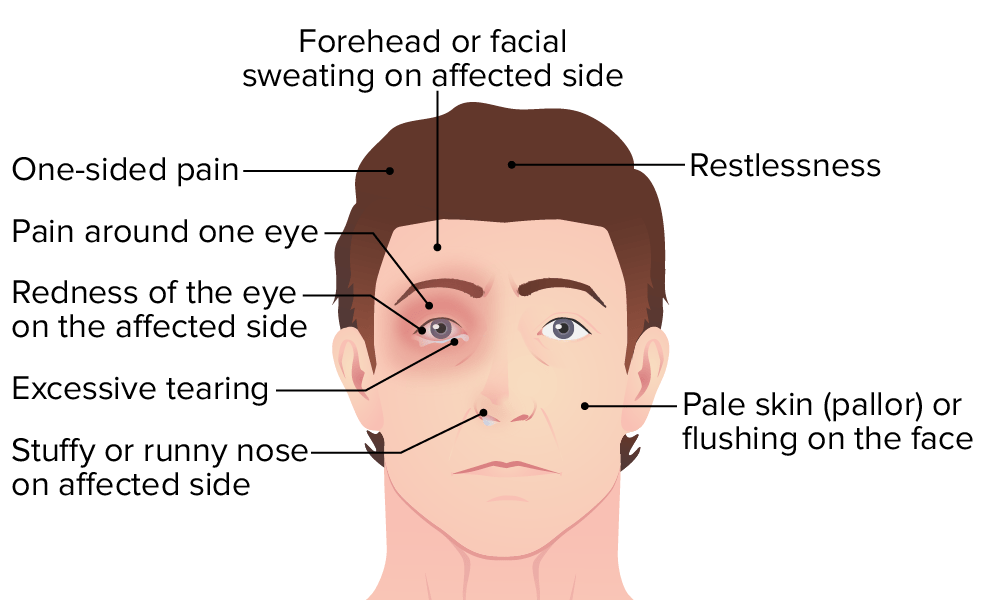
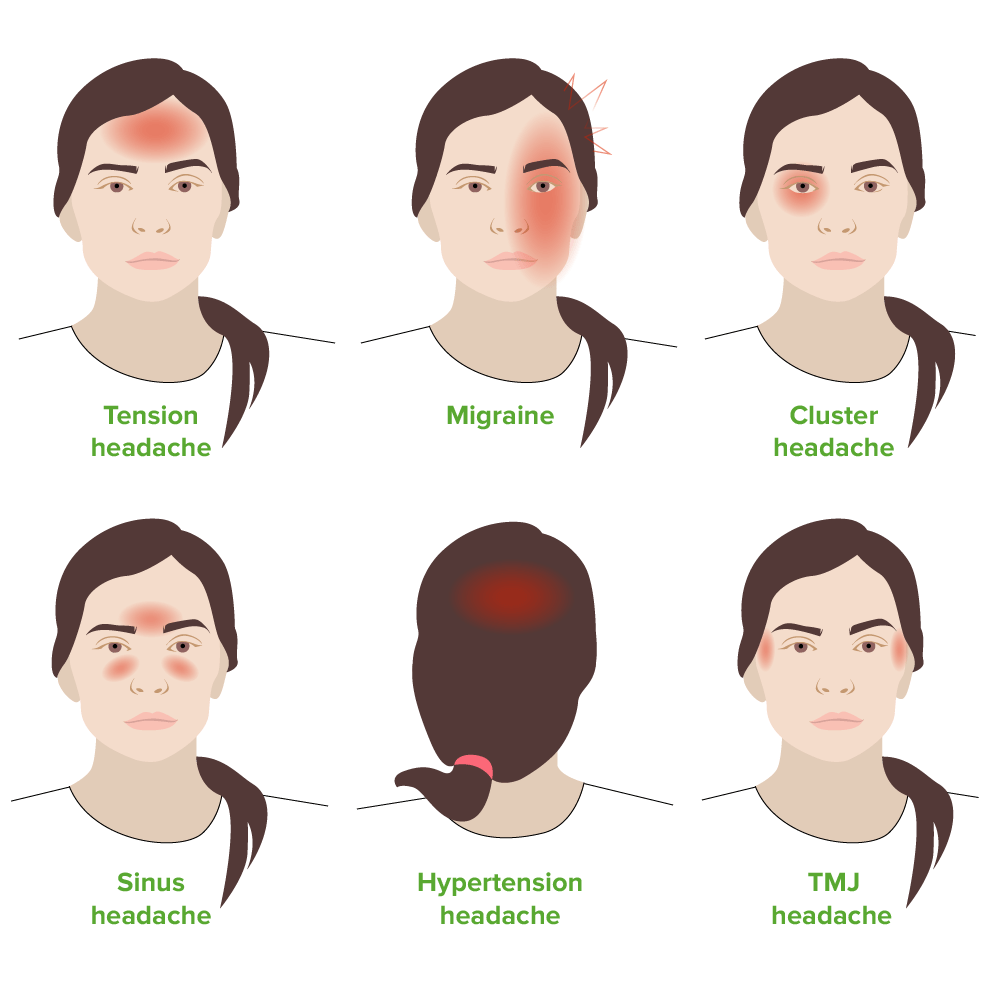
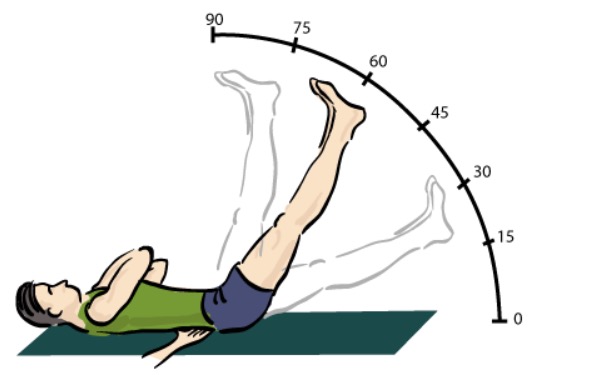
00:01 All right, so let's do some cases, because, you know, I'm sure you are wondering, how are we gonna tie this back to USMLE exams? We can, don't worry. 00:11 I'm gonna talk about some of the-- how these principles actually play out in case scenarios which are those case stems are what you are going to see on USMLE, and how you're gonna answer in an evidence-based and empathic way for some of these issues. 00:25 So I've got a-55-year-old man, history of hypertension, type 2 diabetes, hyperlipidemia, constant dull pain over his left chest for two weeks. 00:34 A little bit more history, it does not radiate and it's not associated with other complaint, such as shortness of breath or nausea and vomiting. 00:43 His vital signs and his physical examination are normal. 00:45 What's the next best step in this case? Is it A. Inquire whether the pain changes with physical activity. 00:51 B. Order an electrocardiogram straight away. 00:54 C. Nuclear stress study. 00:55 or D. Serum D-dimer level. 00:58 And the answer is A. 01:02 Now, we have some history here, and it's interesting because it's a man who's got some chest pain. 01:11 He's got all the major cardiovascular risk factors in terms of chronic illness, but it's a constant dull pain for two weeks. 01:20 That doesn't tell me that this is necessarily angina which should come and go. 01:24 And of course, the critical issue is, does it come and go and get worse with exercise and that's why the answer is A? It also doesn't radiate nor associate with other complaints that you might see with angina and shortness of breath, nausea or vomiting, and his physical exams are all normal. 01:41 So the next best step in this case is, let's get more history. 01:46 We are a history-driven specialty. 01:48 If you wanna be patient-centered. 01:50 Does he need an electrocardiogram, option B. 01:53 Probably, but not before we get more history, because there is a lot to be left to be discovered in this case just with history alone and for restratification. 02:03 And certainly, I'd want that stratification done before I order either a nuclear stress study to check his coronary arteries or a serum D-dimer level, because I'm worried about pulmonary embolism which this sounds nothing like a pulmonary embolism. 02:17 So that's some of the principles playing out here is that in general, if you think about these questions and case stems from a family medicine perspective, getting more history of observation are generally gonna be more profitable answers for you, and it's evidence-based care as well. 02:35 All right, let's do another one. 02:37 How about low back pain? Sixty two-year-old woman complains of low back pain for three weeks in duration. 02:42 She has occasional radiation of the pain down her right posterior thigh. 02:47 Over-the-counter analgesics and stretching have been moderately helpful for the pain, and her physical examination is unremarkable. 02:55 So a limited history, limited case stem. 02:58 What should you do for this patient now? A. Order plain radiography of the lumbar spine. 03:03 B. Order an MRI of the lumbar spine. 03:05 C. Prescribe a muscle relaxant or D. Continue current therapy and consider a referral to physical therapy. 03:11 So let's see. 03:15 Thinking like a family doctor. 03:18 The answer is D. 03:20 So she's getting some moderately relief, the pain has being going on for three weeks which is a good duration, but we know that the vast majority of low back pain, even when it involves siatica, improves significantly within two months. 03:36 And so therefore, probably just more time, possibly with the addition of an evidence-based treatment like physical therapy would be the best option for her. 03:47 It's too early to think about doing imaging. 03:51 I only would think about imaging for somebody with back pain when I'm really thinking about doing something more interventional like referring them on for injection therapy or even surgery. 04:02 And so if she has no red flags on physical examination, no reason to order imaging at this time. 04:09 Muscle relaxants, they are highly sedating, they don't really have a strong therapeutic indication. 04:17 Therefore, I would probably stick with what she's doing now, because it is moderately successful, and the physical therapy might help as well. 04:24 All right, let's do one more case. 04:26 I've got a-40-year-old woman with lots of complains. 04:29 Headache, lightheadedness, blurry of vision, dull abdominal pain, pedal edema, and generalized weakness, all for two weeks. 04:38 So just with that brief history alone, and your mind should be swimming now trying to put all of those complains together. 04:46 If it's swimming, that's good. 04:48 Mine is swimming, too. 04:49 Which of the following interventions is most likely to be helpful in this case? A. MRI of the brain. 04:54 B. An erythrocyte sedimentation rate or SED rate. 04:58 C. An evaluation for psychosocial stressors. 05:00 or D. Thyroid function testing. 05:03 We're you able to draw a singular diagnosis that can link all of those different complains together? I think it's a real challenge. 05:14 I mean, there are certainly are some, you know, rare types of problems that could link all of those together. 05:23 Multiple sclerosis, but I mean, still can't explain the edema. 05:28 Porphyria. 05:30 So, but these are so rare, especially in a-40-year-old, you know assuming, previously healthy woman. 05:38 That I would really start to wonder, you know, maybe there's an insighting event that brought all of these various complains on at once, and maybe it's just a reaction of stress, maybe it's somatization disorder. 05:51 That's gonna to be the most likely when you have desperate complains like this. 05:55 And this is where the biopsychosocial model of health care really helps me out. 05:59 I'm not gonna rush to do testing, whether it's something specific, like an MRI of the brain, or something that's very vague, and you're just trying to find some kind of inflammation with an erythrocytes sedimentation rate. 06:12 Get more history here, and maybe this patient is about to lose her job, maybe she is worried about a family member or there's been a family crisis. 06:23 There's a million things that can promote this spectrum of symptoms and do so acutely. 06:31 And then working through that, once you find that there is indeed some serious stressor in this patient, working through that is gonna be a lot more effective than doing blind testing or blind treatment as well. 06:43 So with that, I hope that those cases gave you an understanding of how we apply some of those principles of Family Medicine to our practice on an every day level, and can help you to provide better answers, more correct answers on your USMLE exam. 07:01 Thanks.
About the Lecture
The lecture Example Cases by Charles Vega, MD is from the course Introduction to Family Medicine. It contains the following chapters:
- Introduction to Family Medicine: Cases
- Low Back Pain
- Headaches and Lightheadedness
Included Quiz Questions
A mom brings in her 7-year-old boy for frequent "bellyaches" that have sent him home from school several times a week for the past 2 weeks. When at home and after a couples hours, he seems more comfortable and playful. However, by the next day his discomfort appears to reoccur. He has less of an appetite in the mornings, but snacks well when brought home from school and usually eats his dinner. He typically has daily or every-other-day bowel movements that appear normal. What is the best next step in diagnosis?
- Take a psychosocial history
- Test for occult blood in stool
- Test for stool ova and parasites
- Obtain an abdominal ultrasound examination
- Refer to a gastroenterologist
A previously healthy 31-year-old woman presents to your office because of stiffness in both her hands, fingers, wrists, and ankles for several weeks. Her symptoms are worse in the morning but improve significantly by noon. She also complains of dry eyes and mouth without any changes to her diet or water intake. She feels tired with little daily activity and cannot complete her work as she used to. She is single and is not in any new relationships. She has a strong family history of rheumatoid arthritis. Which of the following is the most appropriate next step?
- Performing physical examination, creating a differential and management plan, and possibly referring to a rheumatologist
- Obtaining rheumatologic tests
- Screening for depression
- Referring to a psychologist
- Performing bilateral wrist X-rays
A 26-year-old woman comes to the physician because of frequent diarrhea and abdominal cramps over the past six months. She denies blood or mucous in her stools, changes in her diet or appetite, or weight loss. She has not traveled over the past year. She has no history of a serious illness and takes no medications. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- Irritable bowel syndrome
- Crohn's disease
- Ulcerative colitis
- Secretory diarrhea
- Osmotic diarrhea
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
These videos are very efficient and useful for step 2 and so many other medical exams too.... Want to have some more videos from other clinical subjects ..